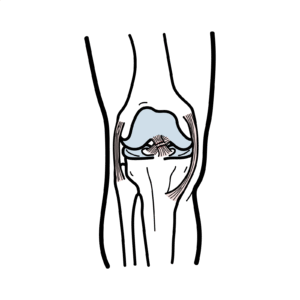
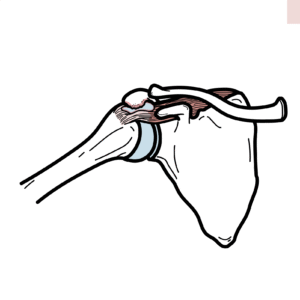
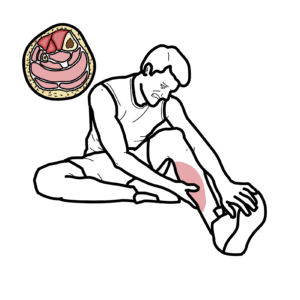
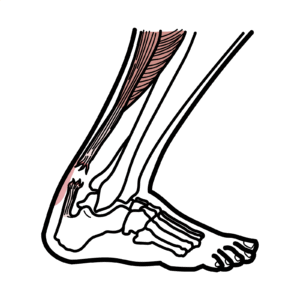
0:00 In this video, we're going to talk about osteoarthritis. 0:08 This is an overview and introduction. 0:11 We will mainly focus on osteoarthritis of the knee joint because it is a very 0:14 common 0:15 condition. 0:16 Now, before going into osteoarthritis, we should revise the synovial joint and 0:21 its anatomy. 0:23 Because one, the knee joint is a synovial joint and two, osteoarthritis occurs 0:28 commonly 0:29 in synovial joints. 0:32 So the bones that form the joints are surrounded by periosteum. 0:36 Remember, the periosteum is a very painful and sensitive structure because it 0:42 contains 0:42 pain receptors. 0:45 The ends of the bones are surrounded by shiny substance called articular cart 0:51 ilage. 0:52 This cartilage helps in absorbing shock and also allows for gliding between the 0:59 bones. 1:00 Surrounding the synovial joint is the synovial membrane. 1:04 The synovial membrane produces what's known as synovial fluid. 1:09 Now, surrounding the synovial membrane, you have the fibrous capsule, which 1:14 together with 1:15 the synovial membrane, forms what is known as the articular capsule. 1:20 The synovial joint is also further stabilized by ligaments. 1:26 And there are many ligaments depending on which synovial joint you're talking 1:31 about. 1:32 Let's look at another diagram now, drawing out the same structures. 1:38 The blood vessels supplying the articular capsule help bring in immune cells 1:43 and also 1:44 help bringing in nutrition, but it also is necessary for draining waste. 1:50 This area is also innervated by nerves, nerve fibers. 1:55 We talked about a type of college called articular college that surrounds the 2:00 ends of the bone. 2:01 Well, in a knee joint, there is another college, a fibrocodlaginous college 2:08 called meniscus 2:09 or meniscai for plural. 2:12 This guy are like wedge discs stuck between two bones. 2:18 And it really helps with the joint stability and helps also in absorbing shock 2:23 at the joint. 2:24 A good example is the knee niscus, which when you run absorbs the shock on 2:31 impact. 2:33 When you are young and healthy, you are mobile and your joints are stable and 2:38 strong. 2:39 In osteoarthritis, you have degeneration of the joint. 2:43 More specifically, degeneration of the articular cartilage. 2:47 You have articular cartilage breakdown, damage and degeneration. 2:52 This is in the presence of joint space narrowing. 2:57 We would call this mild osteoarthritis, which is very common when we age. 3:02 However, there are many risk factors which predispose and increase the risk of 3:08 early 3:08 osteoarthritis. 3:10 These include age, being female, while this is specifically for the hip joint, 3:16 obesity, 3:17 which increases stress on the knee joints, previous joint injuries such as 3:23 sports injury, 3:24 and also having a lower leg deformity or malalignment such as bow legs or knock 3:29 knees. 3:30 This essentially means having a valve risk or valve-gis feature at the knee 3:38 joint. 3:39 There are also some rheumatic diseases and genetics that are risk factors for 3:43 developing 3:44 osteoarthritis. 3:47 Once mild osteoarthritis occurs, progression is inevitable and can be slow or 3:55 fast. 3:56 Severe osteoarthritis eventually occurs. 4:00 Here you can have bone on bone, joint space narrowing, loss of articular cart 4:06 ilage, and 4:07 formation of bone spurs called osteophytes. 4:12 One way osteoarthritis is categorized is into primary osteoarthritis or 4:18 secondary osteoarthritis. 4:21 Primary osteoarthritis is idiopathic, where there is no proceeding injury and 4:25 osteoarthritis 4:26 is basically a result of old age and degeneration. 4:31 Secondary osteoarthritis is different. 4:33 It is usually due to some something else. 4:37 Examples include congenital abnormality, trauma, and inflammatory orthopathies. 4:49 Clinical presentation of osteoarthritis, so the signs and symptoms include pain 4:53 , which 4:54 is exacerbated with exercise and relieved with rest. 4:59 Weather has also been shown to influence the pain. 5:03 There is also stiffness of the joint. 5:07 In severe osteoarthritis, pain can even occur at rest and at night. 5:14 In severe osteoarthritis, you can also have malalignment of the knee joint. 5:18 You can have genu-valgus or genu-val-ris. 5:25 And this will depend on where the osteoarthritis is located at the joint, if it 5:28 's medial or 5:29 lateral. 5:32 On clinical examination, there can be muscle wasting. 5:35 The patient may be overweight. 5:38 In osteoarthritis, there is often tenderness on joint palpation, plus minus 5:44 osteophytes. 