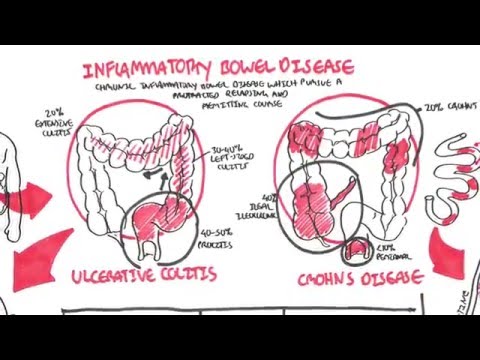
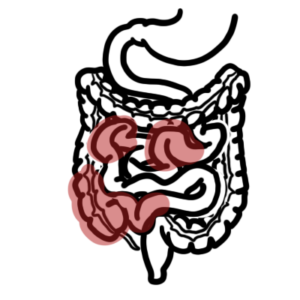
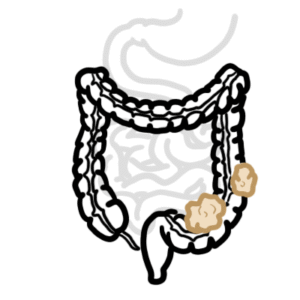
0:00 So in this video, we're continuing on with inflammatory bowel disease, looking 0:08 at the 0:08 local complications as well as the systemic complications of IBD, as well as 0:15 looking actually 0:16 a lot more at the pathophysiology. 0:18 So let's begin with the local complications. 0:22 So here I am drawing the rectal sigmoid area, which is the most common site 0:27 affected by 0:29 ulcerative colitis. 0:31 Complications include colon cancer, rupturing of the bowel, perforation, and 0:38 massive hemorrhage. 0:43 In Crohn's disease, the part of the colon, or GIT, mostly affected is the ili 0:48 osecal area. 0:51 And local complications can include your colon cancer, stenosis, strictures, 0:57 absisformation, 1:00 fistula, lymphadenopathy, as well as perforation, which I have not drawn. 1:07 Now the pathophysiology of both Crohn's and ulcerative colitis, basically 1:12 inflammatory 1:13 bowel disease, is not fully understood, but we do know some things such as we 1:19 know this 1:20 cells involved and as well as the cytokines. 1:24 So let us take a closer look. 1:27 Now both Crohn's and ulcerative colitis share similar pathophysiology. 1:32 So we will just look at an overview, the overview picture, the overall picture. 1:39 So here are your intestinal epithelial cells, your IEC. 1:44 And this can be your M cell, which is part of the payest patches, for example. 1:51 Here is the mucosa layer in blue. 1:55 I mean, this is your mucosa, sorry, which is the fluid. 1:59 And they have bacteria on the surface here, commensal bacteria. 2:04 We have a lot. 2:07 And these are your penith cells that secrete antimicrobial peptides to keep the 2:11 microbes 2:11 in the intestine in check. 2:14 We also have goblet cells, which are the ones that produce and secrete the muc 2:20 us. 2:20 Okay, so you can have genetic and environmental factors that predispose you to 2:25 inflammatory 2:27 bowel disease. 2:28 The genetic factors include problems with the following. 2:31 Antimicrobial peptides, problems, otophagy, handling of bacteria, cytokines. 2:39 All include problems with the microenvironment, diet, infections, stress, non- 2:46 steroidal anti-inflammatory 2:47 drug use, smoking as well as antibiotic use. 2:54 So those are the genetic and environmental factors. 2:58 These genetic and environmental factors can lead to the following scenarios. 3:03 M cells, right, they normally sample antigens in the lumen. 3:08 So you can get translocation of the microbial peptide, the microbial product. 3:12 The translocation of the microbial peptide activates the immune cells. 3:18 So here you have the macrophage, the antigen-presenting cell, activated. 3:24 Alternatively, and this occurs in the large intestine mainly, you can get 3:29 impaired barrier 3:30 function due to genetic or the environmental factor, or whatever, the reason. 3:36 This can also lead to the translocation of microbial products. 3:42 And of course, this internal will activate the immune cells as well. 3:46 So the antigen-presenting cell, the macrophage, will process these bacteria, 3:52 these antigens, 3:53 and it will present it to the T cells, the CD4 T cells. 3:59 The antigen-presenting cell will activate the CD4 T cell. 4:04 This results in a few things. 4:07 One, the CD4 T cell further stimulates and activates the macrophages in the 4:14 area. 4:15 And two, both the CD4 and the macrophages will start releasing heaps of cytok 4:22 ines, including 4:23 TNF-alpha, interleukin-1, and interleukin-6. 4:28 Now these cytokines are continuously released, resulting in chronic 4:35 inflammation. 