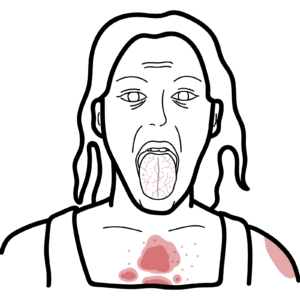
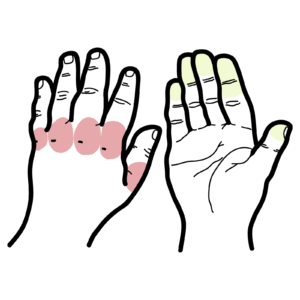
0:00 Systemic lupus erythimatosis, or SLE for short, is an autoimmune disease 0:20 mediated by 0:21 autoantibodies and immune complexes which target nearly every organ in the body 0:26 . 0:26 SLE is a chronic multi-system disorder that most commonly affects women during 0:31 their 0:31 reproductive years. The pathophysiology of SLE involves injury to the body's 0:37 own 0:37 cells leading to damaged cell proteins and their DNA. Injury to a group of 0:44 cells 0:44 can subsequently lead to organ injury. The pathophysiology of SLE is thought to 0:51 involve an interplay between genetics, for example SLE is seen in monozygotic 0:57 twins and there's also influences of epigenetics, immunology factors, hormonal 1:04 factors such as estrogen and mainly environmental factors. Environmental 1:09 factors is thought to be the initial trigger for SLE. These environmental 1:14 factors include UV light, infections such as Epstein-Bavirus, smoking and even 1:22 potentially certain drugs that increases oxidative stress damage that will lead 1:28 to the cells being damaged. Important to note that these environmental risk 1:34 factors are agents which humans are commonly exposed to suggesting that 1:38 people who develop SLE has to have some sort of genetic susceptibility. When 1:45 cells are damaged they can try to repair themselves. If they can't they 1:50 undergo programmed cell death called apoptosis. When cells undergo apoptosis 1:56 internal proteins are displayed on their surface blebs. A normal response is 2:02 when 2:03 our immune system clears up these apoptotic cells. This is done by phagocytes 2:09 such 2:09 as macrophages and monocytes. However if apoptotic cells are not 2:14 cleared efficiently nuclear material is exposed to the immune system which may 2:20 then become sensitized and eventually the immune system will mount an attack on 2:24 our own proteins and nuclear material. Some people who develop SLE are seen to 2:31 have deficiency in some complement proteins such as C1, C2 and C3 and C4. 2:39 These proteins are important to help macrophages clear up certain cells 2:45 such as these apoptotic cells. We mentioned earlier through 2:49 opsinization for example. Deficiency in these early complement proteins mean 2:57 apoptotic cells are not cleared efficiently. When proteins and nuclear material 3:03 are 3:03 not cleared properly they are exposed to the immune system. The immune system 3:08 is 3:08 thought to become sensitized to these materials so next time they encounter 3:13 such a material their body will mount an immune response towards their own 3:18 proteins and nuclear material. The process of sensitization begins when an 3:23 immature antigen-presenting cell such as an immature macrophage or dendritic 3:28 cell 3:28 notices and picks up proteins and nuclear material from the apoptotic cells 3:34 through special receptors such as tall like receptor. The antigen picked up by 3:40 the antigen-presenting cells include nuclear proteins, cytoplasmic proteins 3:46 and membrane components of the cell. Nuclear antigens include histone core, 3:52 double-stranded DNA and ribonuclear protein complexes including SM, NRNP and 4:01 row. Cytoplasmic components also include row, a small variant and cell membrane 4:09 antigens including cardiolipin found in mitochondria and may be platelet 4:14 membranes or red blood cell membrane components as well. Regardless the 4:19 antigens that are picked up by the antigen-presenting cell are then displayed 4:23 on 4:23 the surface of the antigen-presenting cell. 4:27 The antigens are presented to naive T helper cells in nearby lymph nodes. The 4:35 naive T helper when activated can become a number of different types of T 4:40 helper 4:40 cells. In the case of systemic lupus erythematosis where antibodies play the 4:47 main role, interleukin-4 secreted favors T helper 2 cell maturation. T helper 2 4:56 cells promotes the humoral immune response and so the antibody mediated 5:01 immune response. T helper 2 cells stimulate B cell activation and B cell 5:07 proliferation. Activated B cells become plasma cells, the cells responsible for 5:12 producing the antibodies. In this case, autoantibodies which are the antibodies 5:18 towards a person's own antigens. Remember the antibodies produced target the 5:26 antigens which the antigen-presenting cell picked up such as the double 5:31 stranded DNA, the histone, the SM, the row, the cardiolipin. Therefore the 5:38 antibodies produced are autoantibodies because they target self antigens. 5:43 Most of these autoantibodies target the nuclear proteins of the cells which are 5:49 collectively known as ANA. Now these autoantibodies can also form immune 5:56 complexes when exposed to their target antigens. The antigen targeted are 6:01 found in all cells and so these autoantibodies can easily target any cell in 6:06 the body. When the autoantibodies come in contact with nuclear proteins for 6:10 example, a few mechanisms of inflammation can occur. Firstly, through immune 6:16 complex formation and then deposition to organs resulting in complement 6:20 activation augmenting the inflammatory response. The immune complexes can bind 6:26 onto FC receptors of immune cells which will trigger the release of pro 6:30 inflammatory cytokines promoting inflammation. The autoantibodies may 6:36 bind on antigens on the cell surface or directly into the internal proteins 6:41 resulting in complement activation and release of cytokines from the cell. 6:46 Finally, the immune cells around the area are eventually sensitized to the 6:50 antigens and so when the Toleric Receptor detects nuclear antigens for example, 6:55 they will release cytokines promoting the inflammation, the inflammatory 6:59 response. 7:00 These different mechanisms cause inflammation to the surrounding area 7:05 causing further organ injury and damage. This will further cause a cascade of 7:11 damaged cells and the cycle continues. 7:15 Once the inflammation settles through the intrinsic regulation of the immune 7:21 system, the body will slowly recover. However, SLE is an ongoing chronic 7:27 illness. 7:27 A feature of SLE are its flare-ups. Flare-ups or flares in SLE appears to 7:35 reflect immunologic memory. Flare-up occurs in response to another exposure of 7:41 the 7:41 antigen so really any precipitating factor that causes cell or mass cell 7:47 apoptosis can trigger flare-ups and apoptosis exposes the nuclear materials 7:53 to the immune cells. Precipitating factors include sun exposure, infections, 8:00 stress, 8:02 surgery and pregnancy. 8:06 Patients with SLE generally have higher numbers of B cells, plasma cells, 8:17 plasma 8:18 blasts which are the immature plasma cells and higher proportions of activated 8:22 T 8:23 cells than normal individuals. Cytokines which stimulate B cell activation 8:28 include 8:29 interleukin-6 and interleukin-10. At least 50% of patients with SLE have 8:35 increased levels of B lymphocytes stimulator, a growth factor for B-cell 8:41 survival, maturation, antibody production and differentiation into plasma cells 8:48 . 8:49 Risk factors for SLE is up to 20 times more common in women than men and most 8:55 likely to develop between the ages of 15 to 40 years. Female-6 is a risk factor 9:00 due 9:00 to the role of hormones which increases the susceptibility to develop SLE. 9:07 One characteristic of the immune response is the ability of our body to 9:14 create immunological or immunologic memory. That is memory immune cells that 9:20 are ready to mount a response when they encounter the same antigen again. 9:25 Flares in SLE as mentioned appear to reflect immunologic memory occurring in 9:32 response to exposure of the antigens again. The long-lived plasma cells as the 9:39 name suggests are plasma cells which live longer and typically reside in the 9:42 bone marrow. Long-lived plasma cells can remember the same antigen when exposed 9:47 to it again and begin secreting more auto antibodies to help. Finally to 9:54 complete the diagram we talked about T helper 2 cells which help mount the 9:58 humoral immune response. Then there is a T helper 1 cells is the other arm of 10:04 the 10:04 T helper activation. However, T helper 1 cells promote the cell-mediated immune 10:08 response and so do not play a big role in the pathophysiology of SLE. 10:15 There are many signs and symptoms of SLE. Most complain of constitutional 10:22 symptoms such as fatigue, myalgia, weight loss, and fever. The most common 10:28 symptom 10:28 or sign is a UV sensitive butterfly rash over the nasal bridge and malabones 10:34 which 10:34 occur in 50% of people. Individuals can also be sensitive to life. The other 10:40 cutaneous features include dissquared rash. 10:46 Neurological involvement is common and include cognitive impairment which is 10:54 very common. Headache seizures which is and seizures are these uncontrolled 11:00 electrical firing in the brain, delirium and psychosis as well as peripheral 11:05 neuropathies. Pulmonary involvement include interstitial fibrosis and 11:11 pulmonary vasculitis. Pulmonary pleuritis and pleural effusions are seen in one 11:18 third of patients and are usually small. 11:22 Cardiovascular involvement include pericardial disease which tend to be 11:28 asymptomatic unless pericardial effusion becomes so big it will cause symptoms 11:33 of 11:33 chest pain and difficulty breathing. Asymptomatic myocarditis is also common 11:38 and there's also risk of valvular heart disease. Hypertension is a common 11:44 complication of SLE and has to be well managed. Hypertension is probably due 11:49 to complications of renal involvement seen in SLE. Renal involvement is seen 11:56 in at least one third of SLE patients and this is called lupus nephritis where 12:02 the antibodies and the antibody complex is deposits at the glomerulus, the 12:08 functional units of the kidneys and long term this can lead to renal failure. 