Achilles Tendinopathy & Rupture
Achilles tendinopathy & rupture are common causes of posterior ankle pain and disability, particularly in active adults. Tendinopathy presents with chronic pain, stiffness, and impaired function, while rupture is an acute injury characterised by a sudden “pop” and loss of plantarflexion power. Achilles tendon injuries are increasingly prevalent due to sports participation, with rupture incidence ~18/100,000 annually, most often in men aged 30–50 years.
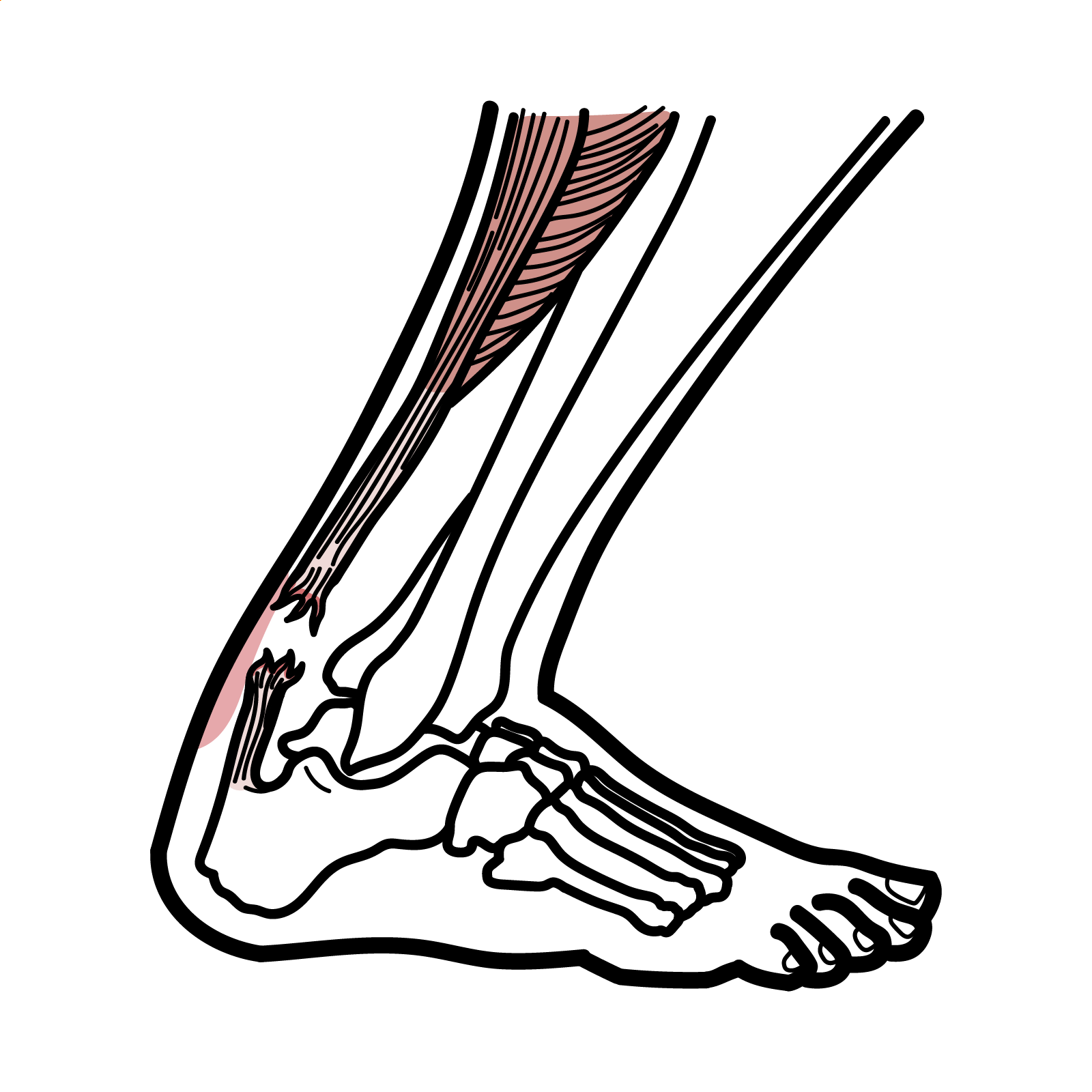
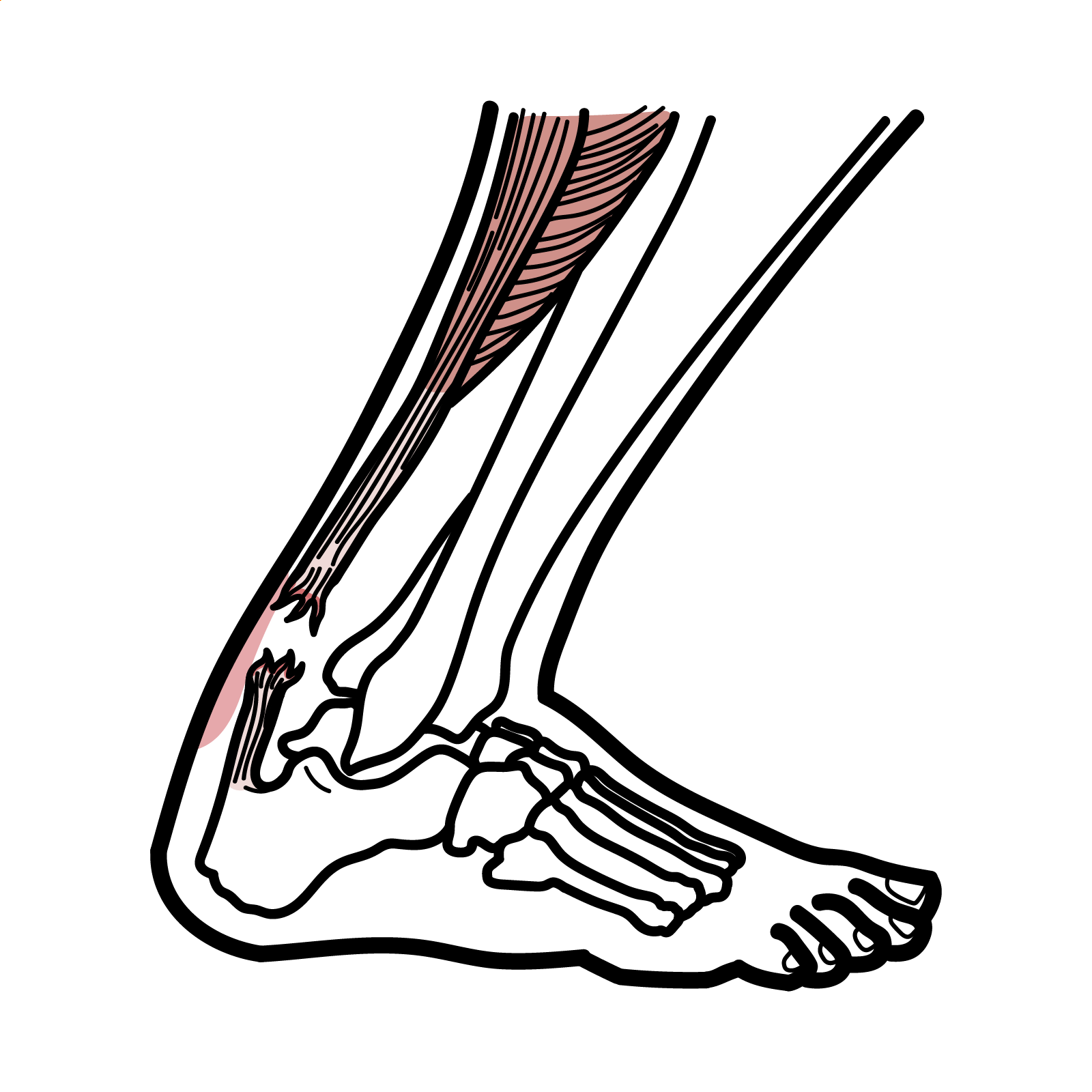
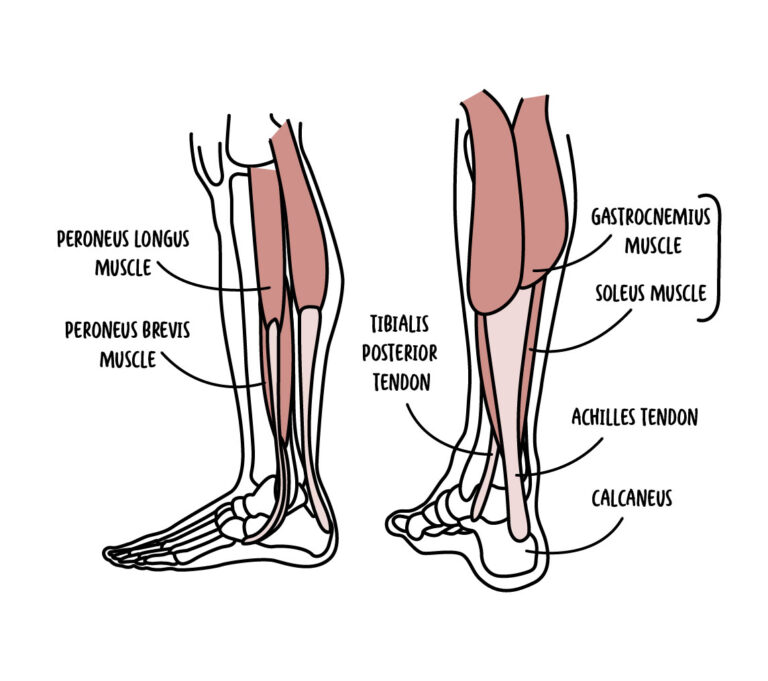
Achilles tendon: Convergence of gastrocnemius and soleus tendons inserting into calcaneus; strongest tendon in the body.
Tendinopathy: Chronic degenerative process of tendon collagen, not just inflammation.
Rupture: Complete disruption of tendon fibres.
Thompson test: Calf squeeze test; absence of plantarflexion = Achilles rupture.
Ruptures usually occur in the hypovascular “watershed zone.”
There are other causes of achilles tendon rupture other than sports. These include Quinolones (such as ciprofloxacin) and prolonged corticosteroid use.
Tendinopathy = chronic degeneration; rupture = acute overload failure.
A patient who thinks they’ve been “kicked in the back of the leg” but no one was there likely ruptured their Achilles.
Triad: Sudden “pop” in ankle, Palpable tendon gap, Positive Thompson test.
Achilles Tendinopathy vs Rupture
| Feature | Tendinopathy | Rupture |
| Onset | Gradual, chronic | Sudden, acute |
| Pain | Activity-related, morning stiffness | Sudden severe pain, may subside quickly |
| Exam | Thickened, tender tendon | Palpable gap, Thompson test + |
| Function | Pain but preserved strength | Loss of push-off, impaired walking |
| Imaging | US/MRI: thickened tendon | US/MRI: complete/partial discontinuity |
| Condition | Differentiator |
| Plantaris rupture | Pain more medial, intact plantarflexion |
| Retrocalcaneal bursitis | Local swelling, no tendon defect |
| Posterior ankle impingement | Pain with plantarflexion, no tendon abnormality |
Eccentric strengthening = gold standard for tendinopathy; surgery vs functional rehab depends on patient profile.
Delayed or missed rupture diagnosis → poor functional outcomes.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion