Paediatric Respiratory Distress Syndrome
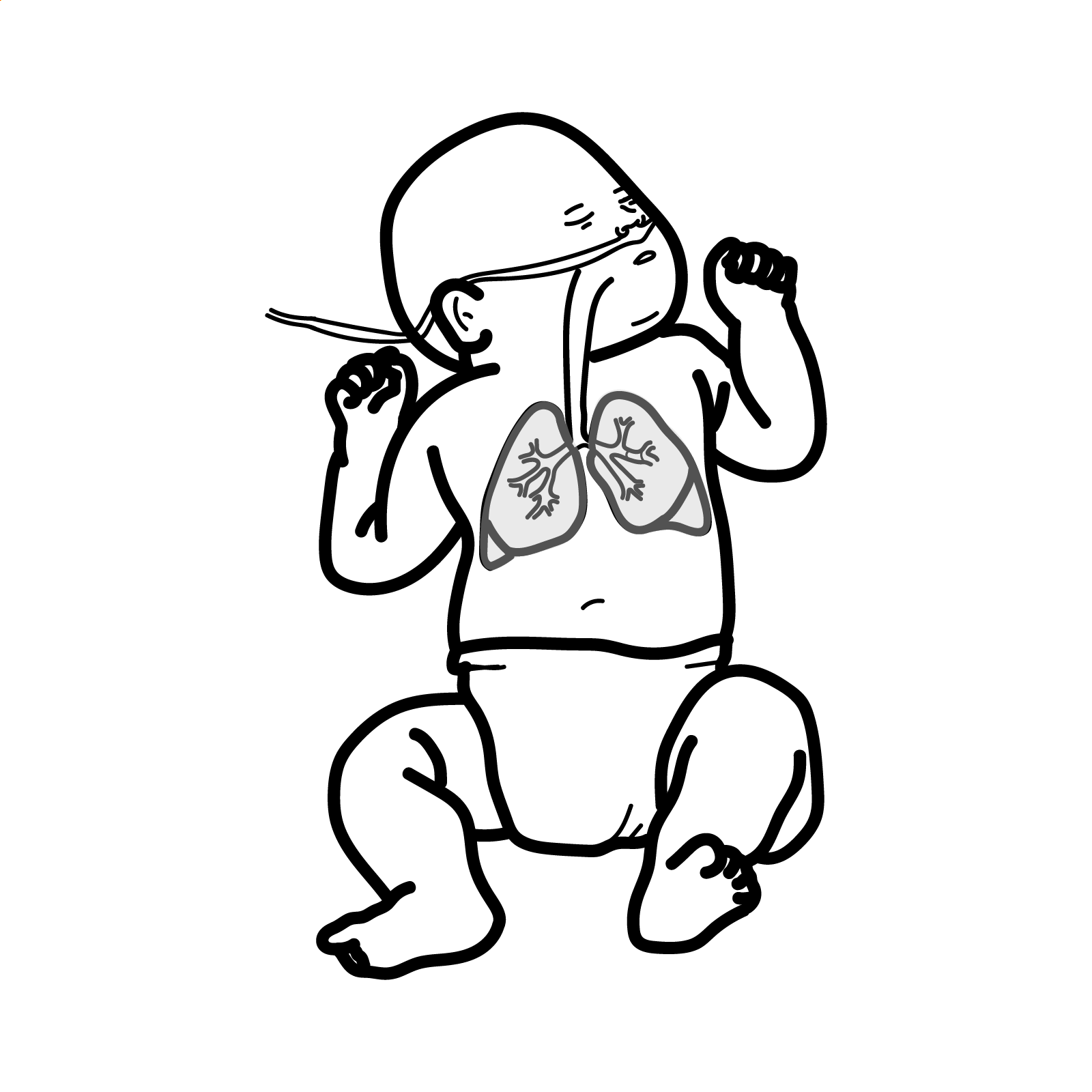
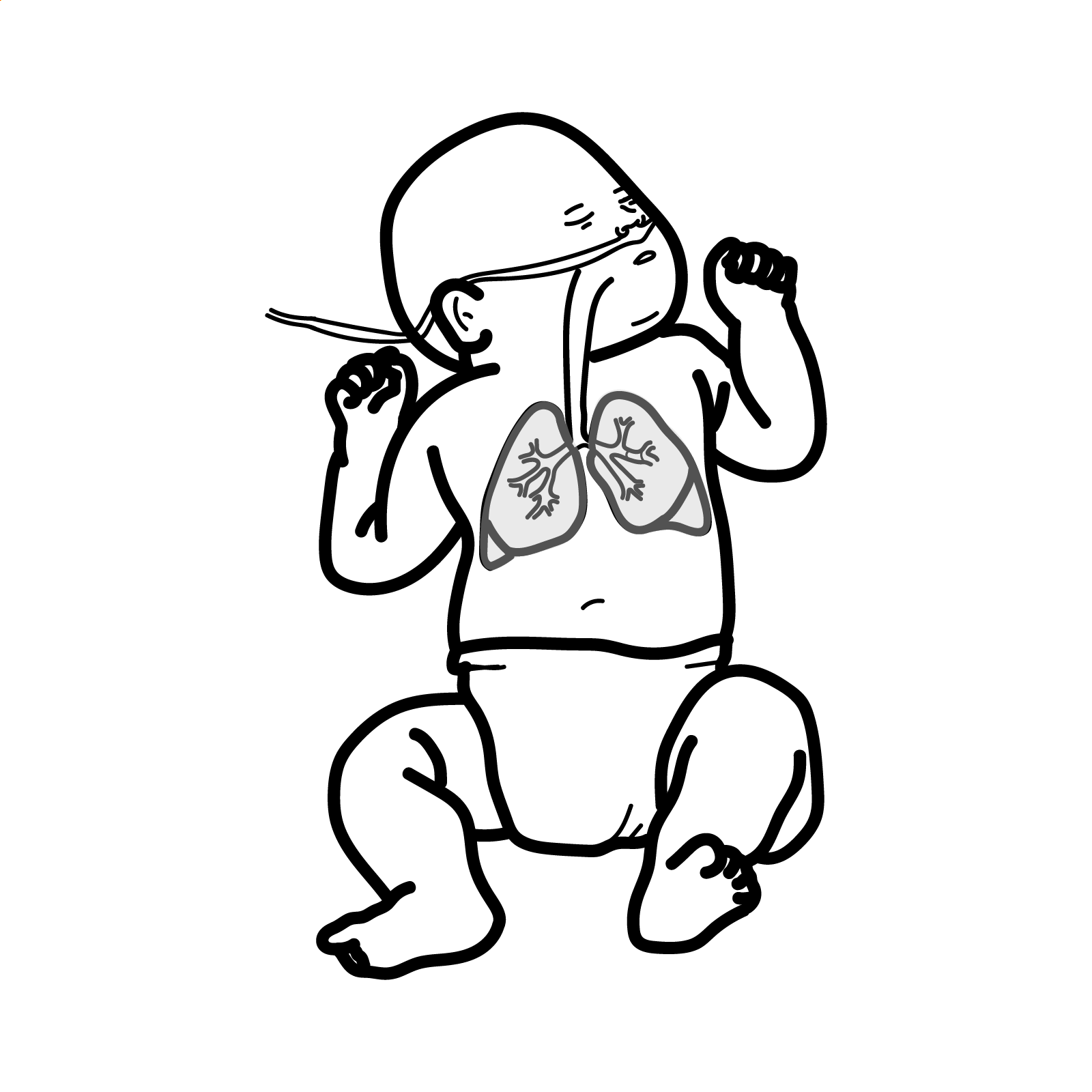
Respiratory distress syndrome (RDS) also known as hyaline membrane disease is a pulmonary disease resulting from immature lung development and surfactant deficiency. Most frequently seen in preterm infants, the clinical presentation is characterized by signs of respiratory distress including nasal flaring, tachypnea, and grunting (an expiratory sound that is heard as the infant exhales against a partially closed glottis). Symptoms often present shortly after birth and can increase in severity over the first 48 to 72 hours of life. The radiologic findings of RDS consist of a homogenous ground glass appearance of the lung fields with visible air bronchograms.
>90% risk of RDS if fetus is born 28 weeks or less.
Hyperpnea: refers to deep, relatively unlabored respirations at mildly increased rates. It is typical of situations in which there is reduced pulmonary blood flow (e.g., pulmonary atresia), and it results from the ventilation of underperfused alveoli.
Tachypnea: refers to shallow, rapid, and somewhat labored respirations, and it is seen in the setting of low lung compliance (e.g., primary lung disease, pulmonary edema).
Transition from foetal life to neonatal life requires:
Infants born by caesarean section are more likely to have retained lung fluid.
Pulmonary Surfactant
Surfactant is a surface-active lipoprotein complex comprised of a mixture of phospholipids (90%), proteins (10%), and a small portion of other neutral lipids. The main function of surfactant is to decrease surface tension of the alveoli allowing for maintenance of functional residual capacity preventing atelectasis and lung injury. The surfactant proteins also contribute to natural immunologic defenses and assist with the spreading of surfactant throughout the alveoli and the recycling of surfactant between cells and the airspaces.
Usually occur at or soon after birth (first 4-6 hours)
Persistent pulmonary hypertension of the newborn is a clinical syndrome of severe hypoxemia resulting from failure of the foetal circulatory pattern to transition normally to the newborn circulatory pattern.
