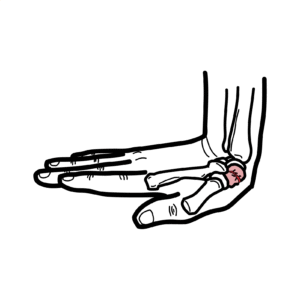
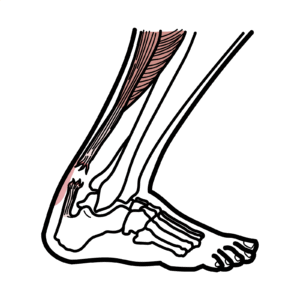
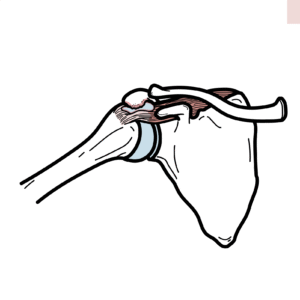
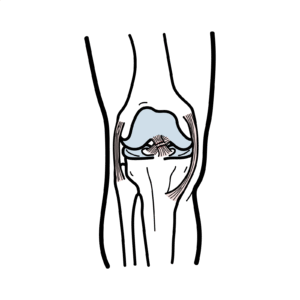
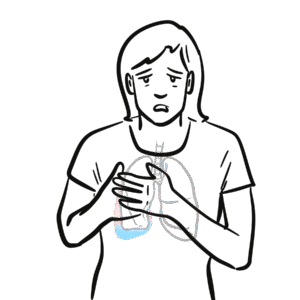
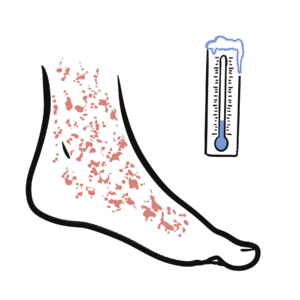
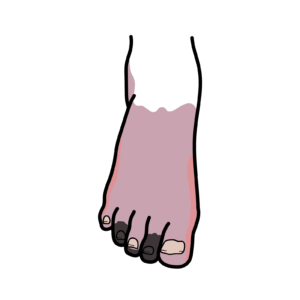
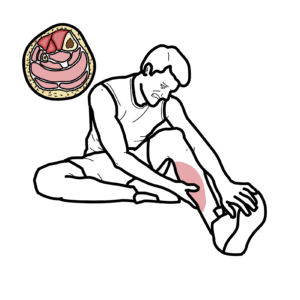
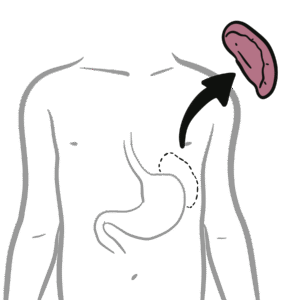
0:00 Osteonecrosis, also defined as a vascular necrosis or a septic necrosis, is 0:16 characterized as a 0:17 bone cell death that follows an impairment of blood flow to the bone from a 0:22 traumatic or non-traumatic 0:24 origin. Osteo means bone and necrosis means death. Around 1830, and I might 0:32 butcher this name, John 0:34 Crueville Haya, French anatomist and pathologist, described necrosis of the fem 0:41 oral head as a late 0:42 complication of hip trauma. He presumed vascular injury from trauma was the et 0:48 iology, only etiology 0:50 of necrosis. However, in the early and middle 20th century, various non- 0:55 traumatic factors were 0:56 identified to induce the disease or are involved in the development of osteone 1:01 crosis, including 1:02 alcohol and steroid use. Osteonecrosis most often happens in the hip joint, 1:09 the femoral head, but may also occur in other anatomical locations such as the 1:15 shoulders, 1:15 the knees and the ankles. In this video, we will most focus on the hip necrosis 1:21 , osteonecrosis. 1:23 So, the anatomy of the hip. The hip is a ball and socket joint. The socket is 1:37 formed by the 1:38 acetabulum, which is the part of the large pelvis bone. The ball is the femoral 1:43 head, 1:43 which is the upper end of the fema. The surface of the ball and socket is 1:48 covered with 1:48 articulate cartilage, a smooth, slippery substance that protects the bone and 1:53 enables them to glide 1:54 easily across each other. The pathophysiology of osteonecrosis is not 2:05 completely understood, 2:06 but most theories point towards a disruption or compromise blood flow as the 2:11 initiation of bone 2:13 death. And this disruption could occur from a traumatic or non-traumatic cause. 2:21 So, let's look 2:22 at each of these, beginning with traumatic cause of bone death. Traumatic cause 2:28 of bone death, 2:29 you can think of as a direct loss or occlusion of arteroflow to the bone, 2:37 leading to ischemia. 2:39 And the causes include a femoral neck fracture or dislocation, and these 2:46 injuries cause really 2:47 damage to the blood vessel that supply the femoral head, which can lead to oste 2:51 onecrosis, bone cell 2:54 death, radiation injury, and a rare condition called casein disease or decomp 3:03 ression syndrome 3:05 in scuba diving. What happens here is that when one goes scuba diving, it can 3:12 cause formation of 3:14 nitrogen bubbles that can occlude arterials, leading to osteonecrosis. 3:20 Non-traumatic causes of osteonecrosis usually affects adults, younger than 50 3:34 years old. 3:34 The causes include, or risks include, steroids, either endogenous or exogenous. 3:43 Significant alcohol use. 3:45 Goesher's disease, which is a marrow-replacing disease. What happens here is 3:52 that a type of fat, 3:54 a type of lipid called glucosiribroside cannot be adequately degraded and can 4:00 lead to direct 4:01 obstruction of blood flow, essentially. Sickle cell disease. In this condition, 4:08 red blood cell 4:09 undergo sickling and can then cause a direct obstruction of blood flow and bone 4:15 marrow 4:16 hyperplasia, and this will lead to essentially osteonecrosis. Any hyperquagul 4:23 able state can 4:24 lead to thrombosis formation, which can occlude the artery and blood flow. 4:29 Systemic lupus erythmatosis 4:31 and transplant patient are also at increased risk. Importantly though, the non- 4:36 traumatic 4:37 causes are also impacted by genetic predisposition, because quite interestingly 4:42 , some people who use 4:45 a lot of steroids and alcohol don't get this condition, osteonecrosis, while 4:50 others do, 4:51 and so there's thought to be a genetic play involved. Genetic factors are also 4:56 implicated 4:56 in hyperquagulability states, and hypo-fibrinolysis. Now, those traumatic and 5:05 atramatic causes of 5:06 osteonecrosis could be the same for any joint or bone, including the shoulder, 5:14 the femoral head, 5:16 the knee, or ankles. However, we are going to focus on the hip joint and the 5:22 femoral head. 5:23 Now, in regards to classification of the osteonecrosis of the hip, 5:32 the ficket and arlet classification