4:37 And essentially, it's the cytokine production and the chronic inflammation, 4:42 which will lead 4:42 to the local and systemic complications associated with inflammatory bowel 4:48 disease. 4:49 So that was a general overview. 4:51 Let us now focus on tumor necrosis factor alpha, TNF-alpha, which plays a big 4:56 role in 4:57 the pathogenesis of IBD. 5:00 So TNF-alpha is one of the inflammatory cytokines. 5:05 And when released, it does many things in the body. 5:08 For example, it stimulates angiogenesis, formation of new blood vessels. 5:13 It induces pathosil necrosis, so say goodbye to the antimicrobials. 5:19 TNF-alpha stimulates IEC death and also impairs barrier function. 5:27 TNF-alpha increases the immune response, causing further damage. 5:33 And also, TNF-alpha stimulates myofibrils to release proteases, which causes my 5:38 ofibril 5:39 induced destruction within the area. 5:45 So as a result of the activity of these cytokines, you get the local and 5:49 systemic complications 5:51 of inflammatory bowel disease. 5:54 We talked about earlier about the local complications of inflammatory bowel 5:58 disease. 5:59 Now let us look at the systemic complications. 6:03 So systemic complications of IBD during the active phase, so when inflammation 6:11 is occurring. 6:13 And this includes conjunctivitis, iritis, mouth ulcers, fatty liver, liver abs 6:21 cess, mesenteric 6:23 or portal vein thrombosis, venous thrombosis, large joint arthritis, erythema, 6:32 nodosum, 6:34 and pyoderma gangrenosum. 6:36 So essentially, these systemic effects are a result of the release of mainly 6:44 cytokines, 6:45 such as TNF-alpha. 6:47 So that was the looking at the pathophysiology, and we also looked at the local 6:52 and systemic 6:53 complications as a result of the cytokines and the pathogenesis. 6:59 Let's now look at the investigations we can perform for patients who present 7:06 with possible 7:07 inflammatory bowel disease. 7:09 So investigations include your full blood count. 7:12 This is to check for anemia, as well as malabsorption, the vitamin B12 and iron 7:16 , for example, because 7:18 your intestine, your intestine and mucosa are damaged. 7:22 Two, blood chemistry, you patients often present with a decrease in albumin due 7:27 to inflammation 7:28 and the interopathy. 7:31 Three, your ECR and your C-reactive protein, levels would be up, and this would 7:39 indicate 7:40 inflammation. 7:43 Four, MCS, the microscopy culture sensitivity. 7:51 And you can do this using stool, so you get a stool sample, and essentially it 7:57 's to rule 7:58 out bacterial and parasitic involvement, such as C-diffecile, because often the 8:03 patient 8:04 presenting, it's similar, a C-diffecile infection, as well as a inflammatory 8:10 bowel disease presentation. 8:12 It can be someone. 8:15 Five, of course, the investigation, the gold, basically gold standard, you 8:19 would want to 8:20 perform an endoscopy, the colonoscopy, which essentially, when you go up 8:25 through the rectum 8:26 up into the colon to check the structure, the architecture of the colon. 8:32 And so now let's focus more on the endoscopy, the colonoscopy, looking at both 8:36 ulcerative 8:37 colitis and Crohn's disease, and what we would see. 8:40 So let's begin with ulcerative colitis. 8:43 Colonoscopy will show error-thematous appearance, continuous lesion, 8:48 superficial inflammatory 8:49 inflammation. 8:50 You can also see pseudopolyps, you can also see PKA, exudate, edema, also may 8:57 be present. 8:58 Now in Crohn's, well, when performing a colonoscopy, you can see cobblestone 9:03 appearance, skip lesions. 9:04 You can also see pseudopolyps, as well as granulomas. 9:09 Six, you can also do a biopsy as your investigation. 