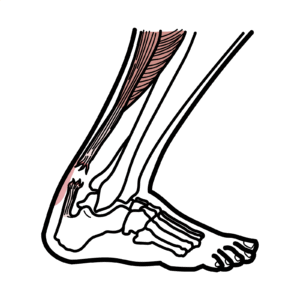
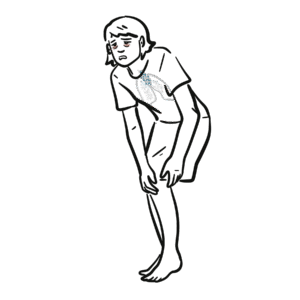
0:00 Hello, in this video we are going to talk about the ankle joint. 0:14 The ankle joint, or a tailo-crewal joint, is a synovial joint located in the 0:19 lower limb. 0:21 It is formed by the bones of the leg, the tibion fibula, as well as the foot, 0:27 the talus. 0:28 Over the ends of the tibion fibula form a bracket shaped socket, covered in 0:32 highline cartilage. 0:35 This socket is known as the malleola mortis. 0:38 The talus fits nicely into the mortis. 0:42 The talus bone in your ankle is a unique shape, with smooth cartilage covering 0:48 over 60% of 0:49 its surface. 0:51 Unlike other bones, it doesn't connect to any muscle. 0:55 The talus is broad anteriorly and narrow posteriorly. 1:01 When it comes to how your ankle works, think of it like a hinge. 1:06 The talus bone fits and glides within a slot between the tibia and fibula, 1:13 creating a 1:15 joint that acts like a door hinge. 1:24 This special setup allows your ankle to do two main movements, and these two 1:29 movements 1:30 are called dorsiflexion and plantar flexion. 1:34 Dorsiflexion is when the anterior part of the talus is held in mortis, and the 1:39 joint 1:40 is more stable, the foot comes up. 1:46 Plantar flexion, when you think about it, is really when you're standing on 1:50 your tiptoes. 1:51 You have your feet flex down. 1:54 The posterior part of the talus is held in mortis, and the joint is actually 1:58 less stable 1:59 in this position. 2:02 Next, let's talk about the ligaments of the ankle joint, which really help keep 2:10 the ankle 2:11 joint stable. 2:13 The ligaments can be divided into two components. 2:16 Firstly, the ligaments that join the distal, fibula, and tibia, then you have 2:21 the ligaments 2:23 that join the fibula and the tibia to the actual foot. 2:32 Let's talk about the ligaments that join the distal, fibula, and tibia together 2:37 . 2:37 The distal parts of the tibia and fibula are articulated through a sin-desmotic 2:44 joint known 2:45 as the tibio-fibula sin-desmosis. 2:49 This joint is stabilized further by the tibio-fibula ligament. 2:55 There are three sin-desmotic ligaments here. 2:58 The anterior tibio-fibula ligament, the interosseous ligament, and the 3:11 posterior tibio-fibula ligament. 3:12 Then you have the ligaments that join the fibula and tibia to the foot. 3:16 These are ligaments that originate from the medial malleolus of the tibia, or 3:20 the lateral 3:21 malleolus of the fibula, and then they attach to the foot. 3:25 The ligaments originating from the medial malleolus, so the tibia, these medial 3:30 ligaments are also 3:32 known as your deltoid ligaments, so medial ligaments are equal to deltoid lig 3:38 aments. 3:39 The medial ligaments consist of four ligaments, which fan out from the malleol 3:44 us attaching 3:45 to the talus, calcaneus, and navicular bones. 3:49 The primary action of the deltoid ligaments is to resist over-eversion of the 3:54 foot, so 3:55 the foot moving outwards, or the ankle moving outwards. 4:00 The ligaments originating from the lateral malleolus include the anterior tibio 4:04 -fibula, 4:05 and the calcaneofibula ligaments. 4:10 The main action of these ligaments is to resist over-inversion of the foot, so 4:15 the foot or 4:16 ankle moving inwards. 4:24 Now let's talk about the muscles of the ankle and the movement. 4:28 As mentioned, the ankle joint is a hinge type joint, with movement permitted in 4:33 one plane. 4:35 This allows for the movement dorsiflexion and plantar flexion. 4:40 Dorsiflexion is possible thanks to the muscles in the anterior compartment of 4:44 the leg, the 4:45 tibialis anterior, extensor-digitorium lungus, and extensor-halusis lungus. 4:51 Plantar flexion is possible thanks to the muscles in the posterior compartment 4:55 of the 4:56 leg, namely gastrocnemus, soleus, and posterior tibialis. 5:02 The gastrocnemus and soleus also help form the Achilles tendon, which then 5:06 attaches to 5:07 the calcaneus. 