was the earliest, and yet remains the most 5:36 widely 5:37 utilized classification. It uses plain radiographs, MRI, and clinical features 5:43 to place osteonecrosis into these stages, essentially pre-collapse stage of the 5:48 femoral head, 5:49 stage one and two, and post-collapse stage of the femoral head, three and four. 5:53 In stage one, 5:56 it looks quite normal, minor osteopenia. In stage two, you have scortic lesions 6:02 and subcontral 6:03 cysts, possibly. In stage three, you lose that round appearance of the femoral 6:08 head, 6:09 and in stage four, you lose the roundness of the femoral head, but also you 6:15 start losing 6:16 the roundness of the acetabula, and you develop significant, painful secondary 6:22 osteoarthritis, 6:24 which leads to the clinical presentation of osteonecrosis of the femoral head. 6:29 In the early disease, this is pre-collapse. In the early disease, the hip can 6:42 be painful, 6:43 and typically is the first symptom. It could be dull, ache, or throbbing pain 6:48 in the groin, 6:49 or the buttock. There can be difficulty standing, but more so weight-bearing, 6:54 so using weight on 6:56 the affected side. Moving the hip joint can also be slightly painful. Early on, 7:02 the hip joint has 7:03 actually relatively good range of motion, and this is because only the femoral 7:08 head is involved 7:09 in the early stages of disease. In the late stage of the disease, 7:18 this is termed post-collapse. In the late stages, it may take several months to 7:25 years for the disease to progress, but later, as a surface of the femoral head 7:31 collapses, 7:32 the entire joint becomes significantly arthritic. Hip and groin pain with 7:39 activity is very common, 7:42 and later, the pain also is present at rest. There is reduced range of motion 7:48 and stiffness. 7:50 Investigations for osteonecrosis include an MRI, which is the gold standard in 8:01 detecting 8:02 early osteonecrosis, and is able to differentiate from other differential 8:06 diagnosis, such as 8:08 bone bruising. Here is an MRI of an obvious right osteonecrosis of the femoral 8:16 head, 8:16 with some collapse, but also this patient actually has left-sided osteonecrosis 8:21 as well, so bilateral. 8:23 Diagnosis can also be made with plane radiographs and x-ray, but this is 8:29 typically in moderate to 8:31 late disease. Here is an x-ray of a right femoral head, and here you can 8:41 appreciate 8:41 there's collapse of the femoral head. This is definitely at least stage three, 8:46 and most likely, 8:47 it is stage four, because the acetabulum is already roughened. Treatment for 8:57 osteonecrosis 8:58 of the hip. There is non-surgical treatment, which really involves lifestyle 9:02 changes. 9:03 You'd have to be using crutches, for example, or walking aids, and then there's 9:07 analgesia for pain. 9:08 There is a role for bisphosphonates as well for osteonecrosis. However, there 9:15 is not great evidence 9:16 for bisphosphonates, and funnily enough, bisphosphonates can also lead to oste 9:21 onecrosis mainly of the jaw. 9:28 The definitive treatment is really surgery, and in early disease, hip 9:33 preservation surgery is used. 9:35 Things to do include core decompression, where drilling one large hole or 9:42 several 9:42 smaller holes into the femoral head is done, to relieve pressure in the bone 9:47 and create channels 9:49 for new blood vessels to nourish the affected areas of the hip. There's surgery 9:54 called 9:56 vascularized fibular graft. Here, a segment of bone is taken from the small 10:01 bone 10:02 in the leg, typically the fibula, along with its blood supply. This graft is 10:07 then transplanted 10:08 into a hole created in the femoral neck, and the head, and the archery and the 10:14 vein are reattached 10:15 to help heal the area of osteonecrosis. In the late disease stage, so stage 10:21 three and four, 10:23 in the classification we learned with severe osteoarthritis or loss of function 10:28 , a total hip 10:29 replacement is required. So in summary, osteonecrosis is defined as really bone 10:43 cell death. That 10:44 follows impairment of blood flow to the bone itself, and this could be either 10:48 through a traumatic 10:50 or a traumatic cause. We mainly focused on the femoral head, the hip joint oste 10:57 onecrosis, 10:58 but really all the causes we have learned and treatment relatively the same 11:03 amongst all the 11:04 joints that suffer from osteonecrosis. Thank you for watching. 11:20 [BLANK_AUDIO]