A chest x-ray is the investigation to perform in infants with respiratory distress. Findings for RDS are white lungs with the presence of air bronchograms and a ground glass appearence. Air bronchograms are so called because the small air-filled bronchi are seen outlined against the opacified fluid-filled alveoli. Ground glass is because of alveoli collapse.
Diagnosis is made on the basis of the combination of clinical and radiological features.
More info on Neonatal resuscitation
Surfactant administration should be considered in any premature intubated infant with a presumed diagnosis of RDS.
| Indications for intubations |
| Hypoxia |
| Severe recurrent apnoea |
| Respiratory failure |
Prevention
If baby suddenly deteriorates despite initially improving think of the possible causes of sudden deterioration.
Overview
ARDS is an acute, diffuse, inflammatory lung injury that leads to increased pulmonary vascular permeability, increased lung weight, and a loss of aerated tissue. Clinical hallmarks of ARDS are hypoxemia and bilateral radiographic opacities, while the pathological hallmark is diffuse alveolar damage.
Clinical Presentation
Clinical hallmarks of ARDS are hypoxemia and bilateral radiographic opacities, while the pathological hallmark is diffuse alveolar damage.
Clinical Course
Diagnostic Criteria – Berlin Definition
Complications of ARDS
| DIFFERENCES BETWEEN NEONATAL AND ADULT RESPIRATORY DISTRESS SYNDROME | ||
| Neonatal Respiratory Distress | Adult Respiratory Distress | |
| Groups Affected | Premature infants, Caesarean section, Infant of diabetic mother | Adults sustained direct or indirect lung damage |
| Pathogenesis | Inadequate surfactant | Direct damage to lung (trauma, aspiration, irritant) or indirect damage from shock |
| Acute Management | Mechanical ventilation (positive end-expiratory pressure), Oxygenation, treat underlying disorder/precipitant, fluid management | Resuscitation then CPAP |
UpToDate
Best Practice
Victoria Health – Australia

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion