Coeliac Disease
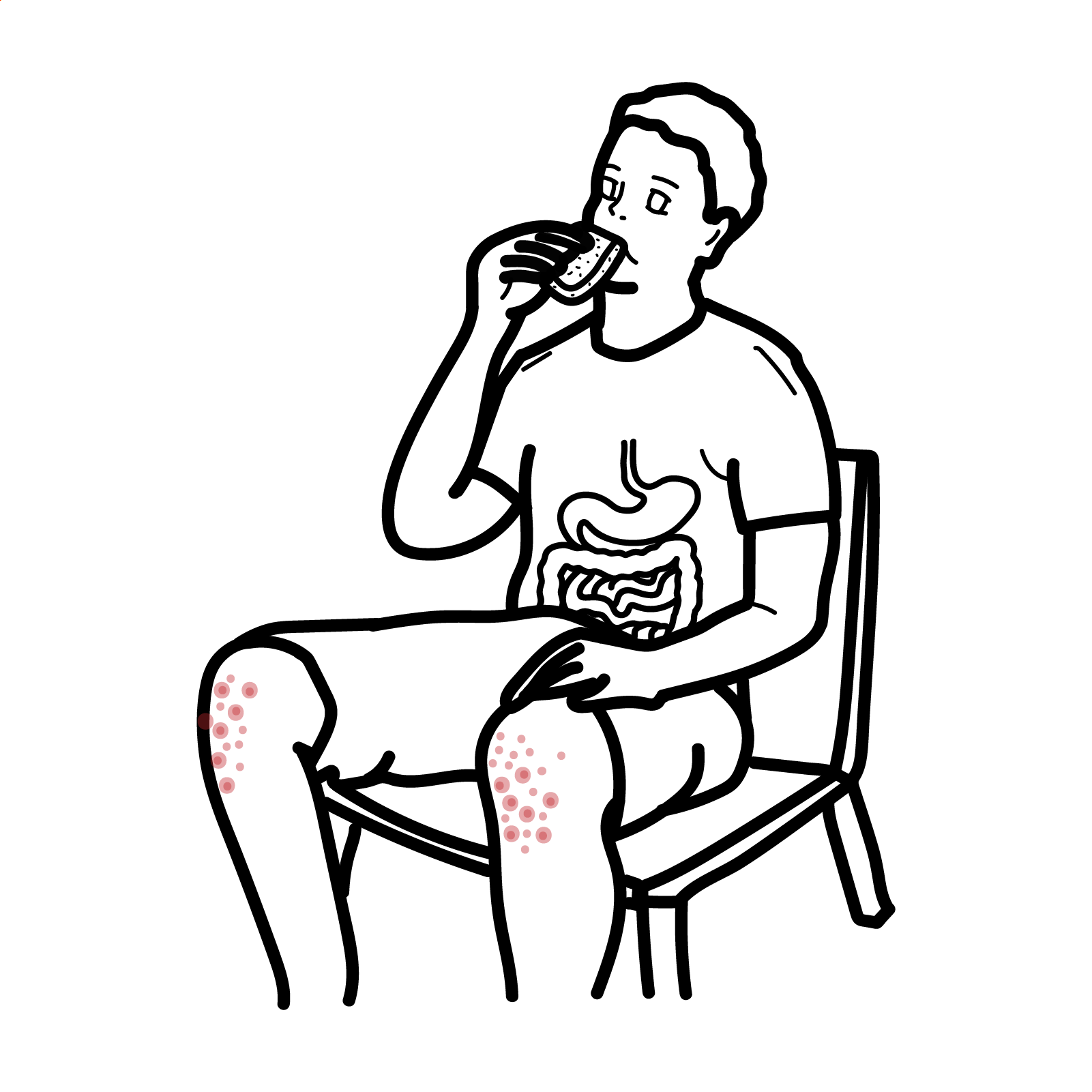
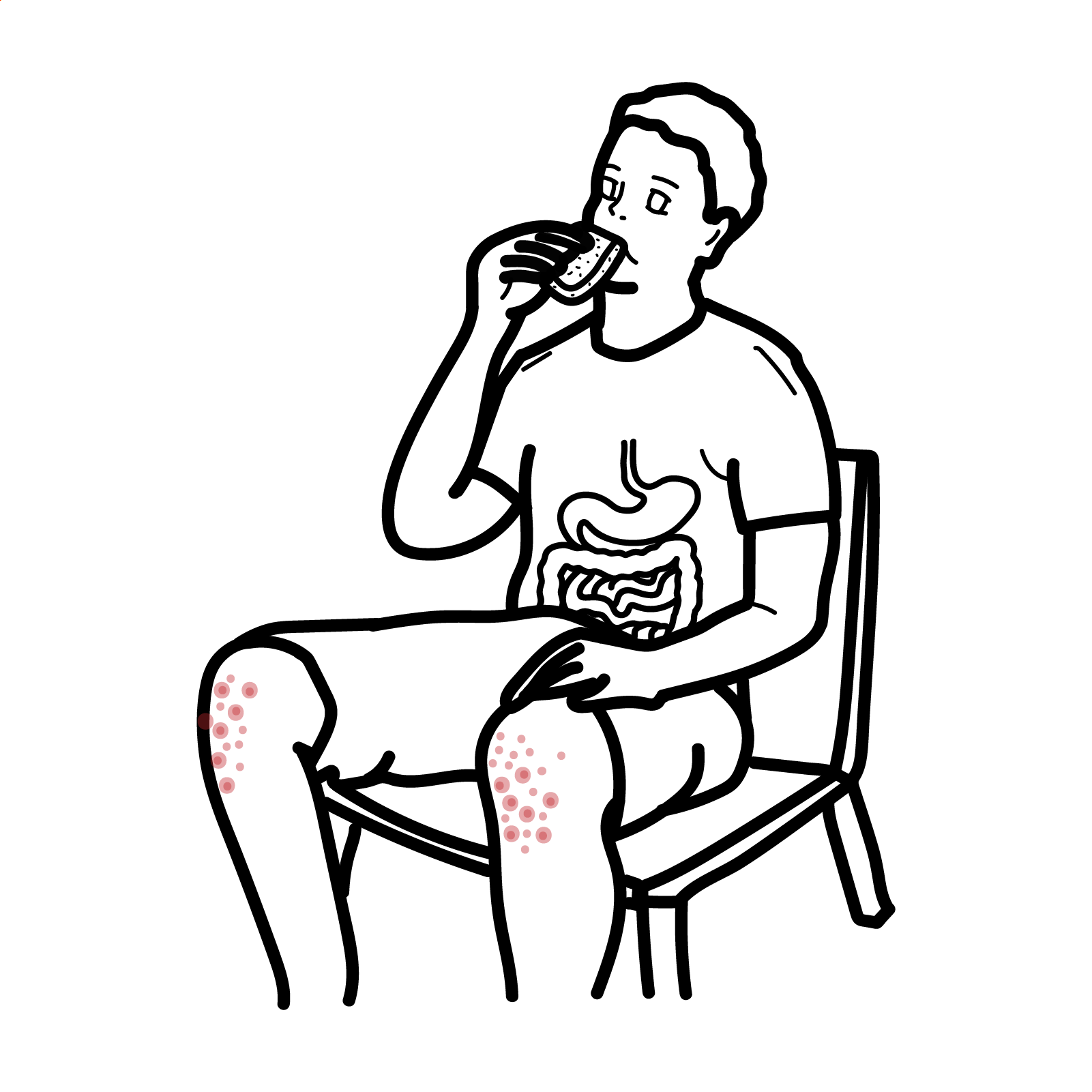
Coeliac disease is a systemic autoimmune disease triggered (T-lymphocytes) by dietary gluten peptides found in wheat, rye, barley, and related grains. Immune activation in the small intestine leads to villous atrophy, hypertrophy of the intestinal crypts, and increased numbers of lymphocytes in the epithelium and lamina propria. Locally these changes lead to gastrointestinal symptoms and malabsorption. The disease is common (1/~1000) and is more common in the Irish.
Coeliac Disease: Inflammatory process, which occurs in susceptible individuals in response to the ingestion of wheat protein (gluten and gliadin)
Gliadin: A glycoprotein (a carbohydrate plus a protein) within gluten
The small intestine is divided into three sections: Duodenum, Jejunum and Ileum.
The three sections of the small intestine
Blood Supply (branches of the celiac trunk)
Blood supply (3/5 branches of the superior mesenteric artery)
Physiology
Macroscopic
Microscopic
Risk Factors
Clinical Presentation
Coeliac disease is associated with Type II diabetes (10%) and Genetic disorders such as Down’s Syndrome (12%).
Clinical Examination – Usually normal, signs are seen in severe cases
Suspect Coeliac Disease in all those with diarrhoea + weight loss or anaemia (esp. if iron or B12).
Childhood other food-sensitive enteropathies (milk sensitivity)
Adults
Exclude coeliac disease in all diagnosed with irritable bowel syndrome.
Diagnosis Small Bowel Histological changes including:
General
Coeliac crisis management – Medical Emergency
Complications
Dermatitis Herpetiformis: Very itchy/“burning” blisters on elbows, scalp, shoulders, ankles

Prognosis
A Colour Handbook of Gastroenterology
Oxford Clinical Handbook of Clinical Medicine
Sleisenger and Fordtran’s Gastrointestinal and Liver Disease 10th Ed.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion