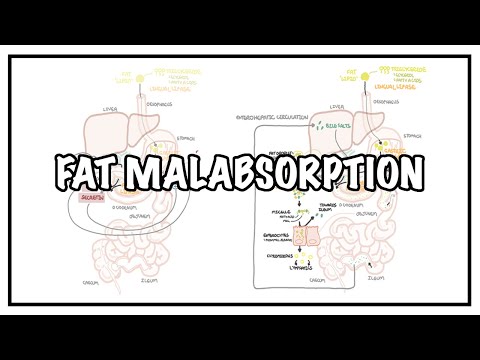
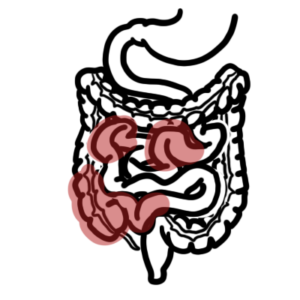
0:00 Hello, in this video, we're going to talk about celiac disease. 0:06 This is an overview and introduction. 0:10 Celiac disease is an inflammatory disease, a process which occurs in 0:13 susceptible individuals 0:15 in response to ingestion of wheat protein, gluten, specifically the protein lad 0:21 en. 0:22 The clinical presentation of celiac disease include abdominal pain, abdominal 0:28 discomfort, 0:30 bloating, diarrhea, stinky stool, stiatoria, which is essentially a fatty stool 0:38 , anemia, 0:40 weight loss, failure to thrive specifically in children, the young. 0:47 But celiac disease can also present asymptomatically in one third of people who 0:54 have it. 0:55 It's important to remember that if someone presents with diarrhea, weight loss, 1:00 or anemia, 1:01 anemia can be iron deficiency, or vitamin B12, to think of celiac disease. 1:08 Some signs of celiac disease around the face include development of apthus ul 1:14 cers, atrophic 1:15 glyceritis from the anemia, as well as anorexia from the malabsorption. 1:24 Dermatitis apatiformis is also another sign, and this is also known as Dureng's 1:30 disease, 1:31 and it's a chronic blistering skin condition that is itchy, and usually are on 1:38 extensive 1:39 surfaces such as your elbow, ankles, below the knees. 1:43 There are many differential diagnoses of celiac disease, but we will not go 1:48 into that. 1:49 If one presents with these clinical signs and symptoms, it's important to order 1:54 investigations. 1:56 Investigations include a full blood count, which will detect anemia or any 2:00 possible infections. 2:02 Electrolyte urea creatinine is important to check for an electrolyte derang 2:07 ement, as well 2:08 as malabsorption. 2:09 LFT is also important to see to rule out differential diagnoses that can affect 2:15 the liver or the 2:16 biliary tree. 2:17 Blood smear is also important to check for what type of anemia. 2:23 Serology tests can also be ordered to test for the presence of autoantibodies, 2:30 seen in 2:31 celiac disease. 2:33 Specifically, autoantibodies to transglutaminase, endomycin, as well as gliadin 2:41 . 2:42 Finally, an endoscopy can be performed, and it is gold-standard for the 2:47 diagnoses of 2:49 celiac disease. 2:51 And this is essentially where a camera is fed through the esophagus down to the 2:55 swollen 2:56 intestine where a tissue biopsy can be taken, and using this tissue biopsy a 3:01 diagnosis can 3:02 be made. 3:03 However, for a proper diagnosis, the person suspected of having celiac disease 3:08 should 3:08 not eat gluten-containing foods initially. 3:12 Then a biopsy will be taken. 3:14 This is followed by eating normal gluten-containing food, and then another 3:19 tissue biopsy taken. 3:20 And this is in order to check for the differences in small intestine tissue 3:27 architecture. 3:29 And the changes seen in active celiac disease include increase in lymphocytes 3:35 in the area, 3:36 hypertrophy of the crypts, as well as villus atrophy. 3:41 And this is the hallmark for the diagnoses of celiac disease. 3:48 Glutin is ongoing and includes mainly a gluten-free diet. 3:51 A gluten-free diet means not eating foods containing gluten. 3:57 Glutin-containing foods can be remembered with the acronym BROW. 4:03 So B as in Bali, R as in rye, O as in oats, and W as in wheat. 4:10 So these four things contain a lot of gluten and therefore should be avoided. 4:15 Further, if malabsorption is an issue, supplements such as calcium, iron, as 4:20 well as other vitamin 4:21 supplements can be offered. 4:24 During periods of exacerbations from celiac disease, aka cilia crisis, quick 4:31 treatment 4:32 is important. 4:34 Celiac crisis is a life-threatening condition, and it is rare. 4:40 People who present usually have unexplained diarrhea with severe malabsorption 4:47 and massive 4:48 electrolyte imbalance. 