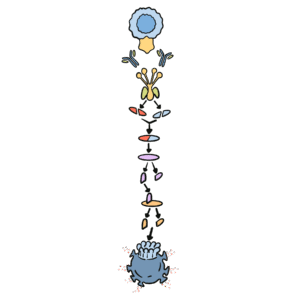
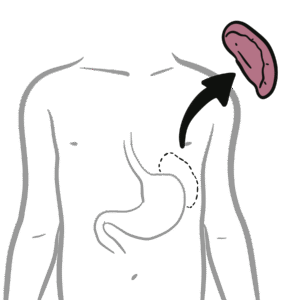
0:00 So here the activated CDA and the activated CD4 cells are in the mesenteric 0:04 lymph nodes 0:05 now, travelling from the pair's patches, as well as the activated B cell. 0:12 Now if the antigen presenting cell, the dendritic cell, didn't activate the 0:16 naive lymphocytes 0:17 within the pair's patches, it can then leave the pair's patches with the 0:21 antigen on the 0:22 major histocompatibility complex and also activate naive lymphocytes within the 0:28 mesenteric 0:29 lymph nodes. So dendritic cells can activate lymphocytes, naive lymphocytes 0:34 within the 0:34 pair's patches, or it can activate lymphocytes within the mesenteric lymph 0:37 nodes, basically. 0:39 So if the dendritic cell were to enter the lymph, mesenteric lymph nodes via 0:43 the afferent 0:44 lymphatic vessel, it will activate the naive CD8 and naive CD4T cells here and 0:50 convert 0:50 retinal to the retionic acid in the process. And remember what retionic acid 0:54 does? Well 0:55 the retionic acid production allows dendritic cells to induce expression of h 0:59 oming receptors 1:00 on these lymphocytes. And remember homing receptors basically tells where these 1:05 lymphocytes 1:06 have to go. Next. So what are these homing receptors called? Well the lymph 1:12 ocytes express 1:13 homing receptors integrin alpha 4b to 7 and also CCR9. However this can also, 1:20 the integrin 1:21 can also be different depending on which location it has to go. But this is 1:27 typically an integrin 1:28 alpha 4b to 7 and CCR9. And the homing receptors are expressed following lymph 1:34 ocyte activation 1:35 by dendritic cells or antigen presenting cells. The naive B cells can then be 1:40 activated by 1:41 the CD4, activated CD4 cell, which is a T helper cell. Once the B cell is 1:48 activated 1:48 by the T helper cell, the B cell will begin maturing and will begin class 1:55 switching, meaning 1:56 that it will class switch from IgM antibodies and begin expressing IgA 2:01 antibodies. And remember 2:02 IgA antibodies is important in the mucosal immune system. A particular T helper 2:09 cell, 2:09 the T helper two cells, secrete interleukin 5 and interleukin 6, which help 2:14 stimulate 2:14 the naive B cells to become IgA-producing plasma cells. However, the plasma 2:19 cells are 2:20 not actually activated within the lymph nodes. They become activated plasma 2:25 cells once they 2:26 leave the blood vessel or the lymphatic vessel into the tissues, the designated 2:32 tissues where 2:33 the homing receptors will take them. So now we have an activated CD8, CD4 cell 2:38 and a 2:39 yet to become plasma cell, leaving the mesenteric lymph nodes via the effort 2:44 lymphatic vessel. 2:46 And they're going to go to where the homing receptors will take them. So again, 2:55 the soon 2:56 to be plasma cell gets activated when the T helper two cells secrete interleuk 3:03 in 5 and 3:04 interleukin 6, which causes a plasma cell to express IgA or make it be able to 3:12 secrete 3:13 IgA antibodies. But this usually happens in the tissues. So what is an IgA 3:21 antibody, 3:21 where an IgA antibodies are very important in the mucosal immune system. When 3:25 they're 3:25 in the mucosal immune system, when they are secreted by plasma cells, they are 3:29 usually 3:29 dimeric, meaning that they're secreted to antibodies back side to back side. 3:36 However, 3:37 if IgA is secreted into the plasma, they're usually monomeric, meaning just one 3:42 antibody. 3:42 But because we're talking about the mucosal immune system, it's dimeric, such 3:48 as this. 3:48 And they're very important in preventing infection by either neutralizing an 3:53 antigen of a pathogen 3:54 or bringing an antigen of pathogen outside of our body into the lumen to be 3:59 secreted out 3:59 as feces or whatever. So these lymphocytes and plasma cells will travel through 4:06 the lymphatic 4:07 vessel and enter the heart. Where once it enters the heart, the heart will pump 4:11 these 4:12 immune cells out via the aorta. So now from the lymph vessel, it is in the 4:17 bloodstream. 4:18 The lymphocytes and the plasma cells will travel via the bloodstream. And 4:23 because it has the 4:24 holding receptors, these integrin and the CCR-9, is able to bind to other 4:31 receptors on the 4:33 blood vessel walls, which allows the lymphocytes to move into the associated 4:39 tissue. 