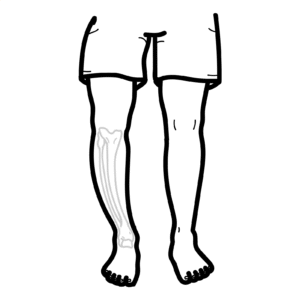
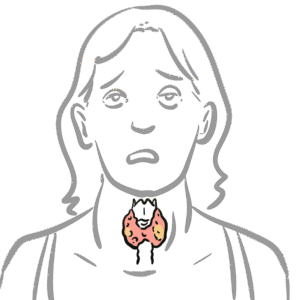
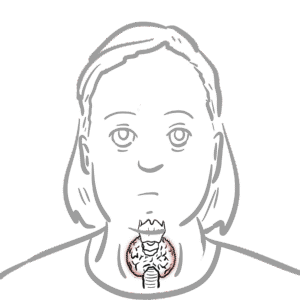
0:00 Hyperparathyroidism is characterized by abnormally high parathyroid hormone 0:12 levels in the blood 0:13 due to overactivity of the parathyroid glands. 0:17 It is differentiated into three types based on the underlying cause. 0:21 There's primary hyperparathyroidism, there's secondary hyperparathyroidism and 0:26 tertiary 0:26 hyperparathyroidism, which is a result of prolonged persistent secondary hyper 0:33 parathyroidism. 0:35 Let's focus on a normal physiology of the parathyroid hormone first. 0:42 Parathyroid hormone is synthesized and produced from the parathyroid gland, 0:47 which sits at 0:48 the back of our thyroid gland, and it's produced in response to low calcium 0:54 levels 0:54 and high phosphate levels in blood. 0:58 Parathyroid hormone has important effects on calcium and phosphate homeostasis, 1:07 and its 1:07 aim is to essentially increase blood calcium levels and reduce blood phosphate 1:13 levels. 1:14 In order to do so, parathyroid hormone affects three main organs. 1:19 In the bones, the parathyroid hormone promotes bone resorption through the 1:23 actions of osteoclasts 1:24 - osteoclasts are the bone-eating cells which will release calcium and 1:29 phosphate from the 1:30 bone into the blood. 1:34 Parathyroid hormone also targets the kidneys, increasing calcium reabsorption 1:39 but decreasing 1:40 phosphate reabsorption. 1:43 The net effect of parathyroid hormone is thus to increase blood calcium levels 1:49 and decrease 1:50 phosphate levels. 1:53 Parathyroid hormone also targets an enzyme in our kidneys, one alpha hydroxyl 1:58 ase, which 1:59 promotes the conversion of something called calcidiol to calcitryol, which is 2:06 the active 2:07 form of vitamin D. Active form of vitamin D is also known as 125-dihydroxych 2:14 olicalcyphrol, 2:16 which I've abbreviated here. 2:20 The active vitamin D will target the gut, increasing calcium and phosphate 2:31 absorption. 2:33 The production of active vitamin D has a negative feedback on the parathyroid 2:38 gland, telling 2:38 it to ease up the production of parathyroid hormone because it no longer 2:44 requires this. 2:45 Similarly, the elevated levels of calcium and low phosphate levels in the blood 2:51 has a negative 2:52 effect to the parathyroid gland, telling it, "Hey, thank you for your job. 2:58 Your job is done here and the body doesn't really need any parathyroid hormone 3:02 right 3:03 now." 3:09 Hyperparathyroidism happens when you have abnormally high parathyroid hormone 3:15 levels and there are 3:15 three types. 3:20 Primary hyperparathyroidism is one of the most common causes of hypercalcemia, 3:26 high calcium 3:26 levels in the blood. 3:28 The most common cause of primary hyperparathyroidism is an adenoma, which is 3:32 usually a benign growth, 3:34 followed by hyperplasia, or of the glands, or when you have multiple adenomas. 3:41 Rarely, a carcinoma or a men syndrome type 1 and type 2 can cause primary hyper 3:49 parathyroidism. 3:51 Whatever the cause, you get a growth, essentially, of the parathyroid gland, 3:57 which leads to overproduction 3:59 of the parathyroid hormone, and this leads to, essentially, increases the 4:05 calcium levels 4:07 in the blood and decreases the phosphate levels in the blood. 4:11 Now the negative feedback system is ineffective. 4:14 The negative feedback system is ineffective because despite the high levels of 4:19 calcium 4:19 and vitamin D, the adenoma or the abnormal growth, it doesn't respond to this 4:25 and will 4:25 still be active and produce parathyroid hormone. 4:33 Patients with primary hyperparathyroidism will have high parathyroid hormone 4:38 levels, hypercalcemia, 4:40 and they will try to compensate for this by peeing out calcium, so they will 4:46 show hypercalciria. 4:48 They will also pee out phosphate leading to hypophosphatemia, low phosphates in 4:53 the blood. 4:56 The treatment of primary hyperparathyroidism is a parathyroidectomy, removing 5:01 the parathyroid 5:02 glands. 5:03 Now if this fails or contraindicated, then calcium emetics can be used, and 5:09 calcium emetics 5:10 are essentially calcium mimics, they mimic calcium, so the body thinks that it 5:18 has more 5:19 calcium, and because of this, the parathyroid gland also thinks it has really, 5:25 really high 5:25 levels of calcium and so it will respond by reducing parathyroid hormone 5:34 secretion. 5:36 Primary hyperparathyroidism is a completely different ballgame. 5:40 Think chronic kidney disease and low vitamin D levels for this. 5:50 You see with chronic kidney disease, it causes a few changes in our body and 5:54 one of the big 5:55 changes is that it impairs excretion of phosphate and as a result you get hyper 6:03 phosphatemia, 6:05 which is high levels of phosphate in the blood. 6:08 Secondly, chronic kidney disease reduces the biosynthesis of vitamin D, which 6:13 will lead 6:13 to hypochalcemia. 6:26 Hypochalcemia and mainly hyperphosphatemia will stimulate the parathyroid gland 6:32 to produce 6:33 parathyroid hormone, because the body is screaming out for more calcium and 6:38 wants to get rid 6:39 of the phosphate in the blood. 6:46 Patients with chronic kidney disease do good for some time, attempting to 6:50 correct the hypochalcemia 6:52 and attempting to correct the hyperphosphatemia, but as chronic kidney disease 7:00 progresses it 7:00 becomes more difficult. 7:06 Remember, also that there is a negative feedback of vitamin D, well the 7:11 negative feedback here 7:13 does not exist, which means that there is less break on parathyroid hormone 7:18 release, 7:18 so you get elevated parathyroid hormone levels as well. 7:23 Another cause of secondary hyperparathyroidism, aside from chronic kidney 7:28 disease is vitamin 7:29 D deficiency, either from low sun exposure, poor diet, or an underlying disease 7:36 , and of 7:36 course malnutrition. 7:41 The features of secondary hyperparathyroidism include hyperparathyroidemia, 7:47 which is high 7:48 levels of parathyroid hormone in the blood, normal calciumia or hypochalcemia, 7:54 and most 7:55 importantly, hyperphosphatemia, as a result of chronic kidney disease. 8:02 The treatment of secondary hyperparathyroidism is treating chronic kidney 8:07 disease, having 8:08 a low phosphate diet, using phosphate binders, and ergo calciferol. 8:14 Ergo calciferol addresses the vitamin D deficiency, or low vitamin D levels. 8:25 Phosphate binders, such as psevelemia, will bind to phosphate in the gut, 8:31 reducing absorption 8:33 of phosphate, leading to reduced serum phosphate levels, and this will 8:39 hopefully reduce parathyroid 8:40 hormone secretion. 8:48 Now, after some time, patients with persistent secondary hyperparathyroidism 8:58 can have tertiary 9:00 hyperparathyroidism. 9:03 Tertiary hyperparathyroidism is caused by persistent secondary hyperparathyroid 9:10 ism. 9:11 What happens here is that, remember, the low calcium, and especially the high 9:17 phosphate 9:17 levels in the blood, will continue to stimulate the parathyroid gland, causing 9:24 hyperplasia, 9:25 essentially. 9:26 The glands will continue to be active, and eventually, it will become its own 9:33 boss and 9:33 doesn't listen to anything that's going on in the body. 9:37 It produces parathyroid hormone continuously, leading to hypercalcemia, and 9:43 because you 9:44 have still pre-existing chronic kidney disease, you will have hyperphosphatemia 9:51 . 9:51 The high calcium levels will try to have a negative effect on the parathyroid 9:56 gland, 9:57 but despite the hypercalcemia, the hyperplastic and active parathyroid gland 10:02 will continue 10:03 to produce parathyroid hormone. 10:06 But to mention that you also still have that hyperphosphatemia, which will 10:10 stimulate parathyroid 10:11 hormone release, therefore, the features of tertiary hyperparathyroidism is 10:21 very high parathyroid 10:24 hormone levels in the blood, hypercalcemia, and hyperphosphatemia. 10:30 The hyperphosphatemia, remember, is a result of chronic kidney disease. 10:37 Treatment of tertiary hyperparathyroidism is the same as primary hyperparathy 10:42 roidism, which 10:43 is surgery, and if not, calcium imidix. 10:47 I hope you enjoyed this video on hyperparathyroidism. 10:50 Thank you for watching.