5:09 Eversion and inversion are produced at the other joints of the foot. 5:14 The movement of eversion and inversion, so the ankle or the foot moving out 5:20 wards and 5:20 inwards, are actually produced not by the ankle joint, but another joint of the 5:26 foot, 5:27 the sub-tailor joint. 5:35 The ankle joint is innervated by a few important nerves. 5:39 Firstly, the deep perineal nerve and the superficial perineal nerve are 5:44 branches of the common 5:45 perineal nerve, as well as the tibial nerve, which is a branch of the sciatic 5:51 nerve. 5:52 These nerves supply motor function for all the movements of the ankle, 5:57 including dorsiflexion, 5:59 plantar flexion, eversion, and inversion. 6:08 The arterial supply to the ankle joint is derived from the malleolar branches 6:12 of the anterior 6:13 tibial, posterior tibial, and fibular arteries. 6:16 The arteries palpated clinically are the dursalis pedis and posterior tibialis. 6:25 Let's talk about some clinical anatomy, beginning with the common ankle sprain. 6:33 An ankle sprain refers to partial or complete tears in the ligaments of the 6:38 ankle joint. 6:39 It usually occurs via excessive inversion to a plantar flexed and weight- 6:45 bearing foot. 6:46 So really, the most common injury is when your foot or ankle points inwards. 6:53 The lateral ligaments is most likely to be damaged for two main reasons. 6:57 Firstly, the lateral ligaments are weaker than the medial ligaments. 7:01 The lateral ligaments are also important in resisting inversion. 7:06 The anterior talofibular ligament is the lateral ligament most at risk of 7:11 irreversible damage. 7:14 The next clinical anatomy is POTS fracture. 7:21 A POTS fracture is a term used to describe a bi-malleolar fracture when your 7:27 medial and 7:28 your lateral malleolar get broken, or a tri-malleolar fracture when your medial 7:35 and lateral malleoli 7:36 as well as the distal tibia get broken. 7:42 This type of injury is produced by forced eversion of the foot, so your foot 7:46 gets twisted 7:47 outwards. 7:48 It occurs in a series of stages, so firstly, you have forced eversion, which 7:55 pulls on 7:55 your medial ligaments, producing an a-vulsion fracture of the medial malleolus. 8:03 The talus bone then moves laterally, breaking off the lateral malleolus, and 8:09 then the tibia 8:10 is then forced anteriorly, shearing off the distal and posterior parts against 8:21 the talus. 8:22 The final clinical anatomy is the foot drop, which is when you have injury to 8:27 the perineal 8:28 nerve, specifically the common perineal nerve and its branch, the deep perineal 8:34 nerve. 8:35 The common perineal nerve normally runs close to the fibula, and supplies the 8:39 muscle responsible 8:41 for dorsiflexion, which is lifting the foot up, as well as foot eversion, 8:46 turning the 8:47 sole of the foot outward. 8:50 If the common perineal nerve is injured, the person cannot dorsiflex the foot, 8:56 and a foot 8:56 drop occurs. 8:58 As a result, the person will have a high stepping gate to help the foot clear 9:03 off the 9:03 ground, when a person walks. 9:06 In addition, the foot will slap down on the floor, because it can't be lowered 9:10 in a controlled 9:11 manner. 9:18 So in summary, the ankle joint is a synovial joint, formed by the tibia and fib 9:22 ula, as 9:22 well as the talus. 9:24 The ankle joint is a hinge joint, and performs dorsiflexion and plantar flexion 9:29 . 9:29 The ankle and foot itself can also perform foot inversion and eversion. 9:36 The ankle joint is supported by strong ligaments, the medial ligament being 9:40 more strong than 9:41 lateral ligaments. 9:43 The ligaments can be divided into the ligaments that join the distal fibula and 9:48 tibia, and 9:49 the ligaments that join the fibula and the tibia to the foot. 9:53 An ankle sprain is a very common injury of the ankle joint, and is when there 9:57 is partial 9:58 or complete tears to the ligaments of the ankle joint.