4:40 So here we have receptors underneath the laminopropia or within the laminoprop 4:46 ia, 4:47 called madcam-1 and CCR-25. These receptors have affinity for the 4:55 holding receptors on the T cells, for example, the integrin and the CCR-9. So 5:01 here we have a 5:01 T helper cell, a CD4 cell, where the integrin binds to the madcam-1 and the CCR 5:09 -9 is attracted 5:10 to CCl-25. And this allows for the cell to migrate across the endothelial cell 5:18 into the laminopropia. 5:20 Similarly, we have a CD8 cell here, a T killer cell, where the integrin has 5:24 affinity for the 5:25 madcam-1 and the CCR-9 is attracted to CCl-25. B lymphoblasts also have this, 5:32 the immature plasma 5:33 cells. So this is not meant to be a CCR-7, it's meant to be a CCR-9. So 5:39 essentially the 5:39 integrin and the chemo-receptors CCR-9 allows the T cells to move from the 5:44 blood into the tissue. 5:45 Now it should be also noted that not all mucosal surfaces express the same chem 5:51 okines and receptors. 5:52 And so this allows the recruitment of lymphocytes to different areas, depending 5:57 on the 5:57 holding receptors, etc. I hope that makes sense. So anyway, the lymphocytes are 6:04 not able to 6:04 migrate through into the laminopropia because they have the appropriate 6:09 receptors and chemo-receptors 6:10 which have affinity and attraction for the receptor and chemokines from the l 6:16 aminopropia, 6:17 or within the blood vessel within the laminopropia. So here we have the 6:21 immature, or soon-to-be plasma 6:24 cell, migrate through. And when this B-cell migrates through, it will become an 6:31 activated plasma cell 6:33 with the help of the T helper cell, and it will express IgA antibodies, which 6:38 is the most important 6:39 antibody within the mucosal system. The T cells will also migrate through the 6:44 CD8 T cells and the CD4 6:46 T cells. The CD4 T cells being predominantly T helper cells and the CD8 T cells 6:52 being T killer 6:53 cells, as well as T memory cells. Why do we have T memory cells within the l 6:59 aminopropia or 7:00 we thin the mucosal system? They are actually very important, and we actually 7:04 have a lot of 7:06 T memory cells within the laminopropia, for example. And this is because the 7:11 mucosal immunity is 7:13 continuously exposed to pathogens when we eat, when we do whatever. And so that 7:18 is why we need 7:19 memory of those pathogens so that we can initiate effective immune response 7:24 ASAP. 7:27 So most cells in the laminopropia are effective cells, such as T helper cells 7:31 and also plasma cells, 7:33 as well as memory cells. Within the laminopropia, there is actually more CD4 7:40 cells than CD8 cells, 7:42 about a 3, 2, 1 ratio. And this is because we need CD4 cells to help activate 7:48 macrophages and 7:49 promote its activity. And remember, we need T helper cells in order to activate 7:53 or stimulate 7:54 IgA producing plasma cells, which are very important. Now, there are also cells 8:01 within the layer of 8:03 the epithelial cell, the intra epithelial layer. And these are usually CD8 8:08 cells, T killer cells. 8:09 These cells move within the layer of the epithelial because they actually 8:15 express different 8:17 humming receptors than the lymphocytes in the laminopropia. They express also C 8:23 CR9, but they 8:25 express different integrin, which is alpha EB7 integrin, which is slightly 8:29 different to the alpha 8:30 4B7 integrin on the lymphocytes within the laminopropia. So CD8 cells predom 8:37 inate in the epithelial 8:38 layer, and the CD4 cells predominate in the laminopropia. So why is there an 8:45 abundance of 8:46 CD8 cells within the epithelial? Well, this is because they can kill infected 8:54 cells very easily, 8:56 the epithelial cells, if they are infected very easily. Because remember, the 9:00 mucosal surfaces, 9:02 the epithelial are continuously exposed to pathogens, such as virus. And so, if 9:07 a virus 9:08 infects an epithelial cell, the CD8 cell can kill it very quickly, because it's 9:12 right next to it. 9:13 So let's look at how it does this. The effective function of intra epithelial 9:17 lymphocytes, 9:18 the CD8 T killer cells. So here we have the epithelial aligning, the mucosal 9:24 epithelial 9:24 aligning, and here we have the lumen. And the CD8 cell resides right next to it 9:29 . A virus 9:31 comes along, let's just say, and it goes into the cell and essentially infects 9:36 the cell, 9:37 changes its genetic code. What happens next is that the infected cell will now 9:45 express 9:46 a major histo-compassarly complex molecule with an antigen on it, telling the 9:52 CD8 cell 9:53 essentially to kill it. The CD8 cell, with no hesitation, will kill it. The T 9:57 cell receptor 9:58 will bind on the MHC, and the CD8 receptor will also bind to this as a co-re 10:05 ceptor. 10:06 And this will tell the CD8 cell to essentially kill the infected cell. 10:11 And that is how the CD8 cell protects the mucosal system from further infection 10:19 . 10:19 Dendritic cells also reside within the laminar appropriate, and it has a 10:23 fundamental role 10:24 in taking up antigen and presenting it to the lymphocytes, remember. 10:28 So how the antigen-producing cells, such as dendritic cells, acquire pathogens 10:34 and antigens 10:35 from the laminar appropriate is actually quite unclear, but there are a few 10:40 mechanisms that are 10:41 thought that have been thought of. Remember that within the payest patches in 10:52 the gut, 10:52 the antigen is being brought in by the M cell, the microphone cell. In the l 10:58 aminar 10:58 appropriate, there can be three different ways. There can be an FCRN dependent 11:03 transport with the 11:05 where basically an antibody binds to the antigen and brings it into 11:08 the laminar appropriate where the dendritic cell can then capture it, or the d 11:14 endritic cell itself 11:15 can squeeze within the epithelial gaps and capture the antigen itself, or 11:20 alternatively, 11:21 the pathogen or antigen infects the epithelial cell. The epithelial cell will 11:29 then kill itself 11:30 through apoptosis, releasing the antigen, and now the dendritic cell can 11:34 capture it. 11:35 So those are the three ways where the dendritic cells can obtain an antigen, 11:39 and now by obtaining 11:41 an antigen, the dendritic cell is activated and begins presenting it on an MHC 11:48 class. 11:49 Class 2. And with this MHC class 2, it also begins expressing receptors, 11:55 allowing it to move into the mesenteric lymph nodes, and this is the exact same 12:00 process as 12:00 we see with the dendritic cells from the payest patches. So now the activated d 12:05 endritic cell from 12:06 the laminar appropriate can travel to the mesenteric lymph node to activate the 12:10 lymphocytes, the naive 12:11 CD4 and naive CD8 T cells. The dendritic cell, as well as other cells with the 12:16 laminar appropriate, 12:17 also has a fundamental role in regulating or stopping the activity of CD8 cells 12:23 , the T-killer cells, 12:25 because without regulating their activity, the CD8 cells, the T-killer cells, 12:29 will kill anything 12:30 around it, because they are T-killer cells, they kill things. And therefore, in 12:36 the absence 12:38 of an antigen or a pathogen, dendritic cells, for example, secrete interleukin- 12:43 10, which regulate 12:45 or stop the actions of CD8 cell, keeping them at bay. Of course, the dendritic 12:50 cells can secrete 12:51 other interleukins, which also stops the activity of CD8 cells, as well as 12:56 there are other cells 12:57 within the laminar appropriate, which also regulates CD8 activity, but dend 13:01 ritic cells are usually the 13:02 most notable ones. And finally, as mentioned ages ago, the plasma cell secrete 13:09 IgA-dimeric antibodies, 13:11 and we will talk about IgA-dimeric antibodies at the very end of this video. 13:15 Another very important 13:17 thing to note is that we don't actually find neutrophils, the granulocytes, the 13:22 neutrophils, 13:23 within the laminar appropriate, and around the connective tissue layer or 13:26 beneath the mucosal 13:27 layer. And this is because neutrophils are very self-damaging, and so they're 13:32 usually found within 13:33 the bloodstream. So neutrophils are not present in the mucosal-associated lymph 13:39 oid tissues, 13:40 but they do come in during invasion, or they are recruited during invasion and 13:45 infection, 13:45 because they're important in phagocytizing these antigens pathogens.