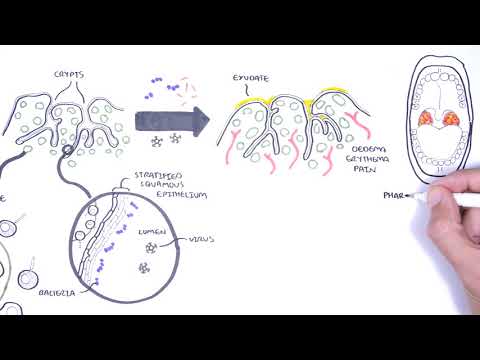
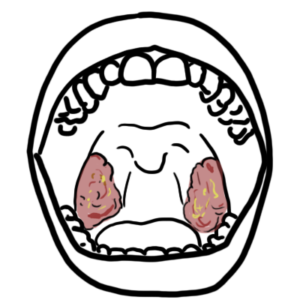
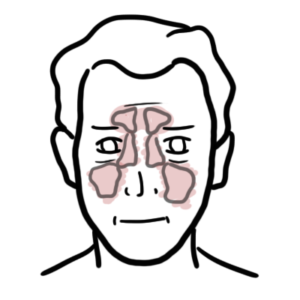
0:00 Hello, in this video, we're going to talk about acute tonsillitis. 0:08 Before delving into the condition, we need to learn about the anatomy. 0:13 The tonsils are part of what is called wilditis ring. 0:16 Generally, when talking about the tonsils, we're talking about the palatine 0:19 tonsils situated 0:20 on both sides of the throat. 0:22 There are also the adenoids, the tubal tonsils, and lingual tonsils, which make 0:26 up wilditis 0:27 ring. 0:28 The tonsils are a lymphoid organ containing macrophages, T cells, and B cells. 0:34 The immune cells here are important in learning and building up the immune 0:39 response. 0:39 The tonsils are important in the early years of life because the lymphoid 0:43 tissues containing 0:44 the immune cells are continuously exposed to many antigens. 0:49 So that is why until the age of six tonsils are typically hyperplastic, they're 0:54 big and 0:55 tend to regress, so shrink by 12 years of age. 1:00 The palatine tonsils have a strong blood supply from five different vessels. 1:05 That is why there is a risk of a lot of bleeding with tonsillectomy, removal of 1:12 the tonsils. 1:14 Zooming into the tonsils, we can see they have deep crypts and lymph nodules. 1:19 The crypts are normally colonized by many species of bacteria and also exposed 1:24 to many 1:25 viral organisms. 1:28 Then you have lymph nodules, which contain immune cells that are your T cells, 1:34 B cells, 1:34 and macrophages. 1:40 Many viral and bacterial organisms can cause tonsillitis, which is inflammation 1:44 of the tonsils. 1:48 Something tonsilare edema, hypertrophy, erythema, redness, and pain. 1:55 The inflammation may affect other areas of the back of the throat, including 1:58 the adenoids 1:59 and the lingual tonsils. 2:01 This inflammatory response produces eggs today, either white, gray, or yellow 2:07 discharge. 2:08 Cultures are not often useful in distinguishing the offending pathogens because 2:14 even if you 2:15 grow something, there are probably commensal organisms anyway, they live there 2:21 naturally. 2:22 Generally with acute tonsillitis, the pharynx is also inflamed, which is the 2:26 back of your 2:26 throat. 2:27 And so a better definition is Ferengo tonsillitis, rather than acute tonsill 2:33 itis. 2:33 In this video, we will use both terminologies. 2:36 Now the majority of cases of tonsillitis are caused by viruses. 2:41 Modern viral organisms that cause tonsillitis include embstined bar virus, EBV, 2:46 adenovirus, 2:48 rhinovirus, respiratory syncedial virus, influenza, and parenfluenza. 2:53 The most common bacterial causes of acute tonsillitis is group A streptococcus, 2:58 also 2:58 known as strep hiaogenes. 3:01 We will focus on the two most important clinical causes of acute tonsillitis. 3:07 That is, embstined bar virus and group A streptococcus, also known as strep hia 3:15 ogenes. 3:16 Let's begin by looking at EBV. 3:19 Now EBV, embstined bar virus, infection, is usually asymptomatic. 3:25 If EBV virus infection causes symptoms, it can be part of a condition called 3:29 infectious 3:30 mononucleosis. 3:32 So we'll be mainly focusing on infectious mononucleosis here. 3:36 And infectious mononucleosis most often begins insidiously with fatigue, vague 3:42 malaise followed 3:43 by several days later of sore throat, pharyngeotonsilitis, headaches, fever, 3:49 swollen posterior 3:50 cervical lymph nodes. 3:52 In some people, there can be hepatomegaly, leading to complications such as 3:58 hepatitis 3:59 and splinomegaly, which may present with splenic rupture. 4:06 Embstined bar virus is a virus that is part of the herpes family and is 4:10 transmitted via 4:11 saliva. 4:13 That is why EBV infection is also known as the kissing disease. 4:18 Once in the body, the embstined bar virus targets B cells in the oropharynx, 4:23 such as 4:23 in the tonsils. 4:25 And so in the tonsils, they replicate and conquer as the body builds up an 4:32 immune response. 4:33 Negations for infectious mononucleosis include a full blood count, which may 4:39 show lymphocytosis, 4:40 high lymphocyte count, thrombocytopenia, low platelets, and then you also want 4:46 to do 4:46 electro urea creatinine, liver function test and CRP. 4:51 A mono-spot test is a useful test to perform and is very quick. 