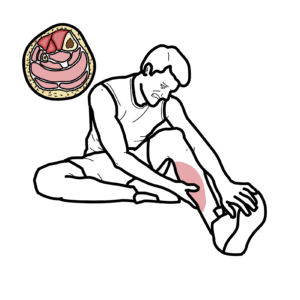
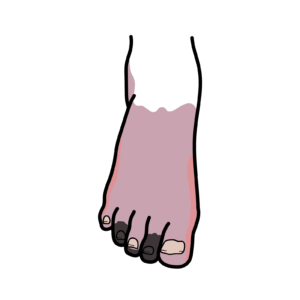
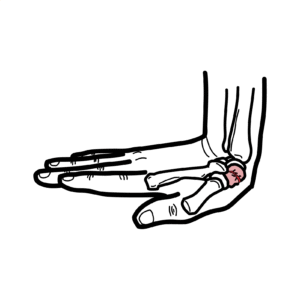
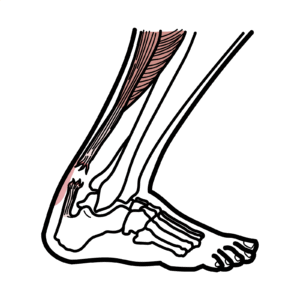
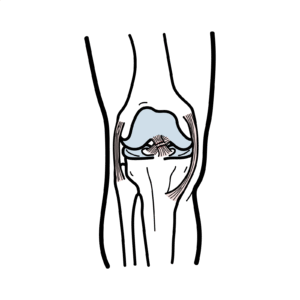
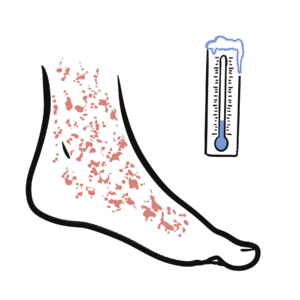
0:00 In this video, we're going to talk about foot drop. 0:11 A foot drop is characterized by the inability to lift the front part of the 0:16 foot. 0:17 This movement is called dorsiflexion. 0:20 It causes the affected foot to drag or slap against the ground while walking. 0:26 This condition can significantly affect a person's mobility and overall quality 0:30 of life. 0:32 Foot drop is a result of a problem with the common perineal nerve, or the fib 0:36 ular nerve. 0:37 The nerve that innervates the muscle responsible for dorsiflexion. 0:47 Let's learn a bit about the anatomy, talking about the sciatic nerve, which 0:52 then eventually 0:52 divides and becomes the common perineal nerve. 0:57 The sciatic nerve is a major nerve of the lower limb. 1:00 It is a thick flat band, approximately 2 centimeters wide, the largest nerve in 1:04 the body. 1:05 The sciatic nerve is derived from the lumbosacal plexus roots, L4 to S3. 1:12 The sciatic nerve is composed of two main nerve bundles, the common perineal 1:18 nerve and the 1:20 tibial nerve. 1:22 The sciatic nerve leaves the pelvis and enters the gluteal region via the 1:27 greater sciatic 1:28 foramen. 1:29 It emerges inferiorly to the piriformis muscle and then descends in an infrol 1:38 ateral direction. 1:40 It then enters the posterior thigh, so the back, bypassing deep to the long 1:47 head of the 1:47 biceps femoris. 1:51 The sciatic nerve is a major nerve in the lower limb, and then it splits into 1:57 two smaller 1:58 nerves, just above the back of the knee. 2:02 These two nerves are called the tibial nerve and the common perineal nerve. 2:12 The tibial nerve helps control the muscles of the calf, which are important for 2:16 plant 2:17 afflection, so standing on your tiptoes, as well as turning the ankle or foot 2:22 inwards. 2:23 This is termed ankle inversion. 2:32 The common perineal nerve, on the other hand, travels around the outer part of 2:36 the leg at 2:37 the top of the fibula. 2:39 This nerve wraps around the fibula and then descends down dividing into two 2:46 smaller nerves, 2:47 the superficial perineal nerve and the deep perineal nerve. 2:53 The superficial perineal nerve supplies the muscle that turns your foot outward 2:59 , ankle 2:59 eversion, and also provides sensation to the front of your lower leg, as well 3:06 as the top 3:07 of your foot. 3:09 The deep perineal nerve controls the muscles that lift your toes and foot up. 3:15 These are the tibialis anterior, extensor digitorium longus, extensor halusus 3:23 longus, 3:24 and perineus tertius. 3:28 The deep perineal nerve provides sensation to the area between the big toe and 3:32 the one 3:33 next to it. 3:35 The deep perineal nerve can be isolated to the number five nerve root. 3:46 Now if you injure the common perineal nerve, you then affect its two branches, 3:53 the superficial 3:55 and deep perineal nerve. 3:57 It will cause difficulty in lifting the foot up and also turning the foot 4:04 outward, eversion. 4:06 This can lead to a specific way of walking, where you lift your foot higher 4:13 than normal 4:13 and it can also increase the risk of falls. 4:17 All of this is what is termed a foot drop. 4:26 So what are the causes of a foot drop? 4:28 Well, you can think about it globally, looking at lesions at each of the sites 4:34 where the 4:35 nerve comes from and travels to. 4:38 So for example, if you have issues or lesions in the L5 nerve root, this can 4:42 cause a foot 4:43 drop, lesions in the lumbosacoplexus, lesion in the sciatic nerve, specifically 4:50 lesions 4:50 in a common perineal nerve or the deep perineal nerve and superficial perineal 5:00 nerve. 5:01 We will first talk about lesions that occur in a common perineal nerve, which 5:06 then will 5:07 obviously affect both the superficial and deep perineal nerve. 5:13 A major cause of common perineal nerve injury is through compression. 