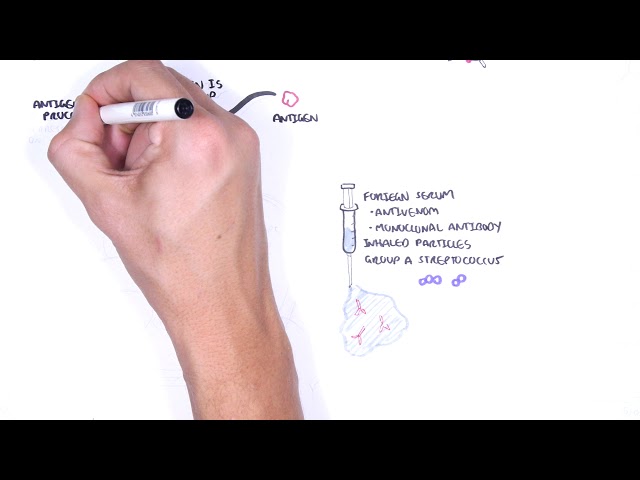
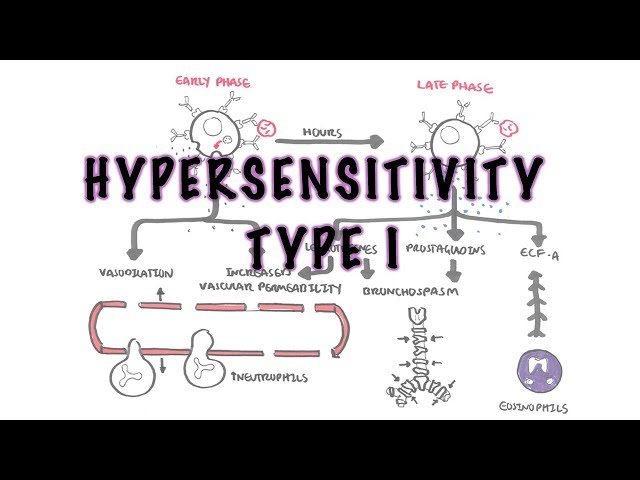
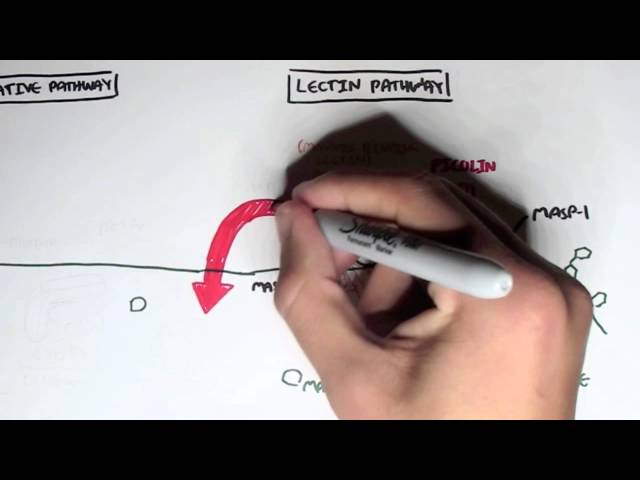
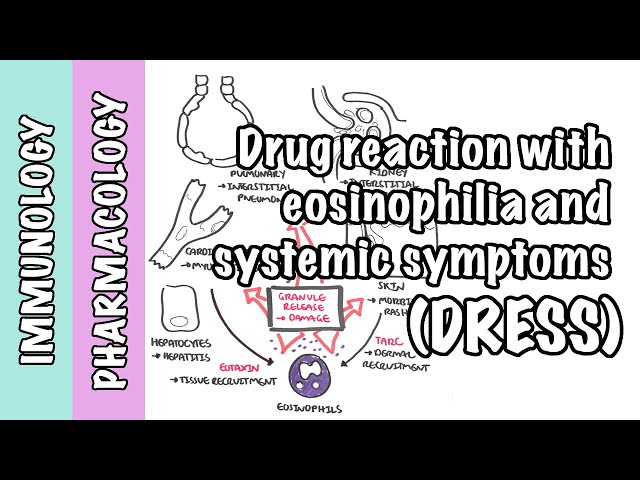
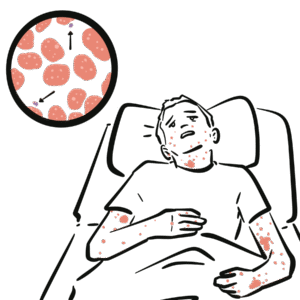
0:00 Hypersensitivity reactions are exaggerated or inappropriate immune response to 0:20 benign 0:21 antigen. 0:22 It is the immune response and not the antigen that is actually harmful. 0:29 An external antigen such as a drug, pollen, or food can elicit an inappropriate 0:35 immune 0:35 response. 0:36 However, an inappropriate immune response to an internal antigen, such as your 0:42 own skin 0:43 or neuron, would be called an autoimmune reaction. 0:48 Hypersensitivity reactions can be the mechanism of diseases in some autoimmune 0:55 reactions. 0:56 Hypersativity reactions are antigen-specific. 1:00 It's antigen-specific because the immune system is educated and primed towards 1:05 the antigen 1:06 after the first exposure. 1:09 In this quick example, first exposure or first contact to an external antigen, 1:14 such 1:15 as a drug, pollen, or food, causes the immune system to sensitize itself 1:21 towards the particular 1:22 antigen. 1:23 In other words, it primes the immune system against that antigen, so when the 1:31 next time 1:32 the antigen comes along, the primed immune system, including the T cells, 1:39 antibodies, 1:40 and neutrophils, they can mount an exaggerated and inappropriate immune 1:46 response, aka a hypersensitivity 1:49 reaction. 1:50 But the immune system can cause hypersensitivity reactions in different ways, 1:56 and that is why 1:57 hypersensitivity reactions can be subdivided into four main types. 2:02 Type 1, type 2, and 3 hypersensitivity reactions are antibody-mediated, whereas 2:08 type 4 is a 2:09 cell-mediated hypersensitivity reaction. 2:15 Let's talk about hypersensitivity type 2 reactions, also known as cytotoxic 2:20 reactions, in where 2:21 antibodies produced, bind directly onto antigens on the surface of plasma 2:27 membranes, and then 2:29 activate the complement response, the complement proteins. 2:34 Complement proteins essentially are circulating proteins that when activated 2:39 lead to an inflammatory 2:41 response against a particular target. 2:45 Hypersensitivity type 2 is an antibody-mediated response against an antigen on 2:52 the surface 2:53 of cell membranes. 2:56 Now this antigen can be, for example, a particular drug such as penicillin, 3:03 hydrochlorothiazides, 3:06 and quinines, which in rare cases can be found on the surface of red blood 3:12 cells and platelets. 3:14 Another example of an antigen could be part of a bacteria. 3:21 Another antigen could be the rhesus antigen, where a rhesus negative person 3:28 will mount an 3:29 antibody response against a rhesus positive red blood cell. 3:36 All of the antibodies produced against these antigens will then activate 3:42 complement systems. 3:45 Please note that all these antigens will be found on the surface of a 3:48 particular cell 3:49 membrane, or a plasma membrane. 3:54 In order to form antibodies in the first place, there must be first contact of 3:58 the antigen 3:59 with the immune system. 4:01 Here the antigen-presenting cell will pick up the antigen, and it can be any 4:05 one of those 4:06 we mentioned earlier. 4:08 The antigen-presenting cell will process and present the antigen then on its 4:13 surface. 4:14 The antigen-presenting cell will travel to nearby lymph nodes, where they will 4:17 interact 4:18 with naive T-helper cells. 4:21 Some naive T-helper cells will be able to bind onto the antigen presented by 4:26 the antigen-presenting 4:27 cell. 4:28 When this happens, the antigen-presenting cell will be able to activate the T- 4:34 cell. 4:35 The activated T-helper cell will then activate specific B-cells. 4:41 The activated B-cell will become plasma cells, and during the whole process 4:45 they will undergo 4:46 class switching, where they change the class of their antibodies. 4:50 So for example here from a immunoglobulin D, IgD antibody, it will become an Ig 4:58 G or IgM 4:59 secreting plasma cell. 5:02 Plasma cells are the cells which produce antibodies, and the antibodies will 5:06 only target 5:06 the specific antigen. 5:09 IgG is a single monomer that circulates in the bloodstream, and IgM is a pent 5:17 ema, 5 antibodies 5:20 bound together, and is usually the first antibody produced against an antigen. 5:27 Both IgG and IgM immunoglobulins can activate a complement system. 5:33 The basic structure of an antibody involves inner heavy chains and outer light 5:40 chains. 5:41 The areas here are the FAB region, which is the antigen-binding fragment region 5:47 that binds 5:48 to antigens, and the bottom part here is the FC region, also known as the 5:55 fragment crystallizable 5:57 region. 5:58 This region actually is able to bind to certain receptors, and the FC region is 6:04 the region 6:05 that is responsible for activating the complement proteins, and we will soon 6:10 see how. 6:11 Again the FAB region binds to specific antigens. 6:20 Examples of hypersensitivity type 2 reactions involve, for example, an IgG 6:26 antibody produced 6:27 against the antibiotic penicillin. 6:33 Now penicillins are able to bind sometimes onto the surface of red blood cells. 6:41 On the rare chance, IgG penicillin antibodies binds to the penicillins via the 6:47 FAB region 6:48 on the cell's surface. 6:55 Once bound, the IgG antibodies activates complement via its FC region. 7:02 Complement activation leads to four main things. 7:05 Number one, it increases inflammatory mediators, and thus inflammatory response 7:12 . 7:12 Number two, it causes obstinization on membrane surface, leading to phagocyt 7:18 osis. 7:19 Number three, complement proteins form the membrane attack complex. 7:24 Which causes essentially the cell to lice. 7:28 And finally, number four, complement proteins can activate natural killer cells 7:32 , which will 7:33 cause the natural killer cell to kill that particular cell. 7:39 Thus, in this scenario, complement activation leads to the red blood cell death 7:46 , or hemolysis, 7:47 resulting in anemia. 7:52 Treatment activation is a bit more complicated, and involves a number of steps. 7:57 In hypersensitivity, the classical pathway of complement activation occurs. 8:06 In the classical pathway, using the same scenario of the red blood cell, what 8:10 happens 8:11 again is IgG, or IgM antibodies, recognize an antigen on the membrane surface 8:17 of a cell 8:18 via its fab region. 8:23 The FC region of the antibody acts as a bridge for the classical complement 8:28 activation pathway. 8:30 Now normally, complement proteins are inactive as they circulate in the body, 8:35 but when cleaved, 8:36 the complement proteins are activated. 8:39 In the classical pathway, the first important product formed by the activation 8:44 of some complement 8:45 proteins is C3 convertase, which is an enzyme. 8:51 C3 convertase is formed and bound to the membrane surface, and its function is 8:57 to cleave and 8:58 activate C3, complement 3, to become C3A and C3B. 9:06 C3A and C3B are active forms of complement 3, and they do separate things. 9:13 C3A is an inflammatory mediator, promoting the inflammatory response. 9:19 C3B obscenizes membrane surface, so it attaches to the membrane surface of the 9:26 cell, for example, 9:27 the red blood cell in this case. 9:32 The obscenized red blood cell is recognized by phagocytes such as neutrophils 9:37 and macrophages 9:38 via complement receptors, and thus it causes phagocytosis and destruction of 9:44 the red blood 9:45 cell. 9:47 C3B, interestingly, can also bind to C3 convertase to form C5 convertase, 9:57 another enzyme, and 9:59 if you haven't guessed it, C5 convertase cleaves and activates complement 5, C5 10:06 , to become 10:07 C5A and C5B. 10:12 C5A and C5B have different functions. 10:16 C5A is an inflammatory mediator, so C3A and C5A essentially increases vascular 10:28 permeability, 10:29 allowing complement proteins to enter the inflamed area, as well as allowing ph 10:34 agocytes 10:35 to enter the area and help engulf opsonized cells, as we have talked about. 10:46 C5B initiates formation of the membrane attack complex, known as MAC for short. 10:53 C5B binds with C6, C7, and C8 complement proteins, which allow formation of a 11:01 channel 11:02 via complement 9 proteins. 11:09 This whole structure is the membrane attack complex, and what it does is that 11:14 it causes 11:15 fluids, it allows fluids to rush inside the cell, causing the cell to lice. 11:22 So the membrane attack complex causes lysis of the cell. 11:31 The complement proteins also, mentioned before, activate natural kilocells. 11:42 Another example of hypersensitivity type 2 is where IgG or IgM antibodies 11:49 against quinines. 11:51 Quinines can attach onto the platelet surface. 11:56 Quinines are molecules important in forming plugs to stop bleeding normally. 12:02 Now antibodies against quinines bind to the quinine on the surface of platelets 12:09 . 12:09 Bound IgG or IgM antibodies activates complement via the FC region of the 12:14 antibodies, as we 12:15 discussed. 12:17 When this happens, you get obstinization and macrophages attacking the plate 12:24 lets, and 12:25 then you also get lysis of the platelets via the membrane attack complex. 12:29 All of this will lead to thrombocytopenia, which is essentially low number of 12:34 platelets 12:35 in the blood. 12:40 Now IgM antibodies against microplasma pneumonia may also form in an acute 12:48 setting, a hypersensitivity 12:51 type 2 reaction. Interestingly, in cold temperatures, these antibodies can 12:56 cross-react with the 12:58 person's own red blood cells, leading to complement activation and hemolysis, 13:04 causing 13:04 anemia. 13:09 Another example of hypersensitivity type 2 are antibodies produced during 13:14 pregnancy. 13:15 Here is a recess positive fetus, a fetus with a recess antigen on the red blood 13:24 cell. 13:25 And in this scenario, this is the second pregnancy of a recess positive fetus 13:31 in a recess negative 13:33 mother. 13:35 Because this is the second pregnancy, the mother may have already created IgG 13:40 antibodies 13:41 against the recess antigen from the first pregnancy. Which means that the 13:46 recess antibodies 13:48 produced by the mother can cross the placenta and into the fetus's circulation, 13:53 attaching 13:54 onto the red blood cells of the fetus and causing hemolysis in the fetus. 14:01 Finally, antibodies formed against the M protein of streptococcus pyogenes, 14:07 also known as 14:08 group A streptococcus, can actually cross-react with cardiac tissues. 14:17 Cross-reaction of the antibodies activates the complement system, leading to a 14:22 serious 14:22 complication of strept pyogenes infection called rheumatic heart disease. And 14:27 this is 14:28 another example of a hypersensitivity type 2 reaction.