Overview
Complex chronic syndrome characterised by recurrent abdominal pain and bowel dysfunction, in the absence of a structural abnormality. It is not associated with an increase in mortality, however, it is associated with substantial morbidity and a significant decrease in an individual’s quality of life.
| Definition IBS IBD |
IBS belongs to a group of disorders collectively known as Functional Gastrointestinal Disorders. Functional Gastrointestinal Disorders are disorders of the digestive system where symptoms occur without structural or tissue abnormality. IBS is more common in Females (Female to Male Ratio = 2:1). There is a 2 fold increase in the prevalence of IBS among individuals who have relatives affected by IBS.
| Side note Other Functional Gastrointestinal Disorders:Functional HeartburnFunctional dyspepsiaFunctional BloatingFunctional Abdominal Pain SyndromeChronic Functional ConstipationChronic Functional DiarrhoeaGastroparesisBelchingHiccups. |
The population prevalence of IBS is high (∼11%) and the condition has considerable consequences for quality of life (QOL) that are comparable to other chronic diseases, such as diabetes mellitus and hepatitis.
Risk Factors
- Age <50 years
- Female Gender
- Previous Enteric Infection
- History of physical and / or sexual abuse
- Family history of mental illness/substance abuse
- Stressful life events
- Illness behaviour
- Abdominal surgery
- Antibiotic use
- Diverticular disease (left)
- Abdominal obestiy
- Endometriosis
Signs and Symptoms
General
| Classic Triad: Abdominal pain, diarrhea, and constipation. |
IBS is often associated with other somatic comorbidities (for example, pain syndromes, overactive bladder and migraine), psychiatric conditions (including depression and anxiety) and visceral sensitivity.
Red flags
- >50yo onset of IBS like symptoms
- Blood on the toilet paper or PR Bleeding
- Anaemia
- Unintendedweight loss
- Fever
- Family history of colon or ovarian cancer
- Major change in symptoms
- Nocturnal Symptoms
Differential Diagnosis
- Coeliac Disease
- Lactose Intolerance
- Inflammatory Bowel Disease - Crohn’s Disease or Ulcerative Collitis
- Infective Colitis
- Lymphocytic Collagenous Colitis
- Colon cancer
- Drug effects (e.g. Proton Pump Inhibitors, NSAIDS, metformin)
- Choledocholithiasis
Investigations
- FBC
- CRP
- Coeliac disease markers
- Colonoscopy
Diagnosis
Diagnostic criteria for irritable bowel syndrome (IBS) include recurrent abdominal pain or discomfort at least 3 days per month in the past 3 months associated with two or more of the following:
- Improvement with defaecation
- Onset associated with a change in the frequency of stool
- Onset associated with a change in the form (appearance) of stool
These changes have to be present at least 6 months after onset of symptoms.
Pathophysiology
The pathophysiology of IBS is unclear. There are no specific anatomical, endoscopic, microbiological or histological findings that indicate a clear pathophysiology.
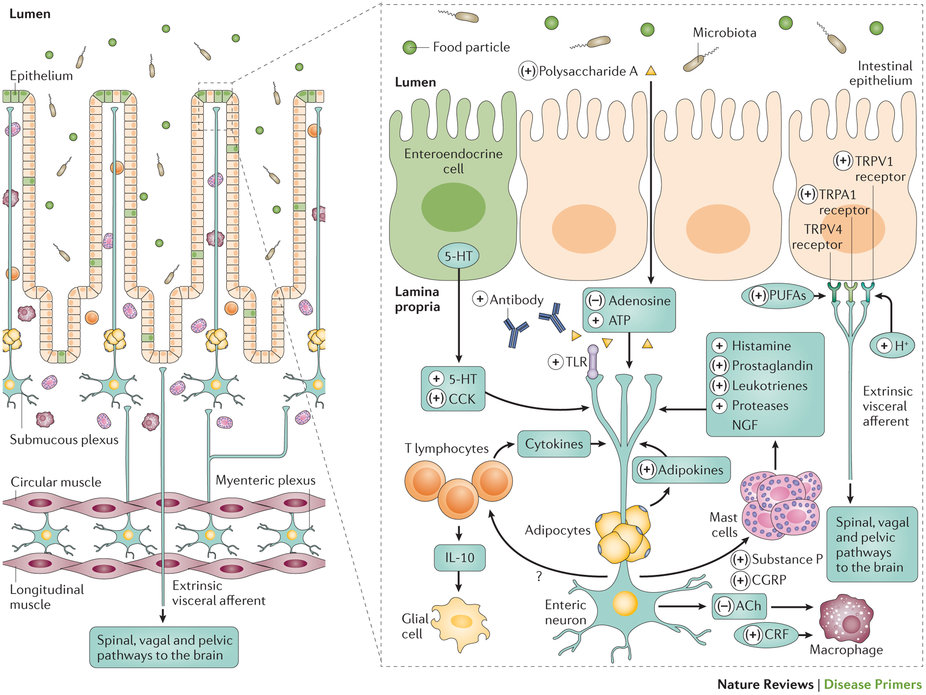
According to current understanding, IBS arises due to multiple factors that contribute to alteration of:
- The Brain-gut axis: Bidirectional communication between the brain and the GIT. Involves the ANS, the neuroendocrine system and neuroimmune pathways
- Gut sensitivity: Sensation of the GIT.
