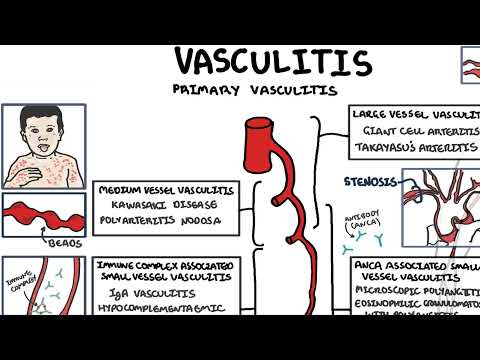
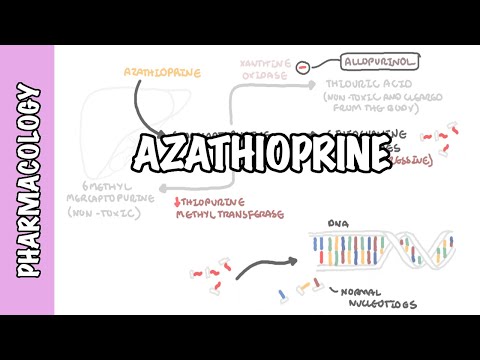
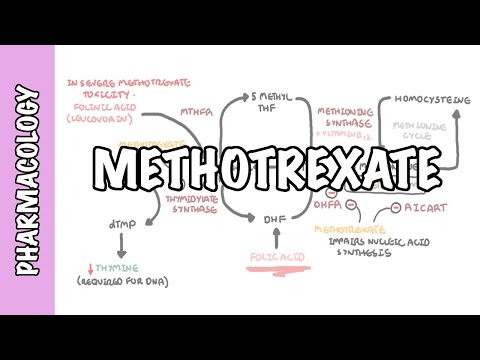
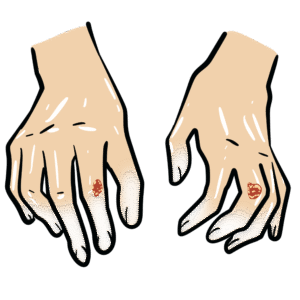
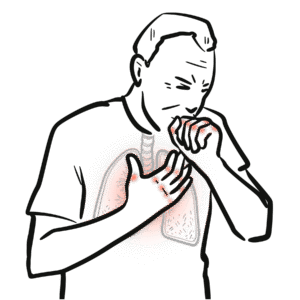
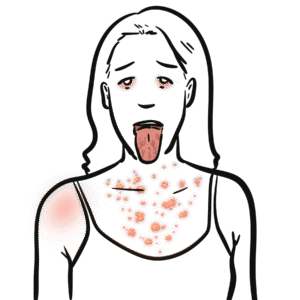
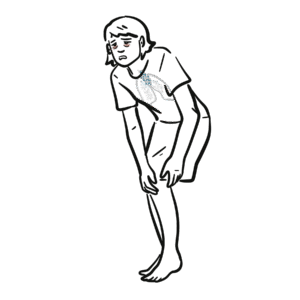
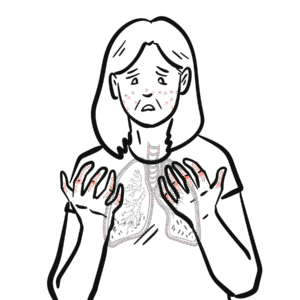
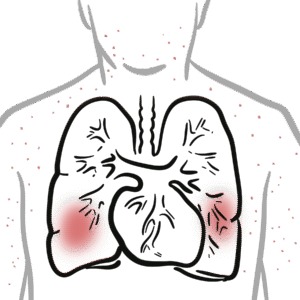
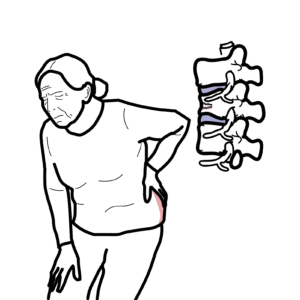
0:00 Hello, in this video, we're going to talk about dermatomyositis. 0:08 If you haven't watched the overview video on inflammatory myopathies, please 0:12 watch that 0:12 first. 0:13 Dermatomyositis is an autoimmune disease where you have inflammation of the 0:18 skin causing 0:19 unique skin rashes and inflammation of the muscle, which leads to muscle 0:27 weakness. 0:28 Dermatomyositis is an autoimmune disease, where the body produces specific 0:33 types of antibodies, 0:36 and the immune system attacks the muscle. 0:39 To understand this autoimmune disease, we need to recap the anatomy of skeletal 0:43 muscle 0:43 tissue. 0:45 This muscle tissue is made up of fascicles, which are made up of muscle units 0:50 called 0:50 muscle fibers. 0:52 Each muscle fiber, in turn, are composed of myofibrils, which contain the 0:57 functional 0:57 unit of muscles, called sarcomeres. 1:01 Sarcomeres are what allow muscles to contract, thus allowing you to lift your 1:07 arms above 1:07 your head and climb upstairs. 1:10 Let's focus on the pathophysiology now of dermatomyositis. 1:16 The sequence of events that actually cause the immune system to cause 1:21 inflammation of 1:21 the muscle is not completely understood. 1:25 However, there is likely an inappropriate activation of complement proteins, 1:32 targeting 1:33 the periomycium, the layer surrounding a muscle fascicle. 1:39 Let's take a closer look at a fascicle, which is surrounded by the periomycium. 1:45 Here, you can also find blood vessels. 1:49 The fascicle is made up of muscle fibers, and myofibrils, as we have learned. 1:55 The thought is that there are antibodies, which accidentally mistake part of 1:59 the muscle 2:00 as foreign, possibly following an infection. 2:04 Or, there are dermatomyositis-specific antibodies that people have that target 2:11 the muscle. 2:12 The antibodies target the periomycium, including the blood vessels there. 2:19 Once bound, the antibodies activate the complement system, which consists of 2:24 specialized protein 2:26 that promotes the inflammatory response towards that target. 2:31 Regardless of what antibodies initiates this whole process, what is seen as a 2:36 result of 2:36 complement activation is blood vessel inflammation and destruction around the 2:41 fascicle that leads 2:42 to schemia and infarction to the muscle tissue, which then in turn leads to 2:50 muscle inflammation 2:52 and muscle atrophy. 