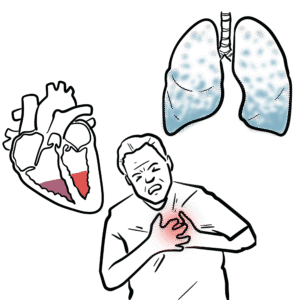
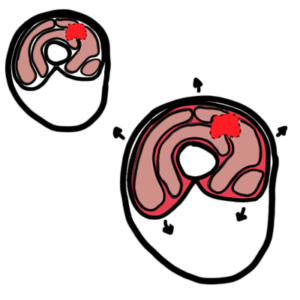
0:00 In this video, we will look at the autonomic nervous systems response to shock. 0:16 Shock is basically when the body, when the body tissues and organs are not 0:20 receiving 0:21 enough blood. 0:23 Shock is characterized by a sudden drop in blood pressure. 0:26 What we have to understand is that there are many types of shocks. 0:31 They are the same in that the result is a decrease in blood pressure, and also 0:36 that 0:36 there is not enough blood supply to body tissues and organs. 0:41 In this video, we will focus on cardiogenic shock, which is essentially shock 0:46 caused by 0:47 the heart failing to pump blood around the body, which means that there is not 0:52 enough 0:53 blood being received by body tissues and organs. 0:59 This hot failing to pump blood out is most often due to myocardial ischemia. 1:05 This is where the heart itself is not receiving enough oxygen, is not receiving 1:10 enough blood. 1:11 Let's take a closer look at myocardial ischemia first. 1:15 So here we have the blood vessels that supplies the hot, called the coronary ar 1:21 chery. 1:22 The coronary archery supplies the cardiac muscle cells with blood. 1:26 So here we have the red blood cells that carry oxygen. 1:31 And so if we have a plaque forming in the coronary archery, there is a block in 1:37 blood flow. 1:38 And so little to know blood is reaching these cardiac muscle cells, resulting 1:45 in ischemia. 1:46 Myocardial ischemia can lead to muscle cell death, because these muscle cells 1:52 are not 1:52 receiving any blood supply, any nutrients or energy. 1:56 Therefore, if the muscle cells die in the hot, we have pump failure. 2:03 And the hot is then unable to pump blood around the body, resulting in a 2:08 decrease in 2:09 blood pressure. 2:12 This also means that there will be not enough blood supplying tissues and 2:16 organs around 2:17 the body. 2:18 So there will be a decrease in oxygen and other nutrients supplying body 2:25 tissues. 2:26 Your body cells will begin to shift then from aerobic metabolism to anaerobic 2:32 metabolism, 2:33 because it is not receiving any oxygen, any red blood cells, due to the drop in 2:40 blood 2:40 pressure and the failing of the hot to pump blood to the tissues. 2:46 Anaerobic metabolism will result in an increase in lactic acid production. 2:52 After a while, an increase in lactic acid will lead to acidosis, which is 2:58 harmful and 2:59 dangerous for the body. 3:02 Now because the body's tissues are not receiving enough oxygen, there will also 3:06 be a decrease 3:07 in ATP production, why? 3:11 Well because oxygen is important in creating or producing a lot of ATP. 3:17 With a decrease in ATP production, cells will and can die due to no available 3:25 energy. 3:25 So there is cell necrosis. 3:30 Also in shock, because the cells are not receiving enough blood and because 3:35 there's bad blood 3:36 flow, you have an accumulation of carbon dioxide, waste essentially. 3:42 Carbon dioxide can actually react with water in the body to form hydrogen ions 3:51 and carbonate. 3:53 This is a normal physiological process, but if you have so much carbon dioxide, 3:59 there 3:59 will be a lot of hydrogen ions being produced, contributing or leading to acid 4:05 osis, which 4:06 as I mentioned, is very harmful for the body. 4:11 Okay, so those are some of the problems that can arise with shock. 4:18 And this also means cardiogenic shock. 4:22 So let's go back to the heart, which is suffering from ischemia. 4:27 So before we can see what the body tries to do in order to compensate for this 4:33 problem, 4:34 for this drop in blood pressure and this bad blood supply, we need to know some 4:39 anatomical 4:40 structures in the heart. 4:44 The aorta, which leaves the left ventricle, forms an arch, called the aortic 4:52 arch. 4:52 The first artery that branches off the aortic arch is the brachiocephalic 4:56 artery, which 4:57 then divides to form the right subclavian artery and the right common carotid 5:05 artery. 5:06 The right common carotid artery then branches on again. 5:11 The second artery that comes from the aortic arch is the left common carotid 5:17 artery, which 5:18 then branches into two. 5:21 The third artery that comes off the aortic arch is the left subclavian. 5:27 Another important thing to note are the nodes that actually orchestrate the 5:33 pumping of the 5:34 heart. 5:36 They form part of the conduction system. 5:40 So these nodes, these guys essentially are the ones that stimulates the heart 5:45 to keep pumping. 5:49 Now, again, the left ventricle here normally pumps blood to the rest of the 5:54 body through 5:55 the aorta. 