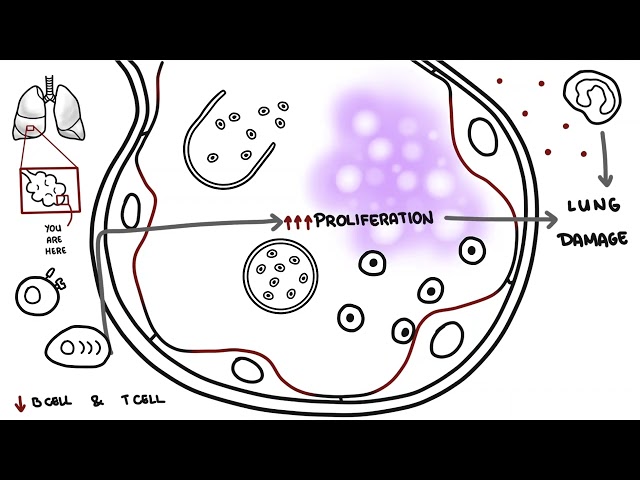
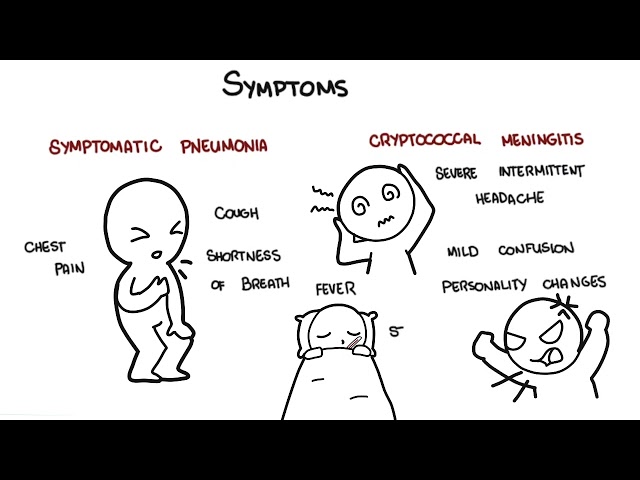
0:00 Interstitial lung disease, also known as diffuse parenchymal lung disease, are 0:10 a group of disorders 0:12 based on similar clinical, radiographic, physiologic and pathologic changes. 0:18 When people think about interstitial lung disease, they think about fibrosis, 0:22 restriction 0:23 in the lungs. 0:24 And there are many, many causes of interstitial lung disease. 0:27 So interstitial lung disease, or diffuse parenchymal lung disease, is more of 0:32 an umbrella term. 0:41 Interstitial means the interstitium, which is where the disease process often 0:45 begins. 0:46 The interstitium is between the alveoli and capillaries of the lung. 0:52 Their interstitial fibroblasts produce lots of products, such as collagen, and 0:57 they proliferate 0:58 producing more collagen and extracellular matrix substances. 1:04 These interstitial changes are what causes the restrictive parenchym. 1:10 However, in reality, the disease affects more than the interstitium. 1:14 It affects the alveoli walls, and often the related small airways and distal 1:19 pulmonary 1:20 vasculature. 1:21 And so diffuse parenchymal lung disease is more appropriate name of the disease 1:26 rather than 1:27 interstitial lung disease. 1:29 And again, these interstitial changes causes an abnormality in gas exchange, so 1:35 you have 1:36 an impairment in gas exchange between oxygen and carbon dioxide. 1:44 Like other lung diseases, these disorders present primarily with shortness of 1:48 breath, 1:49 usually chronic over weeks, two months, without response to initial treatment 1:54 of puffers. 1:55 It's associated with a non-productive cough. 1:59 If there's clinical suspicion of diffuse parenchymal lung disease, they should 2:03 undergo full pulmonary 2:04 function test. 2:06 You want to identify a restrictive lung disease, which is identified by a 2:10 reduced total lung 2:12 capacity and vital capacity. 2:20 You also want to check the DLCO, which would be low. 2:24 The DLCO is the diffusing capacity of the lung for carbon monoxide. 2:29 It measures the ability of the lungs to transfer gas from inhaled air to the 2:33 red blood cells 2:34 in pulmonary capillaries. 2:37 A low DLCO, combined with reduced lung volumes, suggest diffuse parenchymal 2:44 lung disease. 2:45 A low DLCO, because gas is unable to transfer through the diseased alveoli 2:52 interstitial 2:53 main capillaries. 2:55 A normal DLCO associated with low lung volumes is consistent with an extra 3:02 pulmonary cause 3:03 of restriction. 3:07 An extra pulmonary cause of restriction means something outside the lung 3:13 causing restriction 3:14 of the lung, so restricting the lungs to expand. 3:17 This includes obesity, plural effusion, or plural thickening, neuromuscular 3:28 weakness, 3:32 or kifosis, as well as many other causes. 3:39 A normal chest radiograph, or chest x-ray, does not rule out diffuse parenchym 3:44 al lung 3:44 disease. 3:45 The diagnosis of diffuse parenchymal lung disease can often be made based on 3:49 high-resolution 3:50 CT without a lung biopsy, so high-res CT of the chest is gold standard, you can 4:00 say. 4:01 As mentioned, diffuse parenchymal lung disease is an umbrella term, because 4:04 there are so 4:04 many causes, but the hallmark is the same, you know, you have the restrictive 4:10 pattern 4:10 with the reduced DLCO. 4:12 The diffuse parenchymal lung disease are divided into those that are associated 4:16 with 4:16 the known cause of diffuse parenchymal lung disease, or unknown cause of 4:23 diffuse parenchymal 4:24 lung disease, or weed and wonderful rare causes. 4:29 So let's look at each of these in a bit more detail. 4:32 So known causes of diffuse parenchymal lung disease include drug-induced, 4:37 smoking-related, 4:40 radiation-induced, interstitial changes, chronic aspiration, secondary from, 4:45 let's 4:46 just say, gastro-sophageal reflux, pneumoconiosis, which is like worker's lung, 4:51 connective tissue 4:52 disease, including, you know, SLE, rheumatoid arthritis, chloroderma, hypers 4:58 ensitivity pneumonitis, 5:00 which is essentially a response to an allergens, which is a hypersensitivity 5:07 reaction. 5:07 Then you have the unknown causes of diffuse parenchymal lung disease, and this 5:11 includes 5:12 idiopathic interstitial pneumonia, which comprises of three main ones, idiopath 5:16 ic pulmonary fibrosis, 5:18 which is a classic honeycomb appearance on CT chest, acute interstitial 5:24 pneumonia and 5:24 cryptogenic organizing pneumonia, which looks like just pneumonia in both lungs 5:30 , patchy 5:31 or throughout subplural. 5:33 Then you have sarcoidosis, which can present as a diffuse parenchymal lung 5:37 disease as in 5:38 a late stage, and this is a classic mediasthenyl lymphadenopathy. 5:43 Finally, you have the rare causes of diffuse parenchymal lung disease with well 5:47 -defined 5:48 features. 5:49 This includes lymphangioliomyomatosis, icedophilic pneumonia, pulmonary alve 5:57 olar proteinosis, 5:59 pulmonary langerhand cell hysteocytosis, or hysteocytosis X, and there are many 6:07 other 6:07 types of diffuse parenchymal lung disease, which I've not mentioned, but these 6:11 are the 6:11 main ones. 6:12 I hope to create videos on the main diffuse parenchymal lung disease soon. 6:19 Some high yield points to remember when approaching a diffuse parenchymal lung 6:23 disease, or interstitial 6:24 lung disease, or any other lung disease for that matter is to consider which 6:30 areas of 6:30 the lungs these disease affects, because some of these lung diseases affect 6:36 having upper 6:37 lobe predominance, and other diseases have a lower lobe predominant disease. 6:46 So let's look at upper lobe predominant disease. 6:50 With this, you can remember the different causes by the acronym breast. 6:55 So B is for beryllosis, which is a type of pneumoconiosis, R is for radiation 7:01 fibrosis, 7:02 E is for e-cinephilic pneumonia as well as hypersensitivity pneumonia, which 7:07 have e-cinephils. 7:08 A is for allergic bronchopulmonary aspergillosis, as well as ankylosing spondyl 7:14 itis, which is 7:15 a type of rheumatic connective tissue disease, S is for sarcoidosis, T is for 7:22 tuberculosis. 7:24 Remember sarcoidosis is typically mediastinol, but it also has upper lobe 7:28 predominance. 7:29 S is for silicosis, and again this holds true for majority of pneumoconiosis 7:36 that they have 7:38 upper lobe predominance. 