Hypercalcemia in malignancy – pathophysiology and management
Hypercalcemia in malignancy: understand causes, symptoms, and effective treatments for cancer-related high calcium levels. This video explains hypercalcemia in malignancy, why cancers cause elevated serum calcium, and how clinicians diagnose and manage it.
You’ll learn how parathyroid hormone (PTH) and PTH-related proteins drive bone resorption via RANK/RANKL-mediated osteoclast activation, and how tumors (breast metastases, multiple myeloma, lymphomas, renal cell and lung cancers) produce ectopic PTH or active vitamin D (calcitriol) to raise calcium. The transcript clarifies normal calcium physiology (albumin binding, normal range 2.25–2.65 mmol/L), diagnostic steps—start with PTH testing to distinguish primary hyperparathyroidism from malignancy—and key mechanisms: osteolytic lesions, PTHrP secretion, and vitamin D–mediated intestinal and renal calcium uptake.
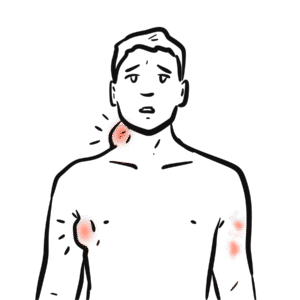
Benefit from a clear review of clinical features (“bones, stones, thrones, groans, and moans”)—bone pain, nephrolithiasis, polyuria/constipation, abdominal pain, neuropsychiatric symptoms—and practical, evidence-based management: aggressive IV normal saline for volume repletion and calciuresis, loop diuretics when needed, and bisphosphonates (zoledronic acid, pamidronate) to inhibit osteoclasts and restore calcium in most patients within days. For refractory or renal-impaired cases, learn when to use denosumab (anti-RANKL) or calcitonin to rapidly lower calcium. Watch to gain a concise, clinically focused guide to diagnosing causes, recognizing complications, and selecting appropriate therapies for hypercalcemia in cancer patients. If you manage oncology or acute medicine patients, this video equips you to act promptly and confidently.