- Gut reactivity: Mobility and secretion of the GIT.
- Psychological functioning
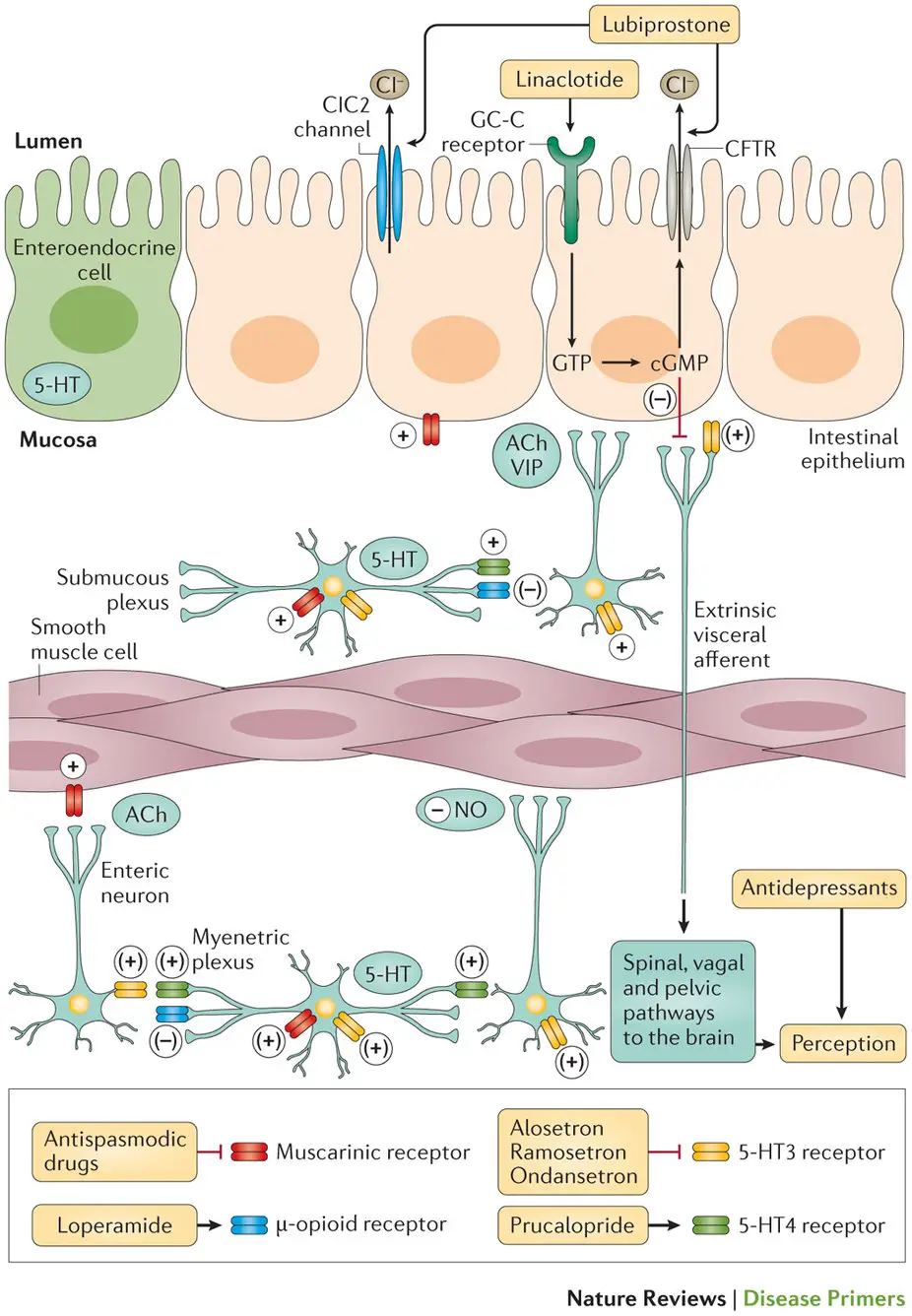
Management
Only a fraction of patients with IBS-like symptoms (∼50%) seek medical care
- Education and reassurance
- Dietary alterations
- Pharmacotherapy
- Behavioural and psychological therapy