7:40 Interestingly, they also present with small nodules typically in the upper lob 7:48 es. 7:49 For lower lobe predominance disease, you can remember the different causes by 7:53 the acronym 7:53 AIDS, so A is for aspostosis, I is for idiopathic pulmonary fibrosis, which is 7:59 the classic honeycomb 8:01 changes on CT chest, D is for drug-induced fibrosis, and there's 3-2 remember, 8:09 amioderone, 8:11 nitroferon toen and methotrexate, S is for scleroderma and other connective 8:17 tissue disease. 8:20 Remember that ankylosing spondylitis is the only one of the rheumatic diseases 8:24 that typically 8:24 affects the upper lobes, upper zones of the lungs. 8:29 So breasts for upper lobe predominance disease and AIDS for lower lobe predomin 8:36 ance disease. 8:37 The clinical manifestation of diffuse parenchymal lung disease is worsening dys 8:43 nia with associated 8:44 usually non-productive cough. 8:50 It's important to also know the occupational history as well as exposure 9:01 history, which 9:02 can help identify potential causes of cole workers lung or other pneumoconiosis 9:09 , as well 9:09 as exposure to birds and pets which may help diagnose hypersensitivity pneumon 9:13 itis, which 9:14 is the allergic response. 9:18 Medication history is also important, such as amioderone causing interstitial 9:21 lung disease. 9:24 On examination lung sounds are variable, it can be normal, it can have a wheeze 9:29 , it can 9:29 be you can have velcro-inspiratory crackles, which are pathinemonic for classic 9:34 idiopathic 9:35 pulmonary fibrosis. 9:38 Especially with diffuse parenchymal lung disease, patients develop some form of 9:42 pulmonary hypertension. 9:44 And so they can have features of right heart strain or heart failure. 9:49 And this typically represents severe disease. 9:53 You can imagine a fibrous lung, this will increase pressure in the pulmonary 9:59 capillaries, 10:00 which means it will increase pressure in the pulmonary arteries, which will 10:03 lead to increased 10:04 pressure on the right side of the heart, so right heart strain. 10:09 And this is really what pulmonary hypertension is. 10:12 So features of pulmonary hypertension and right heart failure include a raised 10:17 JVP, 10:17 peripheral edema, a loud P2, as well as an S3 heart sound. 10:24 Some diffuse parenchymal lung disease have features of clubbing, namely idiop 10:28 athic pulmonary 10:29 fibrosis. 10:30 However, clubbing is not specific for diffuse parenchymal lung disease. 10:35 Other causes of clubbing include cystic fibrosis, cyanotic heart disease, 10:40 cancer of the lungs 10:41 and pleura, as well as colitis, inflammatory bowel disease. 10:48 Patients may have borderline normal pulse oximetry at rest. 10:54 But on ambulation, a 4% drop is consistent with, really, a diffusion limitation 11:02 . 11:02 Finally, the six-minute walk test is a useful test to assess functional status 11:06 in patients 11:07 with diffuse parenchymal lung disease and to check response to any treatment. 11:12 So you can do the six-minute walk test again after treatment to check if they 11:17 've improved. 11:18 Thank you for watching. 11:19 If you enjoyed this video on an overview of diffuse parenchymal lung disease, 11:24 there will 11:24 be some links to watch the specific causes of diffuse parenchymal lung disease 11:29 in more 11:29 detail. 11:30 Thank you.