Overview
Knee osteoarthritis is a chronic, whole-joint disorder characterized by pain, stiffness, functional limitation and progressive structural change affecting cartilage, subchondral bone, synovium, menisci, ligaments and peri-articular muscles. Prevalence rises with age and obesity and contributes substantially to global disability; recent GBD analyses and reviews highlight knee OA as a leading cause of pain and years lived with disability worldwide. Clinically, diagnosis is often made without imaging using validated rules, and core first-line care is education + exercise + weight management.
Definition
Osteoarthritis: a symptomatic, heterogeneous, whole-joint disease with mechanical, inflammatory and metabolic drivers rather than “wear-and-tear” alone.
Kellgren–Lawrence (K-L) grade: radiographic severity scale (0–4) based on osteophytes, joint-space narrowing, sclerosis and deformity (classification, not required for diagnosis).
Bone marrow lesion (BML): MRI high-signal subchondral change linked to pain and progression in KOA.
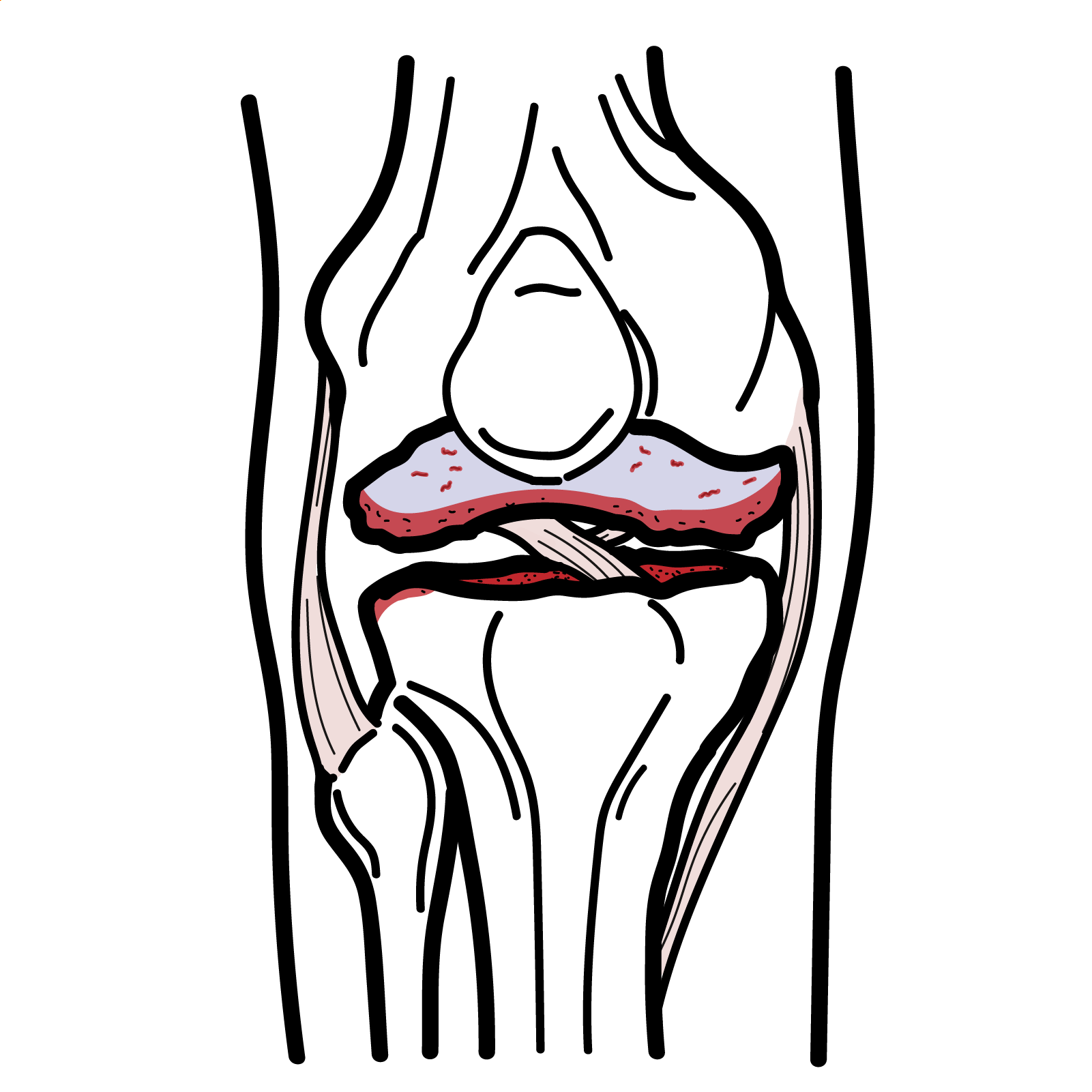
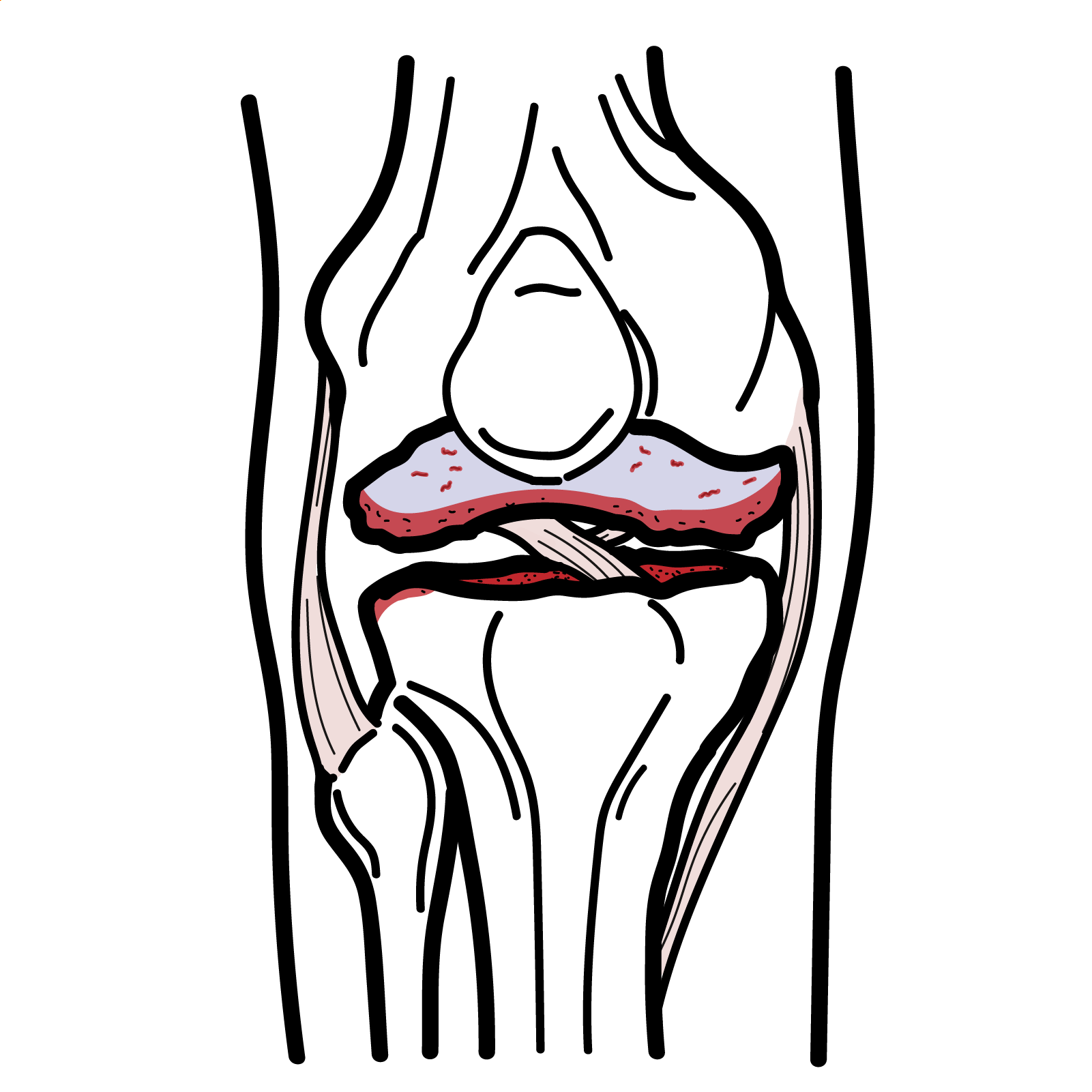
Anatomy & Physiology
- Joint surfaces: femorotibial (medial/lateral) and patellofemoral compartments lined by hyaline cartilage; menisci distribute load and enhance stability; collateral and cruciate ligaments constrain translation/rotation.