2:56 The specific term for these changes seen in the muscles of people with dermat 3:01 omyositis 3:02 is peri-fascicular inflammation with peri-fascicular atrophy. 3:12 When muscle become inflamed and damaged, they start releasing enzymes, and most 3:17 importantly, 3:17 creatinine kinase, as well as AST and ALT, usually known as liver enzymes, but 3:23 are also 3:24 found in muscle as well. 3:30 And so with all this inflammation of the muscle as well as of the skin, dermat 3:35 omyositis manifests 3:37 with both muscular symptoms and skin signs. 3:42 People present with gradual proximal symmetrical muscle weakness in the 3:47 shoulders and in the 3:48 hips. 3:49 People often complain of weakness climbing upstairs or standing from a seated 3:53 position. 3:54 Dysphagia, dysphonia, and symptoms of aspiration indicate possible involvement 4:01 of striated 4:02 muscle of the pharynx and esophagus, and are associated typically with poor 4:11 prognosis. 4:13 And so what are these cutaneous findings or skin changes? 4:16 Well, the skin changes associated with dermatomyositis include pathonomonic 4:21 findings such as heliotropresh, 4:23 which is periorbital erythema with edema, most often of the upper eyelids, gutt 4:28 rends 4:29 papules, pink, elatious papules, overlying interflangeal and metacapophalangeal 4:34 joints 4:35 in the hands, guttrend signs, which are red macules or patches over extensive 4:40 surfaces 4:41 of elbows, knuckles, knees, and ankles. 4:44 Then you have other characteristic rashes, which include sholesign and v-sign, 4:48 which 4:48 are photosensitive, holster sign, cross the thigh, and you also see nail fold 4:55 changes, 4:56 which includes subungal erythema and dilated capillary loops. 5:03 Amiopathic dermatomyositis is a condition where patients have characteristic 5:07 dermatomyositis 5:08 rash without muscle involvement. 5:12 Again, amiopathic dermatomyositis means they have classic dermatomyositis rash, 5:18 but without 5:19 muscle weakness. 5:22 Now there are other clinical manifestations or signs and symptoms of dermatomy 5:27 ositis but 5:27 are only seen in those with certain dermatomyositis specific antibodies. 5:33 These antibodies can be measured in the blood and also help with the diagnosis. 5:38 So what are the dermatomyositis specific antibodies that potentially play a key 5:42 role in the pathophysiology? 5:46 Well, dermatomyositis specific antibodies include anti-MI2, anti-small ubiquit 5:52 in-like 5:52 modifier activating enzyme, SAE, anti-TIF1 gamma, anti-NXP2, and anti-melanoma 6:01 differentiation 6:02 associated protein 5 or MDA5. 