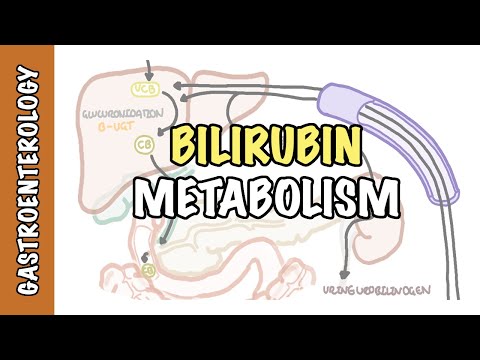
0:00 In this video, we're going to talk about bilirubin metabolism. 0:08 Bilirubin metabolism is important because hyperbilirubinemia is a condition 0:13 where you 0:14 have high amounts of bilirubin that can lead to jaundice, which is yellowing of 0:18 the skin 0:18 and of the eyes, for example, and this could indicate something sinister. 0:25 So bilirubin is formed by breakdown of heme present in hemoglobin. 0:32 So the story starts with an old red blood cell, which enters what's called the 0:36 reticuloendothelial 0:37 system, which is in your liver and in your spleen. 0:41 Here they are engulfed by macrophages. 0:44 The red blood cells contain many hemoglobin molecules, which are broken down to 0:50 heme and 0:50 globin, hence the name hemeoglobin. Heme is further broken down by two enzymes, 0:56 heme oxygenase, 0:58 followed by biliridin reductase, forming bilirubin and iron. 1:04 The iron and the globin is recycled to make more red blood cells. 1:14 The bilirubin formed is in an unconjugated form, so it's unconjugated bilirubin 1:20 , and 1:20 it is lipid soluble. And so it has to bind to something, and albumin is the 1:26 protein which 1:27 acts as a transporter. So this unconjugated bilirubin is bound to albumin, but 1:34 it also 1:34 can bind to other things such as high-density lipoproteins, and less often, it 1:39 can circulate 1:40 freely in an unbound form. Bilirubin is also formed by the breakdown of other 1:46 things such 1:46 as myoglobin and cytochrome enzymes. Anyway, this albumin bilirubin complex 1:54 circulates 1:54 around and then enters the liver system, where disassociates. The unconjugated 1:59 bilirubin 2:00 is taken up efficiently by the hepatocytes, while the albumin remains in 2:05 circulation. 2:06 Bilirubin enters the hepatocytes through facilitated diffusion, essentially 2:10 through a concentration 2:11 gradient. Here they undergo what is called glucuronidation. This process makes 2:19 substances 2:20 such as the bilirubin more water soluble, which allows it to be excreted in b 2:25 ile and 2:26 in urine. Glucuronidation is carried out by a family of enzymes called uredine, 2:35 diphosphoglycoronate, 2:38 glucuronosoltransferase, or UGT. In the case of bilirubin, it is bilirubin UGT. 2:49 The unconjugated bilirubin is now conjugated bilirubin and is water soluble. It 2:55 is secreted 2:56 into the bilirid system and is a component of bile. Conjugated bilirubin 3:03 travels down 3:04 the bile duct, where it joins with the pancreatic duct and into the duodenum 3:08 through the ampulovata. 3:11 The conjugated bilirubin is now in the small intestine, where it continues its 3:17 journey. 3:18 Majority of bilirubin here is conjugated, 98% obviously, and only a small 3:24 proportion 3:25 is unconjugated bilirubin. Conjugated bilirubin remember is water soluble and 3:32 so it is not 3:34 absorbed across the lipid membrane of the small intestinal epithelium. In 3:39 comparison, 3:40 the unconjugated bilirubin fraction is partially reabsorbed and undergoes inter 3:47 ohapatic circulation, 3:50 which is where it travels through the portal system back to the liver, so inter 3:55 ohapatic 3:56 liver circulation. This unconjugated bilirubin can then undergo glucuronidation 4:03 again to 4:03 become a conjugated bilirubin and water soluble. Going back to this conjugated 4:10 bilirubin actually 4:11 continues travelling to the large intestine, where it is exposed to so much 4:16 bacteria. Here, 4:17 the bilirubin is reduced by bacterial enzymes to a series of molecules termed u 4:22 robulinogens. 4:24 Urobulinogens are partly absorbed in the bowel and undergoes again interohap 4:33 atic circulation, 4:35 where the urobulinogen will enter the liver to get processed again. Now, the 4:42 fraction that is 4:43 actually not cleared by the liver will enter the general circulation and is 4:48 partly excreted in urine. 4:49 Urine bilinogen gives urine its yellow color. Majority of urobulinogens is 4:59 actually excreted 5:00 in feces. The urobulinogens here are further oxidized to form urobulins, 5:07 including a sturcobilin. 5:09 Oxidized urobulinogens, which I mentioned, gives feces its brown color. And so 5:18 that concludes the 5:21 basic metabolism of bilirubin. Now, jaundice is where you have high amounts of 5:29 bilirubin in the 5:30 blood, hyperbilirubinemia. And it can be either conjugated or unconjugated bil 5:37 irubin. 5:38 Clinically, hyperbilirubinemia can be divided into two major categories. You 5:45 have 5:45 unconjugated bilirubin mainly or conjugated bilirubin. So disorders, for 5:54 example, associated with 5:56 mainly unconjugated bilirubinemia include things that do not really involve the 6:02 liver. So for example, 6:05 dyserythropoasis, which is abnormality of red blood cell production. And so you 6:13 have a release 6:14 of bilirubin into circulation. Extravascular hemolysis, which is basically 6:20 death of the red 6:20 blood cells outside the vessels, leading to a release of unconjugated bilirubin 6:25 . Intravascular 6:27 hemolysis, similarly, is damage of the red blood cells within the vessel, 6:32 releasing the 6:33 unconjugated bilirubin. Extraversation, which is essentially when the red blood 6:38 cells go into the 6:41 tissues causing bruising and leakage of the bilirubin. Certain medications, 6:46 such as gentamycin and 6:48 some antiretroviral drugs, can elevate unconjugated bilirubin levels. And then 6:54 you also have gilbert 6:55 syndrome, which is deficiency in the bilirubin UGT mentioned earlier, which 7:01 means that you have 7:03 high amounts of unconjugated bilirubin and then yellowing of the skin. 7:15 Now, the second category of hyperbilirubinemia are disorders associated with 7:20 conjugated hyperbilirubinemia. 7:23 And this can be further divided into intrahepatic causes or posthepatic causes, 7:30 also known as 7:31 biliary obstruction. So focusing on the intrahepatic causes, these include 7:37 viral hepatitis, 7:38 alcoholic hepatitis, non-alcoholic steoter hepatitis, primary biliary colang 7:44 itis, 7:44 drugs and toxins, such as alkylated steroids, sepsis, perineoplastic syndromes 7:52 associated 7:52 with malignancies, such as renal cell carcinoma. They can cause something 7:57 called a stowfer syndrome. 8:01 TPN, postoperative patients, and this is multifactorial cause. 8:06 Liver infiltrations, so things such as amyloidosis, sarcoidosis, tuberculosis 8:14 can precipitate 8:15 intrahepatic cholestasis. The other group that causes high amounts of conjug 8:24 ated bilirubin include 8:26 biliary obstruction, also known as posthepatic causes. And this includes cholyl 8:32 ithiasis, 8:33 gallbladder adenocasinoma, biliary colangiocasinoma, ascending cholangitis, 8:42 which is really an 8:43 infection of the bilduct, primary sclerosis in cholangitis, 8:52 strictures after an invasive procedure such as an ERCP. Pancreatic cancer, 8:59 some parasitic infections can cause obstruction, lymphoma can cause obstruction 9:06 , 9:06 AIDS, cholangiopathy, acute and chronic pancreatitis is a very important cause. 9:11 So investigating jaundice, before learning about investigations, we need to 9:19 understand what 9:20 the liver function test blood test is. So the liver function test is to assess 9:25 your liver function 9:27 and we look at the bilirubin and also four main enzymes. So high bilirubin, as 9:34 we know, 9:34 leads to jaundice and there are many causes that we've learned. The first two 9:39 enzymes are the AST 9:41 and ALT, which are your transaminases and are predominantly found in the liver. 9:46 GGT and ALP are 9:48 enzymes found in the biliary system. So if AST and ALT go up, this signifies 9:54 liver tissue injury. 9:56 If GGT and ALP go up, this signifies a biliary tract injury or intra-happatic 10:01 abiliary duct problems. The initial investigation to order in someone with j 10:08 aundice is the liver 10:10 function test, including bilirubin but also albumin and also checking the 10:15 international 10:15 normalised ratio or INR. The bilirubin can then be further differentiated into 10:22 conjugated bilirubin 10:23 or un- conjugated bilirubin. In jaundice with un- conjugated bilirubin, the 10:30 liver function test 10:32 are not deranged. This is because there are usually due to problems with red 10:37 blood cells. 10:38 So in this scenario, consider ordering a hemolytic screep, including a full 10:44 blood count, 10:44 blood phillum, reticulocyte count, haptoglobin, lactate dehydrogenase, and the 10:52 coups test. 10:53 For conjugated bilirubin, think about intra-happatic causes of jaundice, 11:00 which will cause the LFTs to be deranged. The AST and ALT are typically high 11:08 because it's intra-happatic. High AST to ALT ratio signifies alcoholic 11:14 hepatitis, whereas high 11:16 ALT to AST mostly cause other liver diseases, including viral hepatitis. An 11:23 elevated INR with 11:26 low albumin would also indicate severe hepatic disease or dysfunction. 11:33 In this scenario, you have to continue and perform what's called a hepatitis 11:38 screen, 11:38 so you perform blood tests to look for other causes of liver disease, including 11:43 hepatitis B 11:44 and hepatitis C serology, autoimmune hepatitis, checking iron studies to look 11:49 for hemochromatosis 11:51 amongst many other things. For conjugated hyperbilirubin inemia and suspected 11:59 biliary obstruction, the conjugated bilirubin is high, and the liver function 12:04 test is also 12:04 deranged. The enzymes ALP and GGT are higher than the AST and ALT. For biliary 12:12 obstruction, 12:13 you need to do imaging to look for evidence of intra or extra-happatic bile 12:19 duct dilation. 12:21 So for example, doing a liver and biliary ultrasound, a CT abdomen, or an ERCP 12:27 and MRCP. 12:28 So in summary, we looked at an approach to jaundice, which is yellowing of the 12:33 skin and 12:34 the conjunctiva. Clinically, you have elevated bilirubin, which can be further 12:39 differentiated 12:40 into conjugated or un-conjugated bilirubin.