4:50 Treatment of celiac crisis include rehydration with electrolytes and also cort 4:55 icosteroids 4:56 to reduce the inflammation and pain that is occurring. 5:02 Now let us talk about the pathophysiology, the mechanism of disease of celiac 5:08 disease. 5:09 So here is the jejunum, the duodenum, and the stomach. 5:13 We are looking at the lumen of the jejunum and the cells here. 5:17 So here is a zoomed-in view of the area. 5:21 Here is the lumen where food will pass through, or parts of the food. 5:26 The jejunum is made up of enterocytes and below these enterocytes is the lamin 5:32 opropia, 5:33 which contains other types of cells. 5:35 On top of the enterocytes, here in yellow is the mucus. 5:40 The small intestine forms crypt and villi. 5:43 The enterocytes of the small intestine also have microvilli, which are 5:48 essentially small 5:49 finger-like projections that increase the surface area to increase absorption. 5:57 As mentioned, here in yellow is the mucus, which actually lines and protects 6:01 the mucosal 6:02 cells, the enterocytes. 6:04 And reciting on top of the mucus, we can find antibodies, IgA-dimeric 6:10 antibodies. 6:12 And IgA antibodies are the antibodies of the mucosal immune system and help 6:17 defend against 6:18 infections. 6:21 Within the laminopropia, which is the level below the enterocytes, you can find 6:26 some 6:26 other cells, including antigen-presenting cells, which are important cells in 6:31 the communication 6:32 between the innate immune system and the adaptive immune system. 6:37 Some people essentially have a predisposition to developing celiac disease. 6:42 And these are risk factors, and these risk factors include having a family 6:47 history of 6:47 celiac disease, an autoimmune thyroid disease, having type 1 diabetes, having 6:55 IgA deficiency, 6:57 and inflammatory bowel disease. 7:02 The pathophys of celiac disease is a mystery, but here, and now, I'm just going 7:06 to draw 7:07 about the current, I guess, theory. 7:10 So drawing it out, I'm just drawing the same picture on the left. 7:13 Here we have the lumen of the small intestine, the enterocytes. 7:18 And above the enterocytes is the mucus in yellow. 7:21 Below the enterocytes is the laminopropia, where we can find some cells, 7:26 including the 7:26 antigen-presenting cells. 7:30 In some parts of the small intestine, there are also things called payous 7:34 patches, and 7:35 also nearby, there are mesenteric lymph nodes, which are really important lymph 7:40 oid tissues 7:41 which help activate an immune response. 7:45 In these tissues, we can find what's called naive T cells, which are basically 7:50 T cells, 7:51 an immune cell, which is not activated. 7:55 Now above the mucosa, back here again, as mentioned earlier, there are 7:59 antibodies. 7:59 IgA antibodies. 8:01 IgA is the antibody of the mucosal immune system, and it is dimeric here. 8:09 So the pathogenesis theory goes something like this. 8:13 Gluten-containing food is broken down, and a part of gluten, a specific heart 8:17 called 8:18 gliden, is absorbed. 8:21 Gliden, through the enzyme tissue glutaminase, or TTG, gets converted to de-am 8:30 inated gliden 8:31 peptides. 8:33 The de-aminated gliden peptides gets picked up by these antigen-presenting 8:38 cells within 8:39 the area. 8:40 The antigen-presenting cell will then present this peptide onto a specific 8:44 class of molecule 8:45 called the HLADQ2, or HLADQ8. 8:53 And so this antigen-presenting cell will bring this de-aminated gliden to 8:59 nearby lymphoid 9:00 tissues, such as the payer's patches or the mesenteric lymph nodes. 9:04 And here, the antigen-presenting cell will present this gliden peptide to the 9:11 naive T 9:12 cells. 