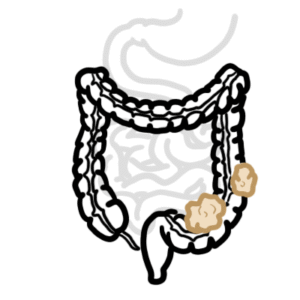
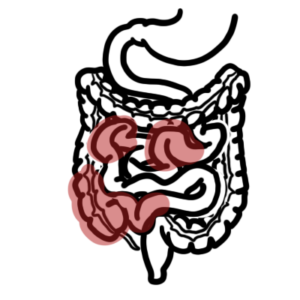
0:00 Acylasia is a rare disorder that results from progressive destruction of the 0:09 ganglion cells 0:10 in the myenteric plexus of the esophageal wall. 0:13 The destruction of these cells leads to the inability of the lower esophageal 0:17 sphincter 0:17 to relax and leads to the loss of peristalsis of the distal esophagus. 0:26 As a result, there is dilatation of the distal esophagus. 0:31 Patients often present with dysphagia, regurgitation, heartburn, reflux, and 0:38 weight loss. 0:39 Acylasia can occur at any age, but most likely diagnose in those ages 25 to 60 0:46 years old. 0:50 Now the esophagus is a muscular tube that transports swallowed solids and 0:54 liquids 0:55 from the pharynx to the stomach. 0:57 The esophagus has a similar structure to the rest of the gastrointestinal tract 1:02 , as it 1:02 consists of outer layer of connective tissue, the adventitia, two muscular 1:07 layers, an outer 1:09 longitudinal layer, and an inner circular layer, a submucosa, a mucosa 1:15 consisting of 1:16 non-teratinized stratified squamous epithelium, which is continuous with the 1:22 columnar epithelium 1:24 of the stomach. 1:26 The gastrointestinal tract is able to move food along and not backwards through 1:32 its intrinsic 1:34 peristaltic movements. 1:36 The intrinsic peristaltic movements are controlled by the enteric nervous 1:41 system, which is composed 1:43 of an outer plexus, the myenteric plexus, also known as the arbok plexus, and 1:49 then there's 1:50 the inner submucosa plexus, also known as the mice-ness plexus. 1:57 The myenteric, the obox plexus, lies between the longitudinal and circular 2:04 muscle layers 2:05 of the gut and exerts main control over gastrointestinal movements. 2:12 The inner mucosa plexus, the mice-ness plexus, is the main control of 2:17 gastrointestinal secretion 2:20 and local blood flow. 2:23 There are two esophageal sphincters, an upper and lower. 2:31 The lower esophageal sphincter is a muscle and its tone is controlled by the my 2:34 enteric 2:35 plexus. 2:36 The myenteric plexus consists of excitatory nerve cells, which contract the sph 2:41 incter, 2:42 preventing reflux of food and acids from the stomach. 2:46 The myenteric plexus also contain inhibitory nerve cells, which relaxes the sph 2:52 incter 2:52 when food travels down the esophagus to the stomach. 2:58 Important to know that the enteric nervous system is also partly controlled by 3:02 the central 3:03 nervous system. 3:04 The vagus nerve in the brainstem innervates the enteric nervous system, and so 3:09 do sympathetic 3:09 nerve fibers from the spinal cord. 3:13 From clinical pearls, gastroesophageal reflux disease is a common misdiagnosis 3:17 made in 3:18 patients with acylasia. 3:20 They are commenced on a proton pump inhibitor, and the time to diagnosis is 3:24 prolonged, leading 3:25 to poor patient outcomes. 3:29 Now the pathophysiology of acylasia is thought to be the result of loss of the 3:34 inhibitory 3:35 neurons in the myenteric plexus, of the distal esophagus, and the lower esoph 3:40 ageal sphincter. 3:41 That leads to unmatched excitation. 3:46 The excitatory cells in myenteric plexus release the neurotransmitter acylch 3:51 oline, which causes 3:53 smooth muscle contraction of the distal esophagus and the lower esophageal sph 3:58 incter. 3:59 Usually the inhibitory cells release vasoactive intestinal peptides, VIP, and 4:06 nitric oxide, 4:08 which have the effect of smooth muscle relaxation. 4:12 However, in the absence of vasoactive intestinal peptide and nitric oxide, due 4:19 to inhibitory 4:21 cell destruction, acylcholine from the excitatory neurons is unmatched. 4:28 The result of this imbalance is the failure of the lower esophageal sphincter 4:33 to relax 4:34 due to uninhibited contraction and loss of distal esophageal peristalsis. 4:42 Acylasia is also considered to be an autoimmune disorder, patients with acyl 4:45 asia have been 4:46 shown to have antibodies to myenteric cells in their circulation. 4:52 So the exact etiology of acylasia is unknown. 4:55 However, it is thought that acylasia can be due to idiopathic unknown cause, or 5:01 associated 5:01 with viral parasitic infections, autoimmune or neurodegenerative disorders. 5:08 Tripenosoma cruzi, the parasite that causes chagas disease, has been shown to 5:13 infect myenteric 5:14 neurons. 5:15 This in turn causes an immunologic reaction to myenteric nerve neurons, leading 5:20 to loss 5:21 of the esophageal and lower esophageal sphincter intramural ganglia. 5:26 In chagas disease, other parts of the gastrointestinal tract are also affected. 5:32 On a separate note, patients with serum antibodies to the herpes simplex virus, 5:36 human papilloma 5:37 virus, and the rubiola virus have been shown to have higher incidences of acyl 5:45 asia. 5:46 Important point to remember is that both myenteric antibodies and herpes simple 5:52 x virus 5:53 one antibodies are found in majority of patients with acylasia. 5:59 Patients with acylasia also have a 3-4 times higher risk to have another 6:06 autoimmune disease. 6:09 Patients with acylasia often present with dysphagia, occurring with both solids 6:14 and liquids, along 6:15 with non-acidic regurgitation of undigested food. 6:20 Additional symptoms include heartburn, weight loss, and chest pain, un 6:25 responsive to acid 6:26 reducing agents. 6:29 The initial investigation to order in patients with suspected neurologic cause 6:33 of dysphagia 6:34 is barium swallow, which shows dilation of the esophagus, with narrowing at the 6:40 lower 6:40 esophageal sphincter, known as a bird's beak appearance. 6:46 The diagnosis is confirmed by esophageal high-monometry testing. 6:51 Classically, the visual findings of acylasia on endoscopy include a dilated es 6:57 ophagus and 6:58 a puckered lower esophageal sphincter. 7:02 Endoscopy also reveal retained foods and saliva with no signs of mechanical 7:09 obstruction. 7:11 A small fraction, about 2-4% of patients who are suspected to have acylasia, in 7:15 fact have 7:16 pseudo-acylasia. 7:19 Pseudo-acylasia is due to an obstructed distal esophagus, from causes other 7:24 than destruction 7:25 of the myenteric plexus at the distal esophagus. 7:28 Rather, they are usually due to obstruction by a malignant mass, but also can 7:33 be due to 7:34 scleroderma, or a structure from ischemia, toxins, or reflux. 7:40 These responsible for pseudo-acylasia include gastric carcinoma, esophageal 7:46 carcinoma, and 7:47 lymphoma. 7:49 The pathophysiology of pseudo-acylasia is thought to be due to obstruction of 7:53 the distal esophagus, 7:55 secondary to growth of a tumor, and invasion of the tumor that causes den 8:01 ervation and 8:02 a functional obstruction in a manner similar to acylasia. 8:07 And pseudo-acylasia should be evaluated with CT or endoscopic ultrasound. 8:16 Now for treatment. 8:18 Approaches to treatment of acylasia include endoscopic or surgical intervention 8:23 with the 8:24 goal of lowering esophageal pressure, which then will hopefully relieve 8:29 symptoms. 8:30 Now endoscopic therapy involves injection of botulinum toxin, pneumatic d 8:37 ilation, or perioral 8:39 endoscopic myotomy. 8:42 Botulinum toxin injection into the lower esophageal sphincter inhibits acylch 8:47 oline release, causing 8:50 lower esophageal sphincter relaxation. 8:54 Toxin injection can be repeated, but becomes less effective. 9:01 Pneumatic dilation disrupts the circular muscle. 9:06 Clinical symptom improvement ranges from 50 to 90 percent, and the most common 9:11 complication 9:12 is perforation. 9:15 Perioral endoscopic myotomy is a newer endoscopic procedure in which the 9:20 physician creates an 9:22 esophageal submucosal tunnel, extending to the level of the lower esophageal sp 9:28 hincter, 9:29 and then performs a myotomy. 9:32 Studies have shown resolution of symptoms in over 80 percent of patients. 9:38 Surgical treatment consists of laparoscopic myotomy of the circular muscle 9:42 fibers. 9:42 Fund application is also recommended to avoid reflux symptoms after myotomy. 9:50 Surgical therapy is reserved for patients who are poor candidates for endoscopy 9:54 or surgical 9:54 therapy. 9:56 Lower esophageal sphincter pressure can be reduced with medical therapy, 10:00 including calcium 10:01 channel blockers such as nephitopene, or long-acting nitrates. 10:06 Patients with acylasia, for more than 10 years, have an increased risk of squ 10:11 amous cell carcinoma. 10:17 Thank you for watching, I hope you enjoyed this video.