- Synovium: regulates nutrient exchange and produces hyaluronan-rich fluid for lubrication; can mount inflammatory responses.
- Subchondral bone: shock absorption and load transfer; communicates with cartilage via osteochondral channels.
- Neuromuscular control: quadriceps, hip abductors and calf musculature modulate joint loading; alignment and gait mechanics determine compartmental stresses.
Lubrication combines fluid-film and boundary layers—movement is protective when dosing is gradual and controlled.
Aetiology and Risk Factors
Aetiology (multifactorial, interacting “whole-joint” mechanisms)
- Mechanical: abnormal joint loading (varus/valgus malalignment, meniscal loss) drives focal degeneration.
- Biological: low-grade synovitis, subchondral remodeling and BMLs; nociceptive and nociplastic pain contributions.
- Metabolic: obesity/adipokines and insulin resistance increase risk and symptom burden.
Risk factors
- Non-modifiable: age; female sex; genetics/family history.
- Modifiable: overweight/obesity; prior knee injury (e.g., ACL/meniscus); high occupational kneeling/squatting/lifting; malalignment; low muscle strength; physical inactivity.
Treat prior-injury knees as “secondary prevention” targets (strength, alignment, load).
Pathophysiology
- Joint load mismatch (demand > capacity) → focal cartilage matrix damage + meniscal stress.
- Synovial activation (cytokines, neuropeptides) → pain and effusion; central sensitization in some.
- Subchondral bone remodeling and BMLs → nociceptor ingrowth/angiogenesis → pain and structural progression.
- Malalignment/deconditioning perpetuate compartmental overload → osteophytes, joint-space loss, functional decline.
BMLs and synovitis correlate best with weight-bearing pain—guide both rehab and injection decisions.
Clinical Manifestations
- Activity-related knee pain (walking, stairs, squatting)
- Short morning stiffness (<30 min)
- “giving way”
- Crepitus and swelling
- Reduced function and confidence
- Flares after load spikes
- Nocturnal pain in advanced disease
Functional features
- Slower timed-up-and-go
- Difficulty rising from chair
- Reduced walking endurance
- Reduced balance.

This image series is only available to members
Diagnosis
Diagnose clinically without imaging when all present—age ≥45, activity-related pain, no morning stiffness or stiffness ≤30 minutes; image if atypical features or red flags.
Label early and start core rehab—do not delay for x-ray.
Imaging
- Weight-bearing AP/lateral and skyline views to classify and plan
- Radiograph severity by K-L grade
- MRI not routinely required—consider if alternative pathology suspected
- US can detect effusion/synovitis and guide injections
Imaging severity (K-L) ≠ symptom severity; target impairments and goals, not x-ray grade.
Classification
- By compartment: medial/lateral tibiofemoral; patellofemoral; mixed.
- By radiograph: Kellgren–Lawrence 0–4 (0 normal → 4 severe with marked joint-space loss and deformity).
- By phenotype (useful clinically): biomechanical–malalignment/instability; inflammatory/synovitis-dominant; metabolic–obesity; bone-driven (BML-dominant); pain-sensitization predominant.
Treatment
- Education
- Structured exercise (strength—esp. quadriceps/hip; aerobic; neuromuscular/balance; tai chi)
- Weight loss if overweight/obese (goal ≥5–10%)
- Pacing and flare plan
Devices/adjuncts
- Cane in contralateral hand
- Knee taping
- Tibiofemoral unloader bracing for unicompartmental OA
Pharmacologic (use lowest effective dose, shortest duration, alongside exercise)
- Topical NSAIDs (first-line)
- Oral NSAIDs + PPI if needed; acetaminophen limited benefit
- Duloxetine conditional for persistent pain
- Topical capsaicin optional
- Avoid routine opioids
Intra-articular therapies
- Corticosteroid: short-term relief for flares; avoid frequent repeat courses (signals of cartilage loss with repeated triamcinolone).
- Hyaluronic acid (no good evidence)
- PRP/stem cells: evidence inconsistent; many guidelines advise against outside research/specialist settings.