5:46 It can be presence of joint effusion during acute exacerbations. 5:51 Preparations is common, and there's also reduced joint movement because of 5:57 stiffness. 5:59 Differential diagnosis for osteoarthritis can mainly be crystals being within 6:04 joint space. 6:05 This is known collectively as calcium pyrophosphate crystal deposition disease. 6:11 It can also be gout, for example. 6:15 The differential diagnosis is septic arthritis, where bacteria invades the 6:20 joint space essentially, 6:21 and this is a medical emergency. 6:24 Rheumatoid arthritis is another differential diagnosis, especially in the 6:29 elderly. 6:29 This is characterized by immune cells and complexes attacking the joint tissue 6:33 and the 6:33 joint space. 6:36 Let us now talk about the pathophysiology and how these signs and symptoms 6:41 arise and the 6:41 clinical features. 6:44 Here again, I am drawing the synovial joint of the knee specifically. 6:49 Here are the two bones, for example, and this is the progression. 6:54 As you can see with the bones, there are some abnormalities. 6:57 Bone changes in osteoarthritis as it progresses. 7:03 In blue, covering the bone surfaces are articular college, which is Highline 7:09 College, which as 7:10 you can also see is slowly degrading as osteoarthritis progresses. 7:16 The synovial joint is not a synovial joint without the synovial membrane here, 7:21 and the 7:21 synovial membrane is made out of cells called synovial sites. 7:26 These guys produce synovial fluid. 7:29 Within the bone, you have many cells, including osteocytes, which then can 7:35 become osteoblasts. 7:36 Osteoblasts are the bone building cells. 7:40 There is also another important bone cell, which I have not drawn here, called 7:44 osteoclasts, 7:45 which break down bone. 7:47 Anyway, there is blood supply to the synovium. 7:52 Within the synovium, you can find tissue macrophages. 7:58 Now the actual pathogenesis of osteoarthritis differs, and there is no exact 8:03 one start-off 8:05 point. 8:06 But we know what cells are found within the joint tissue, and this is just an 8:12 overall example 8:12 of what happens. 8:15 So the tissue macrophages can become stimulated because of a variety of reasons 8:20 . 8:21 For example, it can be stimulated from trauma, from joint abnormalities or mal 8:25 alignment, 8:26 degeneration of tissues, and basically the risk factors of osteoarthritis. 8:32 So this will activate these immune cells, and which will cause the release of 8:36 many chemicals 8:37 and inflammatory cytokines. 8:42 So for example, the macrophages will release cytokines, TNF alpha, interleukin 8:47 1B and interleukin 8:48 6, BEGF, and stimulate E-selectin. 8:53 BEGF essentially will cause new blood vessels to form. 8:59 It's an important factor in angiogenesis. 9:03 E-selectin essentially is where the cells around the vasculature will express 9:09 receptors 9:10 E-selectin, so that other immune cells can be recruited to the area. 9:16 And so BEGF and E-selectin, together with the cytokines, will promote 9:21 inflammatory cell 9:22 recruitment and the inflammatory process itself. 9:27 You get recruitment of immune cells, such as T-cells, specifically T-helper 9:32 cells, and 9:32 this will further produce cytokines in response to trauma and other factors. 9:38 Neutrophils is another immune cell, which gets recruited and is mainly 9:42 important in 9:43 acute inflammatory response, so it's not that common in osteoarthritis. 9:50 T-cells, macrophages, and all the cytokines produced in the area stimulate the 9:54 synovial 9:54 sites to produce proteases. 9:58 The neutrophils, already in the fluid, also produce proteases. 10:03 Proteases are enzymes which break down proteins, and these guys are very 10:09 destructive, thus 10:10 they can damage surrounding tissues, mainly the college. 10:15 The cytokines also stimulate osteocytes, which in turn activate osteoblasts to 10:20 build 10:20 a new bone to compensate, this is sort of a repair mechanism. 10:25 When there is damage and inflammation, the osteoblasts will work, and will aim 10:33 to repair 10:33 the bone that is getting damaged, thus causing what is known as sub-conderal 10:38 sclerosis, which 10:39 is whitening below the cartilage. 10:43 In the long term, the depositing of new bones causes osteophytes, which are 10:49 these bones 10:50 spurs basically, and these are abnormal. 10:55 It is important to take into account that with age there is thinning of the 10:59 cartilage, 11:00 and this is caused by decrease in hydration to the cartilage. 11:04 Age also leads to brittle bones and conjural calcinosis. 11:08 All these factors increase the risk and progression of cartilage destruction. 11:13 It's also important to note that all the risk factors we talked about earlier 11:18 increases 11:19 the risks of cartilage degradation and destruction, so previous trauma, joint 11:24 malalignment, etc. 11:29 So how does pain occur in osteoarthritis? 