4:56 A mono-spot test looks at heterophile antibodies, which are produced by those 5:03 abnormal B cell 5:04 infected by the Epstein-Barr virus. 5:08 Further investigations that can be performed include Epstein-Barr virus 5:12 specific antibodies 5:13 and throat swabs to look for differential diagnosis such as group A streptococ 5:23 cus. 5:24 And for symptomatic Epstein-Barr virus infection, which is infectious mononucle 5:30 osis, is usually 5:31 conservative and include pain and temperature relief using ibuprofen and par 5:37 acetamol, adequate 5:39 rest, fluids, and good nutrition. 5:43 Primary Epstein-Barr virus infection rarely require more than supportive 5:49 treatment. 5:49 Rarely, the enlarged tonsils will cause an airway obstruction. 5:56 But if it does happen, it is important to admit the person, and they will 6:02 likely need 6:02 E and T involvement. 6:05 Steroids are given to reduce swelling. 6:08 Then potentially a nasopharyngeal airway is required, intubation rarely, and 6:14 especially 6:15 emergency tonsillectomy or tracheostomy may be required, which is again rare. 6:21 Complications of Epstein-Barr virus infection include a splenic rupture, leuk 6:26 oplakia, berkits 6:27 lymphoma, lympho-chlorifative diseases as well. 6:32 In some cases, Epstein-Barr virus tonsilitis is treated with antibiotics 6:38 accidentally, 6:39 usually ampicillin, which when given in someone who has Epstein-Barr virus tons 6:46 ilitis will 6:47 cause a fine macular rash in up to 90% of people. 6:52 The mechanism is unknown. 6:55 Which leads to group A streptococcus, the bacterial cause of acute tonsilitis. 7:03 Group A streptococcus, or streptococcus pyogenes, is the most common bacterial 7:07 cause 7:08 of acute tonsilitis. 7:10 Ferengo tonsilitis caused by group A streptococcus is sometimes referred to as 7:14 strep throat. 7:16 The majority of episodes of pharyngitis are caused by viral infections as 7:20 discussed and 7:20 is usually treated conservatively. 7:23 However, early recognition of group A streptococcus is important since failure 7:28 to appropriately 7:29 treat someone who has strep throat may lead to group A streptococcus 7:33 complications. 7:34 But fortunately, distinguishing between viral and bacterial acute tonsilitis is 7:40 difficult. 7:41 The group A streptococcus are beta-hemolyticococci, able to produce some exotox 7:47 ins and 7:47 also contain many surface antigens that play a vital role in the pathophys 7:52 iology, such as 7:53 the M proteins. 7:56 Transmission of strep throat is through saliva and nasal secretion from an 8:00 infected person. 8:02 Here, group A streptococcus targets palatine tonsils. 8:06 However, it's also important to remember group A streptococcus is a common comm 8:11 ensal 8:12 organism as well. 8:18 Clinical features. 8:20 The incubation period of strep throat is usually two to five days of no 8:25 symptoms. 8:26 When symptoms do arise, bacterial tonsilitis causes sudden onset fevers, sore 8:32 throat, 8:33 pharyngitis and tonsilitis, which are red, enlarged, and have perlin exudate. 8:40 On the soft palate, you can also potentially see palat petique. 8:47 Here is a photo of strep throat. 8:50 Note the enlarged tonsils and exudate in yellow. 9:01 Other features of group A streptococcus tonsilitis include dysphagia, 9:06 difficulty swallowing, 9:09 odinophagia, pain when swallowing, and tender cervical limb fat anopathy. 9:15 On physical examination the pharynx is red, tonsils are red, and enlarged with 9:20 perlin 9:20 exudate. 9:22 A throat swab can be performed. 9:24 A throat swab with microscopic culture sensitivity in blood aga will help 9:30 diagnose group A streptococcus 9:32 because it will show a beta hemolytic coca. 9:36 The throat swab for rapid antigen detection tests are ADT can also be used. 9:43 In general though, throat swabs are not very useful because remember, group A 9:47 streptococcus 9:48 are commensal organisms in many patients. 9:53 Other investigations for group A streptococcus related tonsilitis include a 9:58 full blood count 9:59 which will show neutrophilia. 10:00 Now it's important concept to remember to help differentiate viral and 10:06 bacterial tonsilitis. 10:08 Remember lymphocytosis supports a viral cause of acute tonsilitis whereas neut 10:14 rophilia, 10:14 high neutrophil count supports a bacterial cause. 10:20 Early recognition and management is important to reduce complications 10:24 associated with group 10:25 A streptococcus throat infection. 10:28 The management for streptococcus throat infection are antibiotics, specifically 10:33 penicillin or 10:34 amoxicillin. 10:35 It's also important to monitor for complications of the antibiotics themselves. 10:41 So, when you give someone antibiotics with someone who has acute tonsilitis, 10:46 firstly, 10:47 if a rash eruption occurs, ask yourself, ask yourself, could this be a virus 10:52 penicillin 10:53 reaction which will support a diagnosis of Epstein-Barr virus tonsilitis rather 10:59 than 10:59 a bacterial tonsilitis, in which case you have to stop the antibiotics. 11:05 The second thing to think about is whether this could be a proper allergic 11:09 reaction to 11:09 the antibiotic, in which case you would have to stop the antibiotic and change 11:14 it, potentially. 11:16 The third thing is you have to ask yourself, could this be a complication of a 11:22 group A 11:22 streptococcus which is scarlet fever. 11:24 There they also get a rash everywhere. 11:28 Then you have other complications of group A streptococcus which we will not 11:32 talk about 11:33 in this video but can be seen in a video specifically on strept throat. 11:40 Important terminologies to remember regarding tonsilitis is something called 11:43 recurrent tonsilitis. 11:45 Now, sometimes people experience recurrent tonsilitis, up to several attacks of 11:50 acute 11:50 tonsilitis a year and no symptoms in between attacks. 11:55 Then you have chronic tonsilitis. 11:57 Sometimes people suffer from chronic tonsilitis which is when a sore throat is 12:02 present for 12:02 at least three months and is associated with tonsilla inflammation, halitosis 12:08 which is 12:08 smelly breath and persistent tender cervical lympharinopathy. 12:15 Chronic tonsilitis may also be associated with tonsillolith which are biofilms 12:19 that 12:20 form within the tonsillocrypts which leads us to the management of tonsillitis. 12:28 Obviously, we have the different causes, the viral and bacterial but you know, 12:33 sometimes 12:34 the tonsils have to be removed and this is called tonsillectomy. 12:38 Now there are specific indications for tonsillectomy and this is because first 12:43 ly, the tonsils play 12:45 an important role in the first 6 to 12 years of life with the whole immune 12:50 system business. 12:51 Secondly, because there are actually a lot of complications associated with 12:56 tonsillectomy 12:57 due to its anatomy and location, it's very important to follow the indications 13:04 for removing 13:05 the tonsils. 13:07 The indications for tonsillectomy include recurrent tonsillitis which means 13:13 several attacks I 13:15 think six in one year. 13:18 Having chronic tonsillitis, having a peritonecil abscess, tonsilloliths which 13:24 we mentioned 13:25 earlier, having obstructive symptoms, tonsillitis which causes obstructive 13:31 symptoms such as 13:33 an Epstein-Barr virus, for example, or something that will cause obstructive 13:40 sleep apnea. 13:42 And finally, a very important indication is suspected malignancy. 13:51 Tonsillectomy which is very important include general anesthesia associated 13:57 complications, 13:59 dental injury, temporal mandibular joint dislocation during the procedure, post 14:06 -operative bleeding 14:07 because remember there's a lot of blood supply to the tonsils, airway 14:13 obstruction causing 14:14 pulmonary edema as well as aspiration of any contents during the surgery. 14:21 So in summary, acute tonsillitis is inflammation of the tonsils. 14:25 The two most clinically important ones are tonsillitis caused by Epstein-Barr 14:29 virus and 14:30 Group A streptococcus. 14:32 But majority of acute tonsillitis are caused by viruses, just random viruses in 14:37 general. 14:38 Tonsillectomy is removal of the tonsils and have specific indications, but also 14:42 keep in 14:42 mind that there are complications associated with tonsillectomy. 14:45 Thank you for watching, I hope you enjoyed this video.