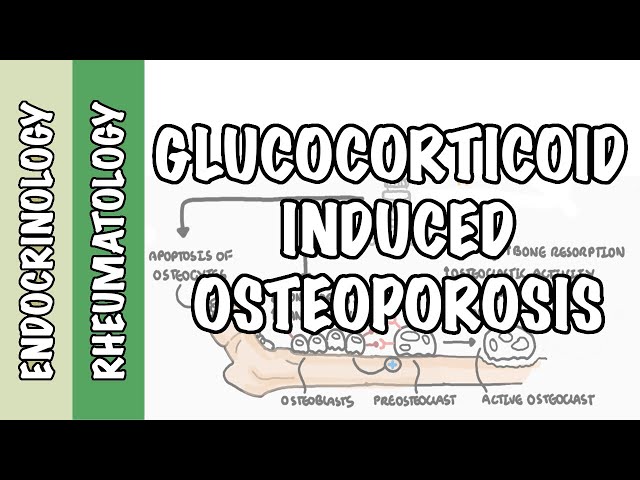
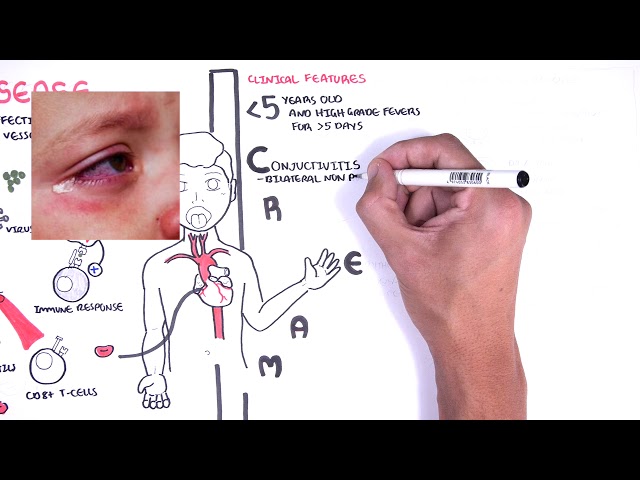
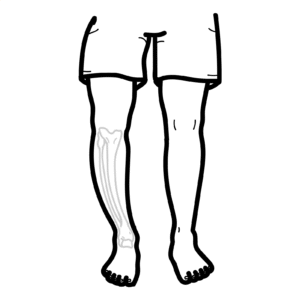
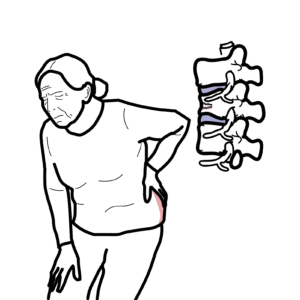
0:00 Hello, in this video, we're going to talk about Padgis disease of the bone. 0:09 This condition is actually a disorder of bone remodeling, where there's an 0:13 increase in 0:13 bone turnover. 0:15 What this means is that in the bone, there's increased bone breakdown, followed 0:20 by increase 0:20 in bone formation, and this results in areas of bony enlargement and deformity. 0:29 This talk about some physiology. 0:31 There are two important cells in the bone, the ones that break down bone, 0:36 termed osteoclasts, 0:37 and the ones that build new bone, called osteoblast. 0:42 Both normally work together in harmony to maintain bone structure and strength. 0:47 The bone formed will eventually become strong lamellar bone, which is a highly 0:52 organized 0:53 structure, with circular layers of collagen, alternating with longer chuteinol 0:59 ayers of collagen. 1:02 In Padgis disease, there are a few things that are found. 1:05 Firstly, there is an increase in number and activity of osteoclasts, the bone 1:12 breaking 1:13 cells. 1:15 Osteoclasts in Padgis disease are much larger, with a greater number of nuclei. 1:22 Up to 100, as compared to 3 or 5, that is found in normal osteoclasts, so a 1:28 significantly 1:30 higher number of nuclei. 1:32 These large osteoclasts are more sensitive to vitamin D, they are more 1:40 responsive to rank 1:41 ligand, which is expressed by osteoblasts to help stimulate osteoclasts, and 1:47 also they 1:48 express anti-apoptotic genes, which means that they are less likely to die 1:55 quicker. 1:56 All these factors cause osteoclastic activity to be increased in Padgis disease 2:00 at the bone. 2:02 Bone breakdown is then followed by bone formation, which leads to the bone 2:06 enlargement and deforming 2:08 looking bones. 2:12 Focusing more on the pathophysiology, the bone changes seen in Padgis disease 2:16 can be 2:16 divided into 3 phases. 2:20 The first phase is the osteolytic phase, followed by the mixed phase and 2:23 finally the 2:24 sclerotic phase. 2:27 In the initial osteolytic phase, there is a lot of bone resorption, bone 2:31 breakdown by 2:32 osteoclasts. 2:34 And this also causes increase in blood flow to the area, called hypervascular 2:42 ization. 2:43 Letic phase is then followed by mixed phase. 2:48 In the mixed phase, there is a mix of both active bone resorption and bone 2:53 formation, 2:54 that really replaces the normal lamella bone with haphazard woven bone. 3:01 The bones that are being formed are essentially weak. 3:05 Remember, the normal lamella bone, the bone is mature, normally highly 3:12 organized and 3:13 strong. 3:16 In contrast, the woven bone that is being produced in these osteoblasts is 3:22 actually composed 3:24 of loosely and randomly arranged collagen bundles. 3:27 The woven bone is weaker than normal lamella bone. 3:37 The final phase is a sclerotic phase, here you have a decrease in bone resor 3:43 ption and 3:44 an increase in osteoblastic activity. 3:49 In the sclerotic phase, the osteoblasts forms hard, dense, less vascular bone. 3:56 The sclerotic phase is also known as the burnt out phase of Padgis disease. 4:02 There is a picture of a bone that highlights the different phases of Padgis 4:08 disease. 4:09 On the left, you have the letic phase where the bone appears very brittle, 4:13 there's more 4:13 breakdown and then as it progresses, you get the sclerotic phase where you get 4:18 bone formation 4:19 and the bone itself has increase in size and density. 4:25 Now this abnormal structure will actually weaken the bone and despite the bones 4:30 being 4:30 enlarged because of the increase in osteoblastic activity, there is an 4:37 increased risk of fractures. 4:39 All these three phases may be present at the same time at different sclerotic 4:45 sites, meaning 4:46 you can have osteolytic phase on one bone and you can have a sclerotic phase 4:52 affecting 4:52 a completely different bone. 4:57 This disease can occur in more than one bone location. 