12:14 Gastrointestinal involvement include these nonspecific abdominal pain, nausea, 12:19 vomiting that can be hepatomegaly and ulcerations as well which tend to be 12:24 from medications. Hematological involvement occurs in about half the 12:30 patients and include chronic anemia and leucopenia. Also can have complications 12:34 from the immunosuppressive drugs used to treat SLE which can also cause the 12:39 same things. Moscular skeletal findings include aulthralgia and arthritis which 12:44 is common. Morning stiffness and polyarticula symmetrical aulthralgis or 12:49 arthritis occur 90% of the cases. Patients with SLE can experience 12:54 Reynolds phenomenon which is an episodic palae or sinosis of the fingers due to 13:00 vasoconstriction of the arterioles in the fingers in response to cold or 13:04 emotional stress. Finally osteopenia and osteoporosis is important part of SLE 13:11 and is a multi-factorial cause in SLE which we will learn about later. 13:18 Investigations for work up for SLE include a full blood count, electrolyte urea 13:24 creatinine to look for kidney function, LFTs, liver involvement and CRP/ESR for 13:31 inflammation. Urine tests which involve urinalysis, urine microscopy and 13:36 urinary albumin-cranine ratio is very important to monitor kidney function. 13:42 SLE serum markers must be ordered. These serological markers are essentially 13:47 antibodies detected against self antigens. The antigens we discussed which 13:53 include nuclear proteins, cytoplasmic and cell membrane components. These 13:58 serological markers include antibodies against double-stranded DNA. If you can 14:04 find antihistamine, anti-SM, anti-RO, anti-NRNP, all these antibodies target 14:11 different nuclear proteins. Anti-nuclear antibody or ANA is another test to 14:16 order which really encompasses all these antibodies. ANA should be ordered in 14:21 someone suspected of having SLE or any connective tissue disease. Then there's 14:26 other tests such as DNA, anti-cardiolipin and anti-rheumatoid factor. 14:32 Serum markers associated with disease flare-ups include reduced complement 3 14:37 and complement 4 and increase in anti-double-stranded DNA. 14:44 Remember to think about drug-induced systemic lupus erythematosis for 14:49 someone with no history of SLE, someone who also recently began a new drug and 14:54 has a positive ANA. Management of SLE involves just general principles such as 15:03 avoiding UV light exposure, vitamin D and calcium supplements, reduce the 15:09 cardiovascular risk through weight loss, stop smoking, stop alcohol, and also 15:14 managing the cholesterol. Now to understand how the pharmacological drugs 15:19 help in SLE, let's quickly revise the immune response again. So remember 15:25 antigen 15:26 presenting cells presents a self antigen to the T helper cell. Interleukin 2 is 15:31 a 15:31 cytokine which stimulates T helper activation and proliferation. The interleuk 15:36 in 4 15:37 is one that helps produce T helper 2 cells which then activates and promotes 15:43 B cell activation. Activated B cells become plasma cells which produce 15:48 Odo antibodies, a hallmark of SLE. Examples of pharmaceutical used in SLE 15:58 include tachylimus which is a calcineurin inhibitor, inhibiting interleukin 2 16:03 production and function. This will suppress T cell activity. Mycofenolate and 16:09 as a 16:10 thyroid purine are drugs which reduce lymphocyte activity both B and T cells 16:16 suppressing the immune system. Belumimab is a monoclonal antibody that blocks 16:24 the 16:25 B lymphocyte stimulator. Remember this molecule which is over expressed in 16:29 people with lupus, promotes the survival and differentiation of B cells, 16:34 inhibiting it therefore aims to reduce antibody producing B cells. During the 16:41 inflammatory process in SLE specifically during the flare-ups, immune cells and 16:46 damaged cells release pro-inflammatory cytokines, glucocorticoids are a main 16:52 state for SLE and help suppress this inflammatory response. NSAIDs are also 16:58 useful especially for musculoskeletal pain associated with SLE. Control blood 17:04 pressure as mentioned is important in SLE, anti-hypertensors are therefore 17:08 important. 17:10 The complications of SLE include osteoporosis and this is due to many factors. 17:19 Low vitamin D from low sun exposure in patients with SLE, renal osteodystrophy 17:25 from renal impairment, steroid use which increases risk of osteoporosis, age 17:31 and 17:31 being female as low fluctuating estrogen levels increases the risks of 17:35 osteoporosis. Other complications include anti-phospholipid syndrome 17:40 occurring in one third of patients with SLE. Remember also that SLE increases 17:47 the 17:47 risk of non-hunchkins lymphoma. 17:55 you