Granulomatosis with polyangiitis – pathophysiology and management
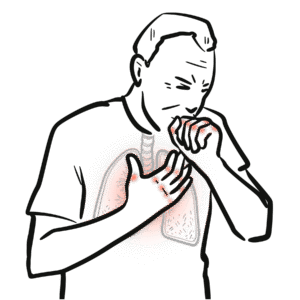
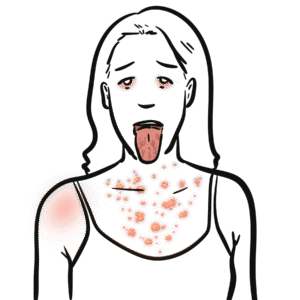
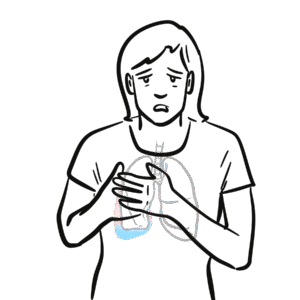
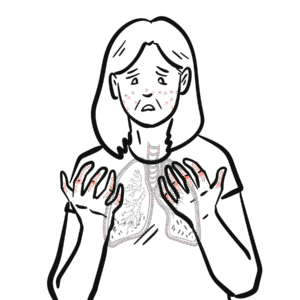
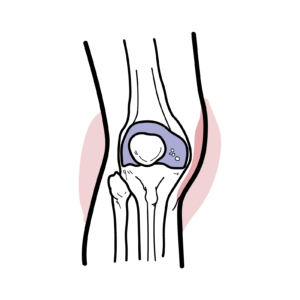
Granulomatosis with polyangiitis (Wegener’s) explained: learn causes, symptoms, diagnosis, and treatment of ANCA-associated vasculitis. ANCA-associated vasculitis targets small blood vessels and is driven by P-ANCA (anti-myeloperoxidase) or C-ANCA (anti-proteinase 3) antibodies; granulomatosis with polyangiitis (GPA) is the most common form and often ANCA-positive against proteinase 3. This video breaks down the hallmark Wegener’s triad—upper respiratory, lower respiratory, and renal involvement—covering granuloma formation, necrotizing small-vessel vasculitis, and common systemic signs like fever, arthralgia, cough, and weight loss.
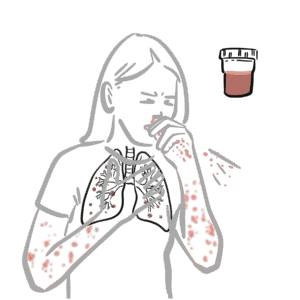
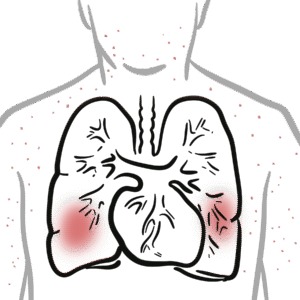
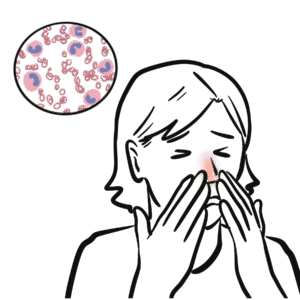
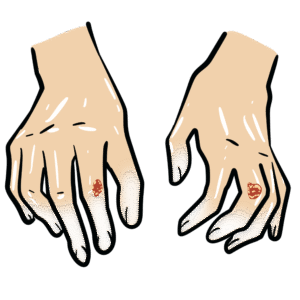
You’ll learn to recognize key clinical features: severe sinusitis, bloody nasal discharge and septal perforation with saddle-nose deformity; subglottic stenosis; pulmonary infiltrates, nodules, hemoptysis; ocular inflammation; and rapidly progressive glomerulonephritis causing hematuria and renal impairment. The summary details essential diagnostic steps—ANCA testing, full blood count, ESR/CRP, urinalysis, chest X-ray/CT, and confirmatory biopsy (skin or kidney)—and clarifies that ANCA titer magnitude doesn’t always match disease activity. Histology findings include granulomas, leukocytoclastic vasculitis, and pauci-immune glomerulonephritis with minimal immunoglobulin deposition.
Practical management guidance is provided: induction therapy with high-dose corticosteroids plus cyclophosphamide or rituximab, followed by maintenance with azathioprine, mycophenolate, or rituximab for 12–24 months after remission. Watch to gain a concise, clinically focused overview for diagnosis, imaging, biopsy interpretation, and immunosuppressive treatment strategies—essential for clinicians, trainees, and anyone seeking a clear guide to GPA. Learn the signs, tests, and treatments to act confidently and improve patient outcomes.