11:32 Well, in summary, remember that there are many cytokines produced in osteoarth 11:37 ritis. 11:38 Some of these cytokines are pain-signaling molecules such as some types of 11:43 prostaglandins 11:44 and also bradykinin, or BK. 11:48 These guys stimulate nearby sensory neural fibers. 11:52 The sensory neuron will go to the level of a spinal cord and synapse with the 11:58 second 11:58 order neuron there, which then will bring the information up to the brain, 12:05 where essentially 12:07 the sensation of pain or pain perception is captured. 12:11 If you are interested to see how pain is processed and works, I have a video on 12:16 pain as well. 12:18 It is also very important to understand that people have different pain 12:23 tolerance and sensitivity. 12:25 The longer a person feels pain, the more chronic it becomes, and this means 12:29 there is an increase 12:31 in pain sensitivity. 12:33 But so interesting, some people with severe osteoarthritis feel minimal pain, 12:38 and that's 12:38 just because of variation. 12:41 They still have a limp and problems with mobility, but pain is not really an 12:46 issue for some 12:47 people. 12:48 Finally, it is important to introduce joint aspiration, also known as arthrocy 12:54 nthesis, 12:55 which is a type of investigation that looks at what is inside the synovial 13:01 fluid. 13:02 It is an investigation performed with any patient presenting with monoarthritis 13:07 , one 13:08 inflamed joint. 13:10 This is important because doctors want to differentiate between other causes of 13:13 monoarthritis, such 13:14 as ruling out septic arthritis or gout. 13:19 Anyways, synovial fluid aspiration involves drainage of the fluid from the 13:25 joint space, 13:26 then analyzing the fluid with microscopy, staining or with microscopy culture 13:32 and sensitivity. 13:33 In general basic osteoarthritis, joint aspiration can reveal leukocytes, neut 13:39 rophil, a neutrophil 13:41 count that range up to 2000 microliters. 13:45 In septic arthritis, this number is way higher, 50,000 plus. 13:51 Finally, let's look at an overall management and algorithm for osteoarthritis. 13:58 So it's important to take a history to find out any trauma or associated fever. 14:08 Next it is important to examine the joint, and if it's a knee joint, perform a 14:11 full knee 14:12 examination. 14:14 An investigation that is very important initially is an x-ray of the joint. 14:20 For osteoarthritis, there's a good acronym to look at the changes seen in osteo 14:25 arthritis. 14:25 This is loss. 14:27 L is for loss of joint space, O is for the presence of osteophytes or bone sp 14:32 ares, S is 14:34 for sub-condrel sclerosis or the other S for sub-condrel cysts. 14:41 Another investigation that can be performed is to help exclude differential 14:47 diagnosis 14:48 and look at the severity of osteoarthritis, and this includes looking at ESR, r 14:55 heumatoid 14:56 factor and anti-CCP. 14:59 Joint aspiration can also be performed, and we talked about it earlier. 15:03 An MRI is very good for looking at soft tissue involvement, but remember x-ray 15:10 is better initially. 15:14 After diagnosing osteoarthritis, you can have non-pharmacological management or 15:19 pharmacological 15:20 management. 15:22 Non-pharmacological management include losing weight, educating the patient 15:27 about osteoarthritis, 15:28 physiotherapy, using a walking stick, using a knee brace, appropriate footwear 15:35 and acupuncture 15:36 has also been shown to benefit some people. 15:39 There's also heat and cold therapy. 15:43 Pharmacological management include firstly, first line is using paracetamol and 15:49 then topical 15:50 non-storoidal anti-inflammatories or capsaicin. 15:54 This can then be moved on to oral non-storoidal anti-inflammatory drugs. 15:59 But prescribing of oral NSAIDs means that you also have to prescribe proton 16:04 pump inhibitors 16:06 to prevent any gastric problems. 16:10 Other pharmacological stuff include glucocorticoid injections, which are 16:15 usually used for exacerbations 16:17 of osteoarthritis. 16:18 There's also viscose supplementation such as synvisk. 16:23 Opioids are used sometimes and this is in severe cases and for those who cannot 16:28 undergo 16:29 surgery. 16:30 Other forms of supplements include glutamine and chondroitin, which has 16:36 differing results. 16:37 And finally, turmeric and fish oil is also shown to be beneficial. 16:41 Finally, obviously there is knee surgery, which can involve total knee 16:47 replacement. 16:48 And this is the last line and is shown to improve knee joint pain and mobility. 16:56 Thank you for watching. 16:57 I hope you enjoyed this video.