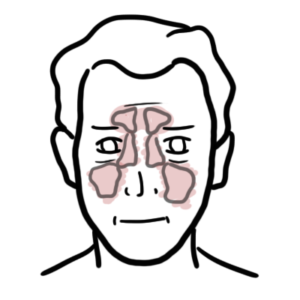
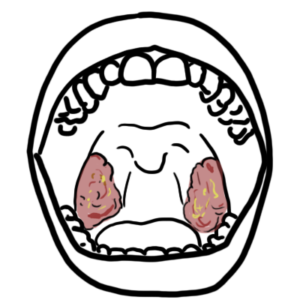
0:00 Hello in this video we're going to talk about the anatomy and the physiology of 0:10 the salivary 0:11 glands. We have three types of salivary glands, bilaterally, all of which 0:18 produce saliva. 0:19 The salivary glands produce saliva, which is essentially going to enter into 0:24 the oral 0:24 cavity located around here where the tongue is. Now sitting below the tongue 0:30 you have 0:30 the two sublingual salivary glands. Under the mandible, your lower jaw to the 0:36 back of 0:37 the mouth, you have the two sub mandibular salivary glands. And then you have 0:43 the bilateral 0:44 parotid glands, which is the largest salivary gland, sitting sort of posterior 0:49 to the mastor 0:49 muscle and anterior to the sternocleidoid mastoid muscle. Each salivary gland 0:57 have ducts 0:57 which drain into the oral cavity, the mouth. The parotid duct here, the sub 1:03 mandibular 1:04 duct, and the sublingual ducts drain into the oral cavity. Here is the mastata 1:10 muscle 1:10 again, which sits anterior to the parotid gland. Salivar is produced and secret 1:17 ed into the 1:18 mouth, producing an alkali substance. Interestingly, the sub mandibular gland 1:25 produces the majority 1:26 of the saliva, roughly 70%. Second is the parotid glands, which is about 25% of 1:34 salivar 1:35 production. Let's zoom into the structure of the salivary gland and look at how 1:43 everything 1:43 works. The functional unit of the salivary glands is called a salivon. A saliv 1:51 on consists 1:52 of asinacels, which produces this isotonic secretion. And this is the first 1:59 part of saliva 2:00 production. Surrounding these asinacels are myoepithelium, which can contract 2:07 moving the 2:08 fluid produced by the asinacels towards the ducts. Here, along the ducts, the 2:19 fluid flows, 2:20 and these ducts cells will reabsorb sodium chloride, but it will not reabsorb 2:27 the water, 2:28 making the saliva more hypotonic. The saliva has three main functions, lubric 2:37 ation, 2:38 protection, and there's a few ways. One way is that it contains lysosomes, 2:42 which attack 2:44 the bacterial cell walls, lactofarin, which chelates iron, and iron is normally 2:49 needed 2:50 by many bacteria for replication, and also it can contain IgA, which is an 2:57 immunoglobulin, 2:58 and helps in the immune response. The final function is digestion, because 3:05 saliva contains 3:06 amylase and lingual lipase, which helps break down carbohydrates and fats, 3:14 respectively. 3:16 Some clinical anatomy, Shrogan's disease, is a systemic autoimmune disorder, 3:21 most commonly 3:22 presenting with sicka symptoms. Sicka refers to dryness, most often involving 3:29 the eyes, mouth, ears, and even nose, all of which are due to inflammation and 3:35 resultant 3:36 pathology of the lacrimal and salivary glands. Shrogan's disease is a rheumat 3:44 ological disease 3:46 and is associated with other rheumatological conditions, including rheumatoid 3:54 arthritis. 3:55 Salivar is produced by the salivary glands, of which we have three pairs. So 4:01 what stimulates 4:02 saliva secretion? Well, salivation is stimulated by thought, sight, smell, and 4:12 taste. Sleep, 4:14 dehydration, fatigue and fear all inhibit salivation. The salivary gland have 4:22 different nerves which 4:23 supply it. In the brainstem, you have the pond and medulla region, and here you 4:29 can find 4:30 the superior salivatory nucleus and inferior salivatory nucleus. The part of 4:36 the nervous 4:37 system responsible for the rest and digest response, and so saliva production 4:44 is the 4:44 parasympathetic nervous system. The salivatory nucleus have parasympathetic 4:50 neurons targeting 4:52 the salivary glands via glossopharyngeal nerve and the facial nerve. Orig 4:58 inating from the 5:00 salivary nucleus in the pond, you have the facial nerve passing through the par 5:05 otid gland 5:06 and synapsing with the second neuron