Overview
Post‑splenectomy immunodeficiency refers to the increased susceptibility to infection following removal (or functional loss) of the spleen. The spleen plays a critical role in filtering bloodborne pathogens, especially encapsulated bacteria, and in mounting both innate and adaptive immune responses. Loss of splenic function leads to impaired opsonisation, reduced IgM production, and defective clearance of abnormal erythrocytes and immune complexes. The most feared complication is Overwhelming Post‑Splenectomy Infection (OPSI) — a rapidly progressive, often fatal sepsis, most commonly due to Streptococcus pneumoniae, Neisseria meningitidis, and Haemophilus influenzae. Incidence of OPSI is highest in the first 1–3 years post‑splenectomy but remains elevated lifelong.
Definition
Asplenia: Complete absence of spleen (surgical or congenital).
Hyposplenism: Reduced splenic function despite anatomical presence.
Overwhelming Post‑Splenectomy Infection (OPSI): Fulminant sepsis in asplenic/hyposplenic patients, often within hours of symptom onset.
Encapsulated bacteria: Microorganisms with polysaccharide capsules that evade phagocytosis without opsonisation.
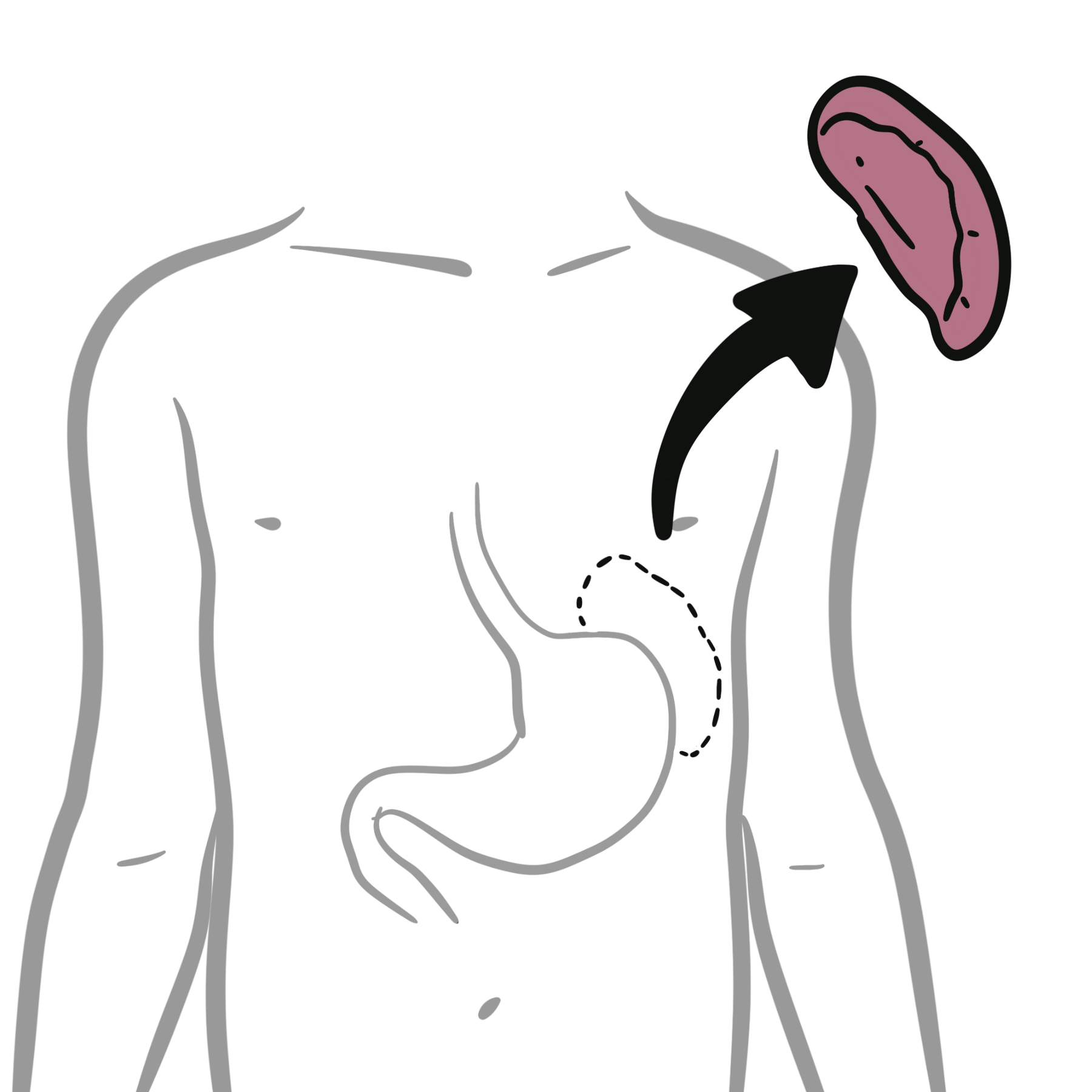
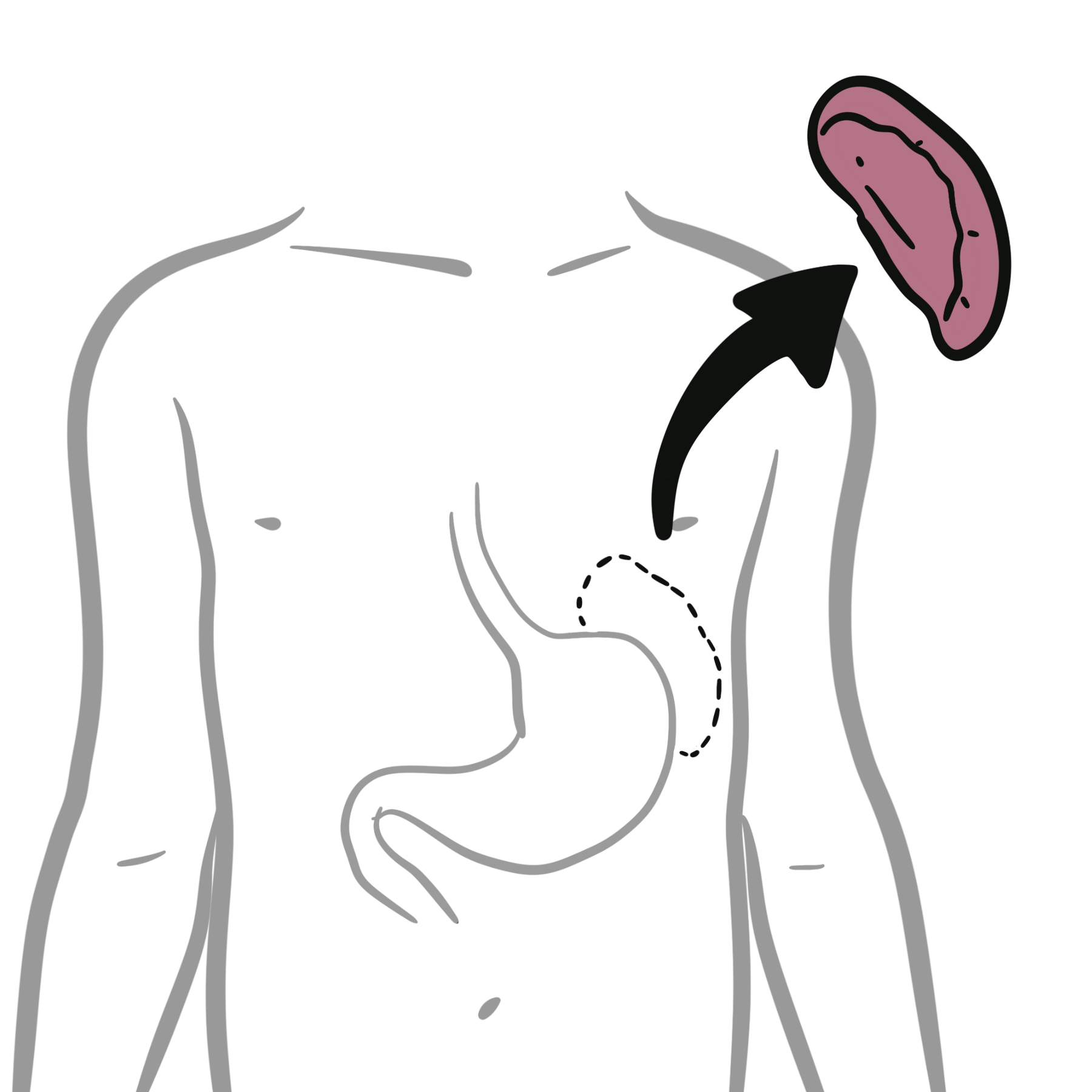
Anatomy & Physiology
- White pulp: Lymphoid tissue (periarteriolar lymphoid sheath, follicles) — site of antigen presentation and antibody production.
- Red pulp: Filters aged/damaged RBCs, removes opsonised pathogens.
- Marginal zone: Rich in macrophages and B cells; critical for T‑independent antibody responses to polysaccharide antigens.
Aetiology & Risk Factors
Aetiology
- Surgical splenectomy (trauma, haematological disorders, malignancy).
- Functional asplenia (sickle cell disease, coeliac disease, advanced HIV, autoimmune disorders).
Risk factors
- Young age at splenectomy (<16 years).
- Splenectomy for haematological malignancy.
- Poor vaccine uptake.
- Delay in antibiotic initiation during febrile illness.
- Lack of patient education on OPSI risk.
Pathophysiology
- Loss of splenic macrophages and marginal zone B cells.
- Impaired clearance of opsonised bacteria from blood.
- Reduced IgM and complement activation against polysaccharide antigens.
- Increased susceptibility to encapsulated organisms.
- Risk of fulminant sepsis (OPSI) with rapid progression to shock and DIC.
Clinical Manifestations
- Often asymptomatic until infection occurs.
- OPSI: Sudden fever, chills, malaise → rapid progression to septic shock, DIC, multi‑organ failure.
- Recurrent or severe infections with encapsulated bacteria.
OPSI can occur decades after splenectomy — risk is lifelong.
Diagnosis
- Clinical suspicion in any febrile asplenic patient.
- Blood cultures before antibiotics (do not delay treatment).
- Peripheral smear: Howell–Jolly bodies (nuclear remnants in RBCs).
- Immunological tests: Reduced IgM, impaired response to polysaccharide vaccines.
Treat febrile illness in asplenic patients as sepsis until proven otherwise.
Treatment
- Acute infection: Immediate empiric IV antibiotics (e.g., ceftriaxone ± vancomycin) after cultures.
- Prevention:
- Vaccinations: Pneumococcal (PCV13 then PPSV23), H. influenzae type b, meningococcal (MenACWY, MenB), annual influenza.
- Prophylactic antibiotics: Daily oral penicillin V (especially in children, first 1–2 years post‑splenectomy; lifelong in high‑risk adults).
- Standby antibiotics for self‑administration at first sign of fever.
- Patient education: Medical alert identification, prompt medical review for fever.
Vaccinate ideally ≥2 weeks before elective splenectomy or ≥2 weeks after emergency splenectomy.
Complications and Prognosis
Complications
- OPSI (mortality up to 50%).
- Recurrent bacterial infections.
- Severe malaria or babesiosis in endemic areas.
- Thrombocytosis → increased thromboembolic risk.
Prognosis
- Lifelong increased infection risk.
- Mortality from OPSI highest in first few years but persists indefinitely.
- Good prognosis with adherence to vaccination, prophylaxis, and rapid treatment.
References
- Srikandi NMP, Suardamana K. Aspects of immunology and management of post‑splenectomy patients. Int J Health Med Sci. 2024;7(3):59‑68.
- Di Sabatino A, Carsetti R, Corazza GR. Post‑splenectomy and hyposplenic states. Lancet. 2011;378(9785):86‑97.
- Davies JM, et al. Review of guidelines for prevention and treatment of infection in patients with absent/dysfunctional spleen. Br J Haematol. 2011;155(3):308‑317.
- Cadili A, de Gara C. Complications of splenectomy. Am J Med. 2008;121(5):371‑375.

Discussion