5:04 The sclerotic sites most commonly involved are the skull, spine, pelvis and 5:08 lower extremities 5:09 such as the tibia. 5:12 People with Padgis disease of the bone are normally asymptomatic, they have no 5:16 symptoms. 5:17 Majority is actually identified incidentally with a blood test which shows an 5:22 elevation 5:23 of something called ALP which is a marker of bone turnover, otherwise patients 5:31 may also 5:31 complain of symptoms such as pain, pain in the joints, osteoarthritis, they 5:36 have an 5:36 increased risk of fractures, they can have disabling deformities of the bone 5:40 and the 5:41 bone itself that enlarges can compress against nerve causing a variety of 5:46 symptoms. 5:47 The bone enlargement especially can cause a lot of complications. 5:54 Padgis disease affecting the tibia or the femur can cause bowing of the actual 6:00 bone. 6:01 There is something called vascular steel syndrome which is essentially a mal 6:07 opathy where the 6:07 bone when it is highly vascularized, it gets all this blood flow and steals the 6:13 blood from 6:14 elsewhere because it is very active and so it can cause a lot of issues, for 6:20 example 6:20 it can steal blood supply from the nerves causing some form of neuropathy or my 6:28 elopathy. 6:29 Also it can result in high output heart failure because all the bone is 6:34 stealing the blood 6:36 as a result the heart works faster and harder. 6:42 Periodontal complication is a result of Padgis disease affecting the mandible 6:47 or the maxilla, 6:49 the bones in the face. 6:52 Padgis disease affecting bones in the inner ear and middle ear can result in 6:55 progressive 6:56 hearing loss and there is an increase of osteosarcoma in Padgis disease which 7:00 is essentially cancer 7:02 of the bone. 7:06 Padgis factors for developing Padgis disease include an increase in age, 7:09 slightly more 7:10 dominant in males, one third of cases have a genetic component to it where you 7:15 have an 7:15 autosomal dominant pattern of inheritance, the gene affected most commonly is 7:20 something 7:21 called sequestosome one gene. 7:25 Classical environmental factors have also been associated with Padgis disease 7:29 including 7:29 paramixovirus and having a rural lifestyle. 7:36 Plains in Padgis disease importantly are the bone turnover markers which will 7:41 be increased. 7:42 We talked about AOP which is alkaline phosphatase interestingly calcium levels 7:49 are normal. 7:51 You can also check the urine for hydroxyproline which may be increased in 7:55 people with Padgis 7:56 which indicates increase in bone lysis or breakdown. 8:02 In radiograph X-rays is very useful and depending on the phase of the Padgis 8:08 disease you can 8:09 see different things. 8:11 For example in the lytic phase as shown in this X-ray of the fema you can see 8:19 lytic lesions. 8:22 Radiographically this manifests as lytic wedge or blade of grass lesion. 8:29 In the mixed phase you can see both lytic lesions and sclerotic lesions. 8:35 Sclerotic lesions as shown in this X-ray you can see thickened cortical bone 8:41 because 8:42 of the building of the bone. 8:44 You can see coarse and thickened trabeculae and also in sclerotic phase you can 8:51 get bony 8:52 enlargement and deformity because of the increase in osteoblastic activity. 9:00 Another type of scan a bone scan is also very useful and is performed in people 9:05 who 9:05 have Padgis disease to see if there is any active disease. 9:13 Treatment of Padgis disease include antirezorptive therapy such as bisphosphon 9:17 ates. 9:18 Bisphosphonates work by inhibiting osteoclastic activity so reducing bone resor 9:24 ption bisphosphonates 9:25 work by laying themselves down on bone and then they allow themselves to be 9:29 absorbed 9:29 by the osteoclase and really induce apoptosis so osteoclase cell death. 9:37 Treatment also importantly consists of monitoring and managing the 9:40 complications associated 9:42 with Padgis disease. 9:44 So in summary Padgis disease of the bone is a disorder of bone remodeling with 9:48 an increase 9:49 in bone turnover. 9:51 It can be distinctly divided into three phases, osteolytic, mixed and sclerotic 9:56 phases. 9:56 Treatment is bisphosphonates, thank you for watching.