6:06 There are some important things to know about these different antibodies. 6:10 First of all, anti-MI2 is the most frequent seen in adults. 6:14 Anti-TIF and NXP are associated with malignancy. 6:20 TIF specifically is strongly associated with malignancy. 6:24 MDA5 is associated with interstitial lung disease. 6:30 Differential diagnosis to be aware about our other inflammatory myopathies such 6:35 as anti-synthetase 6:36 syndrome which is a condition that can present with similar skin changes but 6:40 also associated 6:41 with interstitial lung disease and mechanics hands. 6:48 There's something called overlap myositis which also presents with dermatomy 6:52 ositis skin 6:52 changes but is really associated with other rheumatological causes such as s 6:58 cleroderma 6:59 and lupus. 7:00 There is an image of scleroderma hands called sclerodactyly. 7:09 Inflammatory myopathy differentials that have no skin involvement include poly 7:13 myositis, 7:14 immune-mediated necrotizing myopathy, and inclusion body myositis. 7:19 And here is a hand of a person with inclusion body myositis. 7:23 Note muscle wasting of the hands. 7:27 Other differential diagnosis include viral myopathy and thyroid-related myopath 7:32 ies amongst 7:32 my senior gravis for example as well. 7:38 Earlier in the pathophysiology section we looked at some investigations that we 7:42 could 7:42 have already ordered in inflammatory myopathies such as creatinine kinase, AST 7:48 and ALT which 7:49 would both be elevated. 7:51 The inflammatory markers, CRP and ESR can be both elevated and also importantly 7:57 ordering 7:58 myositis panel to look for myositis specific antibodies. 8:03 An MRI of the muscle is important and most specifically a muscle biopsy which 8:07 is the 8:07 gold standard for diagnosing and differentiating the different types. 8:12 Muscle biopsy as we have learned will show peri-fecicular inflammation and atro 8:18 phy. 8:19 Muscle investigation is a skin biopsy which can confirm features of dermatomy 8:25 ositis. 8:25 Treatment of dermatomyositis is with glucocorticoids and disease modifying anti 8:30 -romatic drugs can 8:31 also be used such as methetrexate or azathioprine, intravenous immunoglobulins 8:37 and other immunosuppressants 8:39 as retuximab and cyclophosphamide are also used. 8:43 There is a risk of flares which can again be treated with escalated doses of 8:49 glucocorticoids. 8:51 In summary, dermatomyositis is an autoimmune inflammatory myopathy 8:55 characterized by presence 8:56 of dermatomyositis specific antibodies and muscle biopsy showing peri-fecicular 9:02 inflammation. 9:04 Treatment is with immunosuppressants.