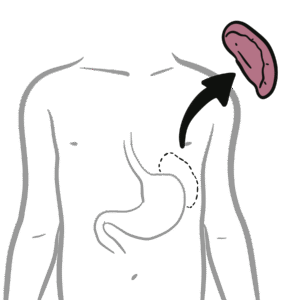
0:00 Ray's syndrome is a rare but potentially fatal condition that primarily affects 0:09 children 0:09 and adolescents recovering from a viral infection, most commonly influenza or 0:14 varicella, which 0:15 is chickenpox. 0:16 There is a strong association with aspirin use during these illnesses and the 0:21 development 0:22 of Ray's syndrome. 0:24 Ray's syndrome is characterized by acute end care fallopathy and hepatic 0:29 dysfunction without 0:31 evidence of inflammation. 0:33 Although its incidence has dramatically declined with increased public 0:37 awareness about the 0:38 association with aspirin use, Ray's syndrome remains a critical diagnosis due 0:43 to its rapid 0:43 progression and high mortality if untreated. 0:50 Ray's syndrome is now extremely rare, particularly in countries that have 0:53 limited pediatric aspirin 0:55 use, except in specific indications such as in Kawasaki's disease, a disease 1:00 that 1:01 causes inflammation of the blood vessel. 1:04 The incidence peaked during the 1970s and early 1980s but declined sharply 1:10 following public 1:11 health campaigns promoting aspirin avoidance in children, leading to a 1:15 corresponding drop 1:16 in cases. 1:18 Most affected individuals are children between the ages of 5 and 15, with no 1:23 significant 1:23 gender predominance. 1:30 So let's talk about the pathophysiology. 1:33 Now the exact cause of Ray's syndrome is not clear but there is a strong 1:38 association that 1:39 exists between aspirin use during viral illnesses and the development of the 1:44 disease as mentioned. 1:46 It is hypothesized that mitochondrial dysfunction in the liver plays a central 1:52 role, leading 1:53 to impaired fatty acid metabolism, hyper ammonia, cerebral edema and hepatic st 2:01 iotosis without 2:02 inflammation. 2:08 The proposed mechanism in clinical presentation, Ray's syndrome typically 2:12 manifests following 2:13 a prodromal febrile illness such as an upper respiratory tract infection or var 2:18 icella and 2:19 is associated with aspirin treatment. 2:22 The early signs include persistent vomiting, lethargy, irritability, confusion 2:28 and disorientation. 2:29 And the latest signs or stages where you get rapid progression to hepatic 2:36 failure, neurologic 2:38 deterioration, seizures and coma can also occur. 2:44 The syndrome is believed, again to result from the mitochondrial injury, 2:49 particularly 2:49 in the liver, leading to acute hyper ammonia and accumulation of other toxic 2:55 metabolites. 2:57 The severity of the disease correlates closely with a degree of hyper ammonia. 3:02 Liver dysfunction and hyper ammonia contribute significantly to the development 3:07 of cerebral 3:08 edema and increase in intracranial pressure, so brain swelling. 3:15 Mitochondrial damage in endothelial cells and astrocytes within the area may 3:19 also play 3:20 a role in cerebral edema. 3:25 Other findings include serum amino transferase levels that are usually up to 3 3:33 times normal. 3:36 Hypogly levels are markedly increased, while prothrombin time is mildly too 3:42 moderately 3:42 prolonged and serum bilirubin levels typically remain normal. 3:47 Hypoglycemia is also a common finding. 3:49 These are essentially all features of hepatic failure. 3:54 Liver histology reveals hepatocytes with a foamy accumulation of triglycerides. 4:01 Electron microscopy shows the structural alterations in mitochondria. 4:05 Strategies that are similarly observed in the brain, hence the thought that 4:11 there is 4:11 an issue with the mitochondria in the pathophysiology of Ray's syndrome. 4:23 Diagnostic evaluation, so early diagnosis relies on clinical suspicion, 4:28 particularly in children 4:28 presenting with unexplained vomiting and altered mental status after a viral 4:33 illness, especially 4:34 if they've had aspirin. 4:36 Investigations include blood tests which show elevated AST and ALT. 4:42 Ammonia levels are elevated. 4:44 This hypoglycemia, prolonged prothrombin time, or INR, lumbar puncture is 4:49 important to rule 4:49 out infectious encephalitis, and CSF is usually a normal. 4:54 The cerebrospinal fluid is usually normal in Ray's syndrome. 4:58 Neuroimaging such as a CT or MRI of the brain may show cerebral edema, and 5:02 liver biopsy 5:03 as mentioned, will demonstrate micro-vaciculosterosis without inflammation. 5:10 But liver biopsies are rarely done because it's normally diagnosed prior to 5:20 this. 5:22 The management of Ray's syndrome is very important. 5:25 It is a medical emergency and does require intensive care. 5:31 Alternative care is usually done in the intensive care unit because you need to 5:35 manage the cerebral 5:36 edema, elevate the head, hyperventilation, manatol or hypertonic saline is used 5:42 , especially 5:43 if they have raised intracranial pressure, correction of metabolic disturbances 5:48 , so glucose 5:49 to address hypoglycemia, vitamin K or plasma products, if quagulopathy is 5:55 present, and obviously 5:57 avoidance of hepatotoxic drugs because of the liver failure. 6:02 The early recognition and aggressive supportive therapy can significantly 6:07 improve outcomes. 6:08 Public health measures remain the cornerstone of prevention. 6:12 Avoid aspirin in children and adolescents, especially if they're recovering 6:16 from viral 6:17 infections. 6:18 Use alternate anti-pyridics such as paracetamol or ibuprofen unless otherwise 6:24 indicated. 6:28 The prognosis of Ray's syndrome depends on the severity of neurological 6:31 involvement 6:32 at the time of presentation. 6:35 With prompt diagnosis and aggressive management, survival rates exceed 80%, 6:40 however severe 6:41 cases with deep coma or de-seribrate posturing carry a higher risk of death or 6:48 long-term 6:50 neurological sequelae. 6:54 So in conclusion, although Ray's syndrome is now rare, it remains a critical 6:59 diagnosis 7:00 to consider in any child with vomiting and altered mental status after a viral 7:05 illness, 7:06 especially when there is a history of aspirin use. 7:09 Of course, viral encephalitis is one of the primary differentials to think 7:14 about as well. 7:16 Early diagnosis and prompt supportive care are essential for improving survival 7:20 and minimizing 7:22 neurological impairment.