Interventional pain
- Radiofrequency ablation (genicular nerves): conditional option in refractory knee OA
Surgery
- Do not perform arthroscopy for primary degenerative knee disease (no meaningful long-term benefit).
- Consider realignment osteotomy (younger, unicompartmental malalignment) or unicompartmental/total knee arthroplasty for severe, function-limiting disease after optimal non-surgical care.
Infections offer a short-term role; avoid frequent repeats (possible cartilage loss signal with repeated steroids).
No single exercise is superior—the best plan is the one they’ll do consistently.
Complications and Prognosis
Complications
- Functional decline
- Falls/deconditioning
- Analgesic adverse effects (GI/CV with NSAIDs; dependence with opioids)
- Post-injection flare
- Accelerated progression in some with repeated IA steroids
- Surgical risks after arthroplasty
Prognosis
- Variable course; many stabilize/improve with sustained exercise and weight loss
- Poor prognostic factors
- Obesity
- Varus/valgus malalignment
- Prior major knee injury
- Severe baseline radiographic/structural damage
- Depression/low self-efficacy
The strongest modifiable levers are weight loss and ongoing exercise.
Acronym
- KNEE-OA = Kilos down (weight loss) + NSAIDs (topical → oral) + Exercise (strength/aerobic/balance) + Education/self-management + Offload (brace/tape/cane) + Adjuvants (IA steroid short-term; duloxetine) — escalate to surgery if refractory. (NICE, Arthritis Foundation)
References
- National Institute for Health and Care Excellence (NICE). Osteoarthritis in over 16s: diagnosis and management (NG226). London: NICE; 2022. (NICE)
- Kolasinski SL, Neogi T, Hochberg MC, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of OA of the Hand, Hip, and Knee. Arthritis Care Res (Hoboken). 2020;72(2):149-162. (Arthritis Foundation)
- Bannuru RR, Osani MC, Vaysbrot EE, et al. OARSI guidelines for the non-surgical management of knee, hip, and polyarticular OA. Osteoarthritis Cartilage. 2019;27:1578-1589. (ScienceDirect)
- American Academy of Orthopaedic Surgeons (AAOS). Management of Osteoarthritis of the Knee (Non-Arthroplasty). 3rd ed. 2021. (aaos.org)
- EULAR. Evidence-based recommendations for the diagnosis of knee OA. Ann Rheum Dis. 2024. (EULAR)
- Hunter DJ, Bierma-Zeinstra S. Osteoarthritis. Lancet. 2019;393:1745-1759. (acpacprogram.ca)
- Oo WM, Hunter DJ, et al. Bone marrow lesions in osteoarthritis: recent advances. Skeletal Radiol. 2024;53:—. (SpringerLink)
- Hall M, et al. Risk factors for incident knee OA: systematic review. Osteoarthritis Cartilage. 2025;—. (oarsijournal.com)
- Filbay SR, et al. Risk of knee OA after knee injury in youth. Br J Sports Med. 2020;54(12):725-—. (bjsm.bmj.com)
- Siemieniuk RAC, et al. Arthroscopic surgery for degenerative knee arthritis and meniscal tears: guideline. BMJ. 2017;357:j1982. (BMJ)
- EULAR 2024 update—non-pharmacological core management of hip/knee OA. Ann Rheum Dis. 2024;—. (ard.bmj.com)
- AAFP. Osteoarthritis Management: Updated ACR Guidelines. Am Fam Physician. 2021;103(2):120-122. (AAFP)
- Radiopaedia. Kellgren and Lawrence system for classification of OA. 2025. (Radiopaedia)
- EULAR recommendations for imaging in OA clinical management. Ann Rheum Dis. 2017;76:1484-1494. (eprints.whiterose.ac.uk)
- The Knee Journal. K-L grade and morphological parameters. 2019. (thekneejournal.com)
- Kolasinski SL, et al. ACR/AF guideline—hyaluronic acid conditional against. Arthritis Care Res (Hoboken). 2020;72:149-162. (acrjournals.onlinelibrary.wiley.com)
- NICE NG226 Visual Summary. 2022. (NICE)
- McAlindon TE, et al. Intra-articular triamcinolone vs saline and cartilage volume. JAMA. 2017;317:1967-1975. (JAMA Network)
- GuidelineCentral summary of AAOS: lavage/debridement not recommended. 2021. (Guideline Central)

Discussion