Chronic Lower Limb Ischaemia: Intermittent Claudication
Chronic lower limb ischemia can be classified using the Fontaine classification:
Grades III and IV are classified as Critical Limb Ischemia.
Intermittent claudication is a type of chronic lower limb ischemia that presents with muscle pain on exercise and is relieved on rest2. It affects 4% of people over 55, mostly men1. Up to 60% of patients have an underlying coronary or carotid disease. Around 40% experience stroke within 5 years of presentation3.
Peripheral artery disease (PAD) is a chronic obstruction of arteries supplying the extremities, usually caused by atherosclerosis; it is more common in the lower limb.
Intermittent claudication (IC) is defined by leg muscle pain, cramping and fatigue brought on by exercise; relieved on rest and caused by inadequate blood supply; it is the primary symptom of peripheral arterial disease (PAD).
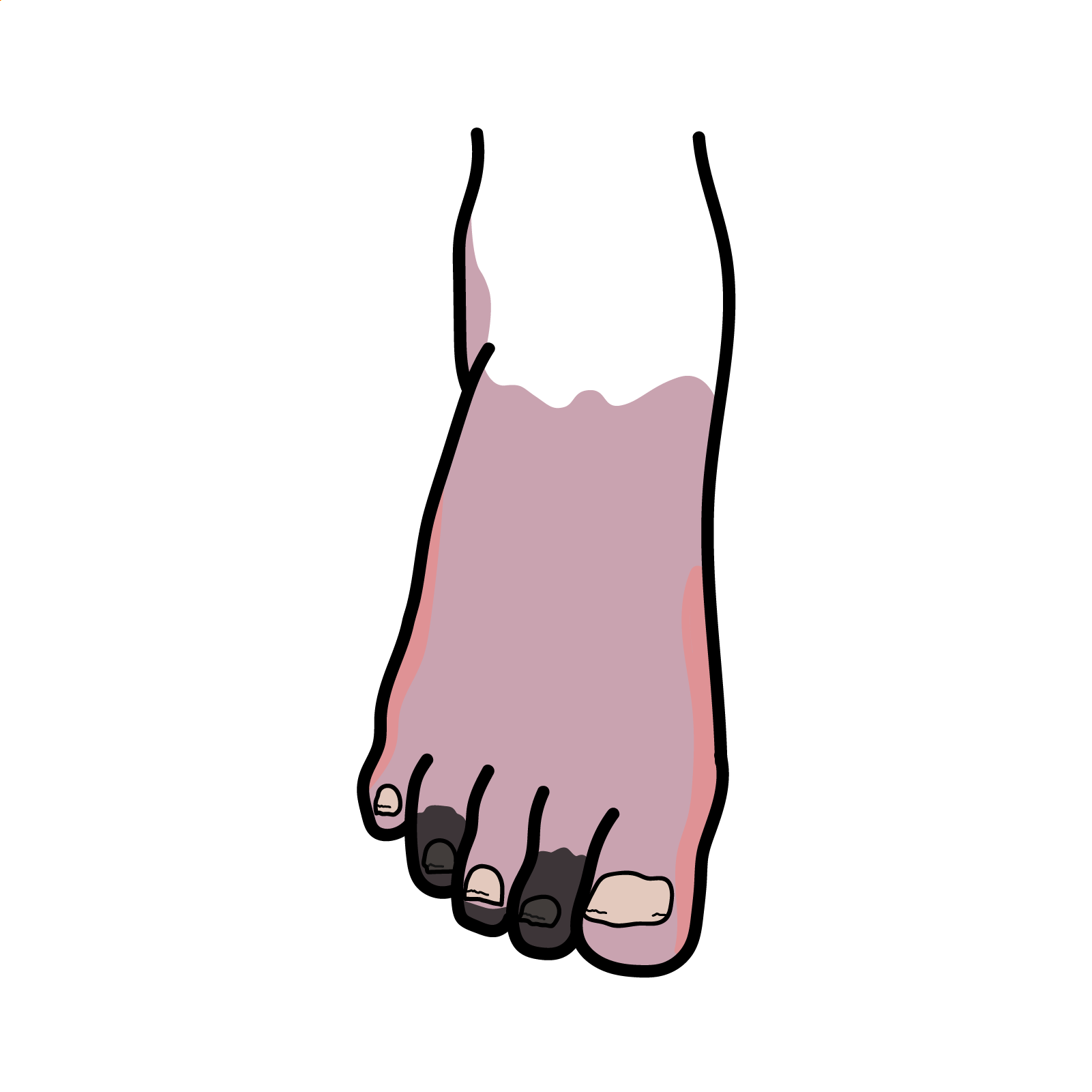
