Overview
Orthostatic hypotension is an important, treatable cause of dizziness, syncope and falls. Less frequently it leads to visual disruption, dyspnea on exertion, angina and even stroke. Orthostatic hypotension also known as postural hypotension results from a failed sympathetic response when standing upright resulting in decrease venous return and cardiac output causing dizziness, syncope and/or fall. Important to note that a common problem in patient with orthostatic hypotension is the concurrent presence of supine hypertension.
Normal Physiological Response to Orthostasis (standing up)
- Standing up from a recline or sitting position results in pooling of 500-1000mL of blood in the lower extremities and splanchnic circulation.
- The physiological response
- ↓venous return to the heart → ↓ventricular filling → ↓cardiac output → baroreceptor reflex
- Baroreceptor reflex
- → stimulation of the vasomotor center → peripheral vasoconstriction → ↑BP → ↑venous return + ↑cardiac output
- → stimulation of the cardiovascular center → ↑HR → ↑cardiac output +↑venous return
- Overall clinically there is a small reduction in systolic BP (<10mmHg), increase in diastolic BP and an increase in HR
| Remember Orthostatic hypotension results when one or more of these compensatory mechanisms fails leading to a drop in BP when standing up |
Diagnosis
- A fall in BP of ≥20 mmHg systolic or 10 mmHg diastolic on standing from supine
Aetiology
- Medications
- Antihypertensives
- Vasodilators
- Antipsychotics
- Opiates
- Chronic hypertension - reduced baroreflex sensitivity and left ventricular compliance - common in elderly
- Volume depletion
- Sepsis
- Autonomic failure
- Diabetes
- Parkinsons disease
- Prolonged bed rest
- Adrenal insufficiency
- Raised intrathoracic pressure
| Remember Decrease in baroreceptor sensitivity leading to postural hypotension is commonly seen in elderly patient |
Management
- Identify and treat cause
- Stop or adjust medications which may contribute to hypotension
- Pendant alarms - for old people
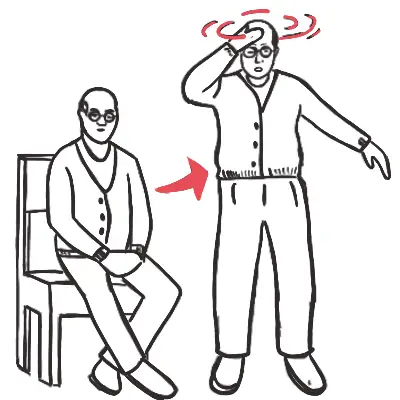
- Have patient modify behavior by standing slowly and step-wise, and lying down at prodrome.
- If patient is salt or water depleted (e.g., diuretics, diarrhea)
- Medications
- Alpha-1 agonists - midodrine
- Fludrocortisone
- Desmopressin
- Supplementary agents
| Postprandial hypotension is when blood pressure falls 1-2 hours after a meal due to inadequate sympathetic compensation to meal-induced pooling of blood in the splanchnic circulation →↓venous return to the heart → ↓ventricular filling → ↓cardiac output → (postprandial hypotension) |
Complications
- Supine Hypertension (nitroglycerin patch at night and remove in morning to help)