9:14 And this is, you can do it for both, but for ulcerative colitis, the findings, 9:18 you can 9:19 see things such as crypt abscess, crypt atrophy, mucin depletion, and 9:26 inflammatory signs. 9:29 Seven, radiology. 9:33 And this is for Crohn's disease, and it's essential for staging Crohn's disease 9:38 , and 9:39 also for the radiological investigations, a traditional barium is used. 9:45 Now let's talk about, so that was some investigations that can be performed for 9:50 inflammatory bowel 9:51 disease. 9:52 Let's now look at the diagnosis for ulcerative colitis and Crohn's disease. 9:57 So for ulcerative colitis, it's essentially presence of chronic diarrhea more 10:01 than four 10:01 weeks, and evidence of acute inflammation on endoscopy, and chronic changes on 10:08 biopsy. 10:10 So that is why biopsy is mainly performed for ulcerative colitis. 10:14 For Crohn's disease, you have endoscopic findings of Crohn's disease and 10:18 imaging studies with 10:20 compatible clinical history of Crohn's. 10:25 Treatment. 10:26 Mainly, you, two things, one, to treat acute attack, and two, to prevent 10:32 relapse. 10:33 So let's focus on ulcerative colitis first. 10:36 So active proctitis, extensive colitis, you use five as a therapy, oral, plus 10:43 minus corticosterous 10:44 steroids. 10:45 So what is five asa? 10:47 Well, it's an acid similar to aspirin type thing, but it's five asa is usually 10:52 inactive 10:52 when you give it, and when it enters the colon, it becomes activated by the 10:57 bacteria there, 10:59 and essentially when it's active, it will result in a, it will cause, reduce, a 11:04 reduction 11:05 in local inflammation. 11:06 That's just a general picture overview. 11:09 For severe ulcerative colitis, you need evaluation, lab tests. 11:14 You have to perform, you have to give fluids for dehydration, intravenous cort 11:18 icosteroids 11:19 to reduce immune flare. 11:21 You don't give them five asa for severe ulcerative colitis. 11:26 But of course, if all this is unresponsive, you give them intravenous 11:30 antibiotics or 11:30 TNF alpha antagonist. 11:34 And for maintenance of remission when the inflammatory bowel disease is not 11:40 active, they 11:41 are there on five asa therapy. 11:45 Surgees is also performed and it's very common. 11:48 Surgees for remove, to remove the parts of the colon, and actually about one 11:52 third diagnosed 11:53 with ulcerative colitis undergo surgery in the first five years. 11:58 And surgery can involve removing parts of the colon, for example. 12:04 Now let's look at Crohn's disease. 12:06 The principle treatment for Crohn's is continuous monitoring for the 12:11 complications because there's 12:13 a lot of complications associated with Crohn's, including your strictures and 12:18 fistulas, as 12:18 well as just stenosis. 12:23 Treatment also includes preventing the relapse. 12:25 This involves corticosteroids for immune suppression, diet, chronic patients. 12:32 You give TNF alpha antagonists, which are your, essentially, your antibodies. 12:39 For maintenance therapy, patients are given theopurine or methotrexate. 12:44 And this is to reduce the immune response. 12:47 And yeah, also TNF alpha antagonists are also given. 12:53 Surgery is also performed. 12:55 So surgery, it deals with the complications associated with Crohn's disease. 13:00 And also, you remove parts of the colon that are severely damaged. 13:04 Because Crohn's disease is a transmural inflammation, it affects all layers. 13:08 So it really causes a lot of damage. 13:13 So I hope you enjoyed this video on Crohn's disease. 13:14 We looked at the local, the systemic complications due to the pathophysiology, 13:20 the cytokines. 13:21 And we also looked at the investigations, the diagnosis, and management for all 13:26 inflammatory 13:26 bowel disease. 13:27 Thank you for watching. 13:30 You