at the sub-mandibular ganglion. This 5:12 second neuron 5:12 is what will supply the sublingual and sub-mandibular gland, increasing parasy 5:17 mpathetic tone causing 5:19 salivation. From the inferior salivatory nucleus, the parasympathetic tone is 5:26 via the glossopharyngeal 5:28 nerve which synapses with the second neuron at the optic ganglion. From here, 5:33 the nerve 5:33 will stimulate parotid glands to produce saliva. When we think of parasymp 5:40 athetic nervous system, 5:41 we need to think about acetylcholine. Let's see how these neurons stimulate the 5:45 salivation 5:46 process. On the acetyls, you have receptors on the basal surface. These 5:54 receptors are 5:54 muscurinic receptors, three or even one. The parasympathetic tone of the saliv 6:02 ary glands 6:03 are controlled by cranial nerve nine and seven, and these guys will secrete 6:08 acetylcholine. 6:09 Acetylcholine binds onto muscurinic receptors in the area causing sodium and 6:14 water to enter 6:16 the loom in producing isotonic fluid, which is the initial part of the saliva 6:21 production. 6:22 Thus, by inhibiting muscurinic receptors or inhibiting this interaction between 6:30 acetylcholine 6:31 and the receptor, you can really cause dry mouth. So, clinical pharmacology, 6:38 looking at drugs and 6:39 the dry mouth. So, many drugs can cause a dry mouth. Remember, the parasymp 6:44 athetic neurons secrete 6:45 acetylcholine, which binds onto muscurinic receptors on the basal surface of 6:50 the asinac cells. 6:52 This causes salivation. Anticholinergics are drugs that block the action of 6:57 acetylcholine. 6:58 Atropene is one example. Atropene works by mimicking acetylcholine, and thus it 7:06 can bind onto 7:07 this muscurinic receptor, preventing the actual acetylcholine to bind onto the 7:11 receptor, 7:13 thus causing a dry mouth. Diuretics is another drug that works indirectly to 7:18 cause a dry mouth, 7:19 by causing an increase in fluid excretion, thus reducing fluid volume, which 7:25 can lead to a dry mouth. 7:26 Other medications that are important causes of dry mouth are anti-psychotics, 7:32 sympathetic memetics, and cytotoxic drugs. 7:39 The parotid gland is an important gland because many conditions can cause it to 7:44 become inflamed, 7:44 a term called parotitis. Also, parotid tumors can occur, requiring what's 7:52 called a parotidectomy, 7:54 which is the removal of the parotid gland. Normally, parotidectomies come with 8:00 no complications, 8:01 but there are some rare complications, including what's called bell's palsy. 8:06 And this is caused 8:07 by cranial nerve 7, the facial nerve injury, during the operation. Injury to 8:13 the facial nerve on the 8:14 affected side causes weakness of the muscle of facial expression on that side. 8:21 Remember, 8:21 the cranial nerve 7 or the facial nerve passes through the parotid gland, and 8:27 anatomically, 8:28 the parotid gland is divided into the deep and superficial lobes, which are 8:33 separated by the 8:34 facial nerve. Phrase syndrome is another interesting complication of parotidect 8:41 omy, 8:41 and this is caused by auriculotemporal nerve injury, which is a branch of cran 8:48 ial nerve number 5, 8:50 which is the trigeminal nerve. Injury to the auriculotemporal nerve will cause 8:57 the affected side to have ghostatory sweating, which is symptoms of profuse 9:04 head and neck 9:04 diaphoresis and flushing with eating. Here is an image of a patient that has 9:12 facial nerve 9:13 palsy or bell's palsy on the right side. As you can see, when asked to smile, 9:19 the right side of 9:20 his face, the muscles are weak. Here is a photograph of a person that has had a 9:26 left 9:26 parotidectomy as seen by the scar. When this person eats, he has ghostatory 9:35 sweating, where you have 9:36 flushing as well as sweating on the affected side, and this is due to injury to 9:42 the auriculotemporal 9:45 nerve, a branch of the trigeminal nerve. This condition is called Phrase 9:51 syndrome.