5:18 The compression of the actual common perineal nerve at the level of the fibular 5:23 head. 5:24 And this is due to the presence of a bony prominence at the fibular head, as 5:28 well as 5:28 a superficial positioning of the nerve itself at that level. 5:34 Compartment syndrome affecting the leg, either due to trauma or related ischem 5:39 ia, can lead 5:40 to perineal nerve ischemia with subsequent foot drop. 5:45 Not associated from orthopedic injuries such as knee dislocation, severe ankle 5:50 inversion 5:50 or some other fractures can also directly cause injury to the common perineal 6:00 nerve. 6:01 Theatrogenic causes from surgical procedures or protracted positioning and 6:06 anesthesia. 6:07 So for example, women in a lefotomy position giving birth causes compression 6:13 against the 6:13 fibular head and the actual common perineal nerve, as well as orthopedic 6:17 procedures can 6:18 possibly disrupt or injure the common perineal nerve. 6:28 There are many neurological disorders or causes of common perineal nerve injury 6:33 . 6:33 For example, a stroke that affects the motor pathway that supplies the actual 6:40 muscles of 6:41 the tibialis anterior or the lateral aspect of the tibute. 6:47 So a stroke that affects the motor pathway responsible for the nerve fibers 6:51 that will 6:52 eventually become the common perineal nerve. 6:58 Multiple sclerosis demyelinating lesions of the central nervous system can 7:01 affect also 7:02 the motor pathway, amiotrophic lateral sclerosis, ALS or motor neuron disease 7:11 causes issues with 7:13 the anterior horn of the spinal cord and thus the motor pathway. 7:19 Charcot-Mary tooth disease, a hereditary disorder characterized by motor 7:23 sensory polyneuropathy. 7:25 So this is a lower motor neuron injury as well as a motor neuritis multiplex, a 7:31 vasculitis 7:32 of the small vessels that supplies the actual common perineal nerve, gilien bar 7:37 re syndrome, 7:38 as well as diabetes, mellitus or other neurological disorders. 7:48 Injury at the level of the perineal nerve will only cause a foot drop, so loss 7:53 of dorsiflexion 7:55 as well as ankle eversion if the superficial perineal nerve is involved. 8:01 The nerve upstream, so the sciatic nerve itself, is otherwise okay, including 8:06 the tibial nerve, 8:08 the nerve that supplies the calf muscles. 8:15 But it's also important to consider lesions upstream that we also mentioned 8:20 earlier, such 8:21 as a L5 reticulopathy, most commonly due to an L4-L5 disc protrusion, prolapse 8:28 or herniation. 8:29 This will result in foot drop as well as neuropathic pain, starting in the lumb 8:34 ar region and radiating 8:35 down through the posterior thigh to the big toe. 8:40 Clinical examination has a straight positive leg raise test. 8:44 Also, lumbosacral plexopathy and any lesion along the sciatic nerve can lead to 8:51 a foot drop. 8:58 And so investigations to order for a person that comes to you with a new foot 9:04 drop include 9:05 x-ray and CT scan, first of all, around the knee or even the pelvis, really 9:10 looking for 9:11 any fractures, masses, arthritis or tumours that could be compressing anywhere 9:16 along the 9:17 nerve root, an MRI scan along the nerve pathway to see if there's any features 9:24 of nerve compression. 9:26 An electromyogram and nerve conduction studies can also be helpful in local 9:30 ising where the 9:31 lesion is, whether it is the common perineal nerve or below or the sciatic 9:38 nerve being 9:39 involved. 9:46 Treatment for a foot drop really importantly is physical therapy, the use of 9:52 orthosis as 9:53 well as splinting, pain management if there is a particular component to it. 9:59 Surgery can also be performed where early on a nerve repair can be done or even 10:05 a nerve 10:06 transfer, where a functional but less important nerve is transferred to a dist 10:11 al part of the 10:13 affected nerve. 10:20 So in summary, a foot drop is characterised by the inability of the front part 10:25 of the 10:25 foot to move up, this movement is called dorsiflexion. 10:30 It causes the affected foot to drag or slap against the ground while walking, a 10:34 foot drop 10:35 is a result of a problem with a common perineal nerve, the nerve that innerv 10:40 ates the muscle 10:41 responsible for dorsiflexion. 10:50 .