9:13 This contact will actually activate the naive T cells to become either CD8 T- 9:20 killer cells 9:21 or CD4 T-helper cells, depending on the cytokines, chemical produced, and all 9:26 these other stuff. 9:28 But just remember that the naive T cells become either a T-killer or a T-helper 9:34 cell. 9:35 And these cells are now primed against the de-aminated gliden peptide, or the 9:43 gliden protein to 9:44 make it easy. 9:47 The CD8 T-killer cell, as the name suggests, kills things. 9:51 They are agro and will promote inflammation when in contact with gliden. 9:56 So every time we eat gluten, which contains gliden, inflammation will occur. 10:03 The CD4 T cells, as the name suggests, they actually help another cell called B 10:10 cells. 10:11 What they do is they help activate B cells. 10:13 And the activation of B cells means that these B cells can mature and become 10:18 plasma cells. 10:20 And plasma cells are the cells that produce our antibodies. 10:24 So in this scenario, this plasma cell will produce antibodies against gliden 10:31 because 10:31 it was the protein that was presented in this whole scenario. 10:37 Interestingly, the plasma cells activated in patients with celiac disease can 10:42 actually 10:42 produce other antibodies. 10:45 So we mentioned anti-gliden, but there are also anti-endomycin, or endomycium, 10:53 or endomycio, 10:54 as well as anti-tissue transglutaminase. 11:00 Regardless, when these antibodies are in contact with gliden, endomycium, or 11:07 functional tissue 11:08 transglutaminase, they will promote inflammation. 11:12 And so every time we eat foods containing gliden, inflammation will occur 11:16 around the 11:16 area. 11:19 Inflammation around the small intestine will cause abdominal pain, abdominal 11:23 discomfort, 11:25 diarrhea, as well as bloating. 11:27 Not only that, but inflammation damages the lining of the small intestine, 11:31 making the 11:32 crypts look all funny, and also damaging the microvilli, the small finger-like 11:37 projections 11:38 in the area. 11:39 So what does this mean? 11:41 Well, it means that things can't be absorbed properly. 11:45 So when there's damage to the mucosa, this area, things such as iron and 11:50 vitamin B12 11:52 cannot be absorbed properly. 11:55 Infants such as protein carbohydrates cannot be absorbed properly. 12:00 Iron and vitamin B12 that can't be absorbed leads to anemia. 12:06 Other nutrients not being absorbed efficiently leads to weight loss, as well as 12:10 failure to 12:11 thrive in children. 12:14 Lipids, fats that are not being absorbed, means that the lipids will still stay 12:19 in the 12:19 bowels and will come out in poo, and this will cause the stool to be stinky, 12:24 and you 12:24 get steatoria, which is basically fatty stool. 12:29 And these things again are not absorbed properly because of the damaged mucosa 12:36 lining, thanks 12:36 to the inflammation. 12:39 Let's now take a closer look and focus on the pathological changes seen in the 12:44 small 12:44 intestine of people who have celiac disease. 12:48 And there are four changes that is important here. 12:52 The first is that we can see villus atrophy. 12:55 We can see hyperplasia of intestinal crypts. 12:59 We can see increase in lymphocytes in the laminopropia and around this area. 13:04 And finally, we see cell death around the area, or just destruction in general. 13:11 Complications of celiac disease can be minor or life-threatening. 13:16 Complications include anemia, they have increased, I guess, risk of developing 13:22 certain tumors, 13:23 a GIT T cell lymphomas. 13:27 They can get hypo-splinism, osteoporosis, neuropathies, and dermatitis herpat 13:37 iformis. 13:39 All diagnoses of celiac disease include cow milk sensitivity, food sensitive 13:47 entropathies, 13:50 Crohn's disease, colitis, GIT lymphoma, Whipple's disease, Giardia-Lambia 14:03 infection, and irritable 14:06 bowel syndrome.