5:57 But because this heart in particular is failing on the left side due to skimea 6:02 here, it can't 6:03 pump that much blood out of the heart. 6:07 When the heart can't pump much blood out, it means there is a decrease in what 6:12 's called 6:13 cardiac output. 6:15 A decrease in cardiac output means a decrease in mean arterial pressure, which 6:21 is pressure 6:22 in the arteries. 6:24 Now because there is not much pressure, this will cause a decrease in barore 6:31 ceptor firing. 6:33 So what does this mean? 6:35 Well, we have these special receptors called the baroreceptors. 6:43 These baroreceptors are stretch receptors, and we can find them here. 6:49 Here they are called the aortic arch baroreceptors. 6:52 And here they are called the carotid sinus baroreceptors. 6:57 So baroreceptors are stretch receptors. 7:01 When there is a lot of pressure, these receptors are stretched, and so they are 7:07 stimulated. 7:08 And therefore, they will fire many signals, essentially. 7:13 But when there is a decrease in pressure, such as what we see in shock, the bar 7:17 oreceptors 7:18 won't stretch as much. 7:20 And so they are not stimulated, and so they won't fire as much signals, 7:27 essentially. 7:29 And what does this mean? 7:30 Well, coming off these baroreceptors, there are sensory nerves. 7:36 There is one sensory nerve called the vagus nerve, which receives information 7:40 from the 7:41 aortic arch baroreceptor, and it will send this information to the medulla ob 7:49 longata, 7:50 which is a region in the brainstem here. 7:54 And then there is another sensory nerve that receives information from the car 8:00 otid sinus 8:01 baroreceptors, called the glossopharyngeal nerve. 8:06 And this will also send information, the signals, to the medulla as well. 8:12 So the medulla oblongata is a super important place, because within the medulla 8:17 there is 8:17 a cardioregulatory and vasomotor sensor, and we will learn more about it soon. 8:27 So here we are zooming into the section of a medulla. 8:31 And here we have a cross section. 8:33 In this section of the medulla oblongata, we have the cardioregulatory center, 8:39 which 8:40 is made up of the cardio-inhibitry center and the cardio-acceleratory center. 8:45 So here, and they are even on both sides. 8:50 So we have a, you know, on this side we also have a cardio-inhibitry center. 8:59 So let's step away from this diagram and just try to understand what the body 9:03 will try to 9:04 do when there is a decrease in baroreceptor firing due to a decrease in mean 9:10 arterial pressure. 9:13 So the goal is to increase mean arterial pressure. 9:17 So when there is a decrease in baroreceptor firing, two things will occur in 9:22 the medulla. 9:23 First is that there will be activation of the cardioregulatory center and vasom 9:30 otor center. 9:33 And at the same time, there will be an inhibition or unactivation of the cardi 9:39 oregulatory center. 9:42 Now the cardioregulatory center is the sympathetic nervous system. 9:47 The cardioregulatory center is the parasympathetic nervous system. 9:53 So when there is a, when the cardioregulatory center is not activated, there 9:59 will be a decrease 10:00 in parasympathetic activity. 10:02 And so there will be a decrease in vagus nerve activity because the vagus nerve 10:06 is the main 10:07 nerve of the parasympathetic nervous system. 10:12 So normally coming out of the cardioregulatory center here in the medulla, we 10:19 have the vagus 10:20 nerve, the motor vagus nerve that travels from the medulla to the conduction 10:26 system 10:27 of the heart. 10:29 And the aim of the motor vagus nerve is to slow the heart rate down. 10:34 But we don't want to do this. 10:38 So therefore, the sensory neurons that are coming to the medulla from the bar 10:44 oreceptors 10:45 will actually inhibit the cardioregulatory center. 10:50 So it will inhibit the motor vagus nerve from working essentially. 10:58 At the same time, this decrease in baroreceptor firing will stimulate the cardi 11:04 oregulatory center. 11:07 This means that it will stimulate the sympathetic nerve activity. 11:13 And there is a, there are a few, there's an early, there's an early and late 11:18 response. 11:19 The early response is that the sympathetic nerve will try to increase the heart 11:24 rate. 11:25 And also it will try, it will stimulate the release of adrenaline and noradrill 11:29 in from 11:30 the adrenal glands to cause vasoconstriction. 11:34 So let's look at this at a diagram to try to understand what's happening. 11:42 So these baroreceptors, these baroreceptor nerves that are coming to the med 11:49 ulla, will 11:52 inhibit the cardioregulatory center. 11:54 But at the same time, it will stimulate the cardioregulatory center. 11:59 So it will stimulate the sympathetic nerves. 12:04 This sympathetic nerve will travel down the spinal cord to the thoracic spine. 12:10 And then it will go out from the spinal cord. 12:14 It will synapse with another neuron in the sympathetic ganglion. 12:20 This post-sympathetic neuron will then travel to the conduction system of the 12:26 heart and 12:27 will stimulate the conduction system of the heart to increase in heart rate. 12:33 And therefore an increase in heart rate will cause an increase in cardiac 12:38 output to increase 12:40 mean arterial pressure. 12:42 At the same time the neurons, there are neurons in another region of the thorac 12:47 ic, another 12:48 sympathetic neuron in the thoracic that will essentially go out and stimulate 12:55 the adrenal 12:56 glands, which are found above the kidneys. 12:59 It will stimulate the adrenal medulla of the adrenal glands to secrete two 13:04 important 13:05 hormones, adrenaline and noradrenaline. 13:10 Adrenaline and noradrenaline will bind on receptors on veins and arteries. 13:16 It will bind on alpha receptors on veins and arteries to cause vasoconstriction 13:23 . 13:24 It will cause vasoconstriction to the arteries and veins all over the body 13:31 except in the 13:32 heart and brain because it wants blood to flow to these areas. 13:41 So what does vasoconstriction do? 13:45 Well, vasoconstriction will cause an increase in total peripheral resistance. 13:53 And therefore it will lead to an increase in mean arterial pressure because we 13:59 want to 14:00 increase mean arterial pressure. 14:04 So going back to this small mind map, we have the early response of the 14:09 sympathetic activity, 14:11 which is increase in heart rate and also the release of noradrenaline and 14:16 adrenaline to 14:17 cause vasoconstriction. 14:19 And then we have a mid to late response. 14:22 In the mid to late response, we have an increase in renin production as well as 14:28 an increase 14:29 in aldosterone production. 14:33 So what do these two molecules do? 14:37 Well going back to our spinal cord and sympathetic neurons, sympathetic neurons 14:42 can travel down 14:43 again to an region of the thoracic. 14:47 The sympathetic neuron will synapse with another neuron in the sympathetic gang 14:52 lion. 14:52 This postsynaptic, post-sympathetic neuron will travel to the kidneys and it 15:00 will stimulate 15:03 the kidneys to release an enzyme called renin. 15:08 Now what does renin do? 15:10 Well renin will travel in the blood. 15:14 Renin is an important enzyme to increase blood pressure. 15:19 How does it do this? 15:22 Well the liver produces a molecule called angiotensinogen which is a precursor. 15:29 Renin will convert angiotensinogen to angiotensin1 in the blood. 15:36 Angiotensin1 is not that cool but angiotensin1 can travel to the lungs where 15:43 there is a high 15:44 percentage of enzymes known as angiotensin converting enzyme. 15:51 So when angiotensin1 goes travels to the lungs angiotensin1 will convert to ang 15:57 iotensin2 15:58 by angiotensin converting enzyme ACE. 16:02 Angiotensin2 is such an important molecule in increasing blood pressure. 16:09 First of all it stimulates thirst which means that it will increase blood 16:15 volume resulting 16:16 in increasing blood pressure. 16:18 It also stimulates vasoconstriction. 16:23 If there is so much angiotensin2 being produced it will also cause cardiac 16:28 hypertrophy which 16:30 is long term but angiotensin2 main function that is very important is that it 16:37 actually 16:38 stimulates the adrenal glands will actually stimulate the adrenal cortex of the 16:45 adrenal 16:46 glands the outer part to release aldosterone which is a hormone that will 16:52 increase blood 16:54 pressure. 16:55 It does this by acting on the kidneys. 17:00 It causes the kidneys to increase potassium secretion in so more potassium in 17:07 urine but 17:07 it causes an increase in sodium reabsorption from the nephrons. 17:15 So an increase in sodium reabsorption means that more water is being absorbed 17:21 which means 17:21 that it will increase plasma volume increasing blood pressure which we want in 17:33 shock. 17:34 So there are all these responses occurring during shock from early to late 17:41 stage. 17:42 Another important thing to mention would be that there is another reflex you 17:51 can say 17:52 that the heart has which is the chemo receptor reflex. 17:56 See when there is a decrease in pH or there is a decrease in oxygen in the 18:01 blood and an 18:02 increase in carbon dioxide in blood this will stimulate the chemo receptors 18:08 which are situated 18:10 where the bowel receptors are. 18:13 When these chemo receptors are stimulated they will actually stimulate the 18:19 respiratory 18:20 center which will cause hyperventilation so you breathe quicker. 18:40 the body is not going to be able to breathe more.