Overview
Syncope is defined as transient loss of consciousness due to reduced cerebral blood flow. Syncope, commonly described as “fainting,” is a symptom, not a disease, and can be classified according to the cause, the most common of which is neurocardiogenic syncope. Presyncope is feeling of fainting and patient often presents as feeling dizzy. Syncope is a transient loss of consciousness and is usually always due to a cardiovascular event such as arrhythmia or postural hypotension. Important to differentiate syncope (global cerebral hypoperfusion) with seizure (abnormal, excessive or synchronous neuronal activity in the brain) as both result in a transient loss of consciousness.
Types of true syncope
- Neurally mediated syncope
- Postural hypotension
- Cardiogenic syncope
Definition
| Definition Consciousness Awareness of the environment and being able to respond to it Syncope Transient loss of consciousness and postural tone from reduced cerebral perfusion, followed by spontaneous and full recovery Presyncope refers to a reduction in cerebral perfusion resulting in a sensation of impending loss on consciousness, but not actually pass out. This sensation include lightheadedness, feeling of warmth, diaphoresis, visual blurring and nausea. Transient loss of consciousness is a state of real or apparent loss of consciousness with loss of awareness, characterised by amnesia for the period of unconsciousness, abnormal motor control, loss of responsiveness and a short duration. |
Differential Diagnosis
- Seizures
- Cataplexy
- Intracranial haemorrhage
- Intracerebral haemorrhage
- Subarachnoid haemorrhage
- Vertebrobasilar TIA
- Carotid TIA
- Subclavian steel syndrome
- Intoxication
- Cardiac arrest
- Coma
| Differentiating features | Seizures | Syncope |
| Age | Any | 8-15 years |
| Timing | Whenever | Day |
| Situation | Commonly during activity | Standing |
| Prodrome | Brief (twitching, hallucinations) | Long (dizziness, sweats, nausea) |
| Duration | Variable | Under 5 minutes |
| Tonic-clonic movement | Common | Rare |
| Colour change | Maybe cyanosis | Pallor |
| Injury | Common | Rare |
| Incontinent of urine | Common | Rare |
| Recovery | Drowsiness, confusion or headache | Quick Recovery |
| Aetiology of syncope | ||
| Neurally mediated syncope (Reflex syncope) | Vasovagal syncope (Neurocardiogenic) | Provoked by
|
| Situational syncope | Provoked by
| |
| Carotid sinus hypersensitivity | Provoked by
| |
| Postural (Orthostatic) hypotension | Primary autonomic failure | Lewy body disease Multiple system atrophy |
| Secondary autonomic failure | Diabetes HIV neuropathy | |
| Drug-induced (most common cause of postural hypotension) | Anti-hypertensives, diuretics, antidepressants | |
| Volume depletion | Blood loss, adrenal insufficiency, dehydration | |
| Cardiac syncope | Arrhythmias | Bradycardia Tachycardia |
| Structural cardiac disease | Valvular heart disease Ischaemic heart disease Cardiomyopathy Pericardial disease |
| Remember Vasovagal syncope is also known as neurocardiogenic syncope. Postural hypotension is also known as orthostatic hypotension |
| Syncope pentad transient loss of consciousness, loss of muscle tone, loss of responsiveness, amnesia during event, short duration, spontaneous recovery |
Approach
History
- Circumstances of the event
- Witnessed?
- convulsions likely seziure
- Person’s posture immediately before losing consciousness
- standing up then fainting likely postural hypotension
- Trigger?
- coughing, sneezing, micturition likely situational syncope
- presence or absence of any prodromal symptoms (such as sweating or feeling warm/hot) and movement during event (for example, jerking of the limbs and duration);
- Appearance (for example, whether eyes were open or shut) and colour of the person during the event)
- Any biting of the tongue (record whether the side or the tip of the tongue was bitten)
- Injury occurring during the event
- Posterior shoulder dislocation likely seizure
- Headstrike secondary intracranial haematoma?
- Duration of the event (onset to regaining consciousness)
- Recovery – confused?
- Current medication
- Screen for non syncopal causes
- Seizures
- Hypoglyaemia
- Head injury
- Narcolepsy
Examination
- Injures to fall
- Head trauma
- Confusion/post ictal
- Neurological assessment
- Hydration status
- Murmur
- Blood loss
- Cardiovascular exam
- BP, HR
- Postural change in BP
- Changes >20mmHg systole indicate orthostatic hypotension
| Think If confirmed postural hypotension review medications followed by neurological examination. If neurological exam normal consider postganglionic autonomic insufficiency. |
Neurally mediated syncope (reflex syncope)
Syncope is defined as transient loss of consciousness due to reduced cerebral blood flow. Neurally mediated syncope or reflex syncope occurs when there is increases parasympathetic activity with concurrent decrease in sympathetic activity. The increase parasympathetic activity and decreased sympathetic activity (sympathetic withdrawal) causes a decreased heart rate, reduced heart contractility and vasodilation. All this causes reduces perfusion to the brain causing syncope. Three types of neurally mediated syncope which are caused by this mechanism:
- Vasovagal syncope
- Situational syncope
- Carotid sinus hypersensitivity
For neurally mediated syncope patients can experience presyncopal symptoms such as feeling unwell, nauseated, dizzy, or tired, with yawning, blurred or ‘tunnel’ vision, or altered hearing. After their syncopal episode patients recover rapidly.
Often patient experience what called Bezold–Jarisch reflex
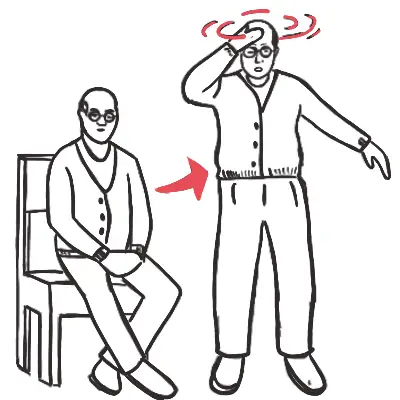
Postural Hypotension (orthostatic hypotension)
Orthostatic hypotension is an important, treatable cause of dizziness, syncope and falls. Less frequently it leads to visual disruption, dyspnea on exertion, angina and even stroke. Orthostatic hypotension also known as postural hypotension results from a failed sympathetic response when standing upright resulting in decrease venous return and cardiac output causing dizziness, syncope and/or fall.
Main mechanism of postural hypotension
- Autonomic failure
- Volume depletion
- Medication induced
Click here for more information on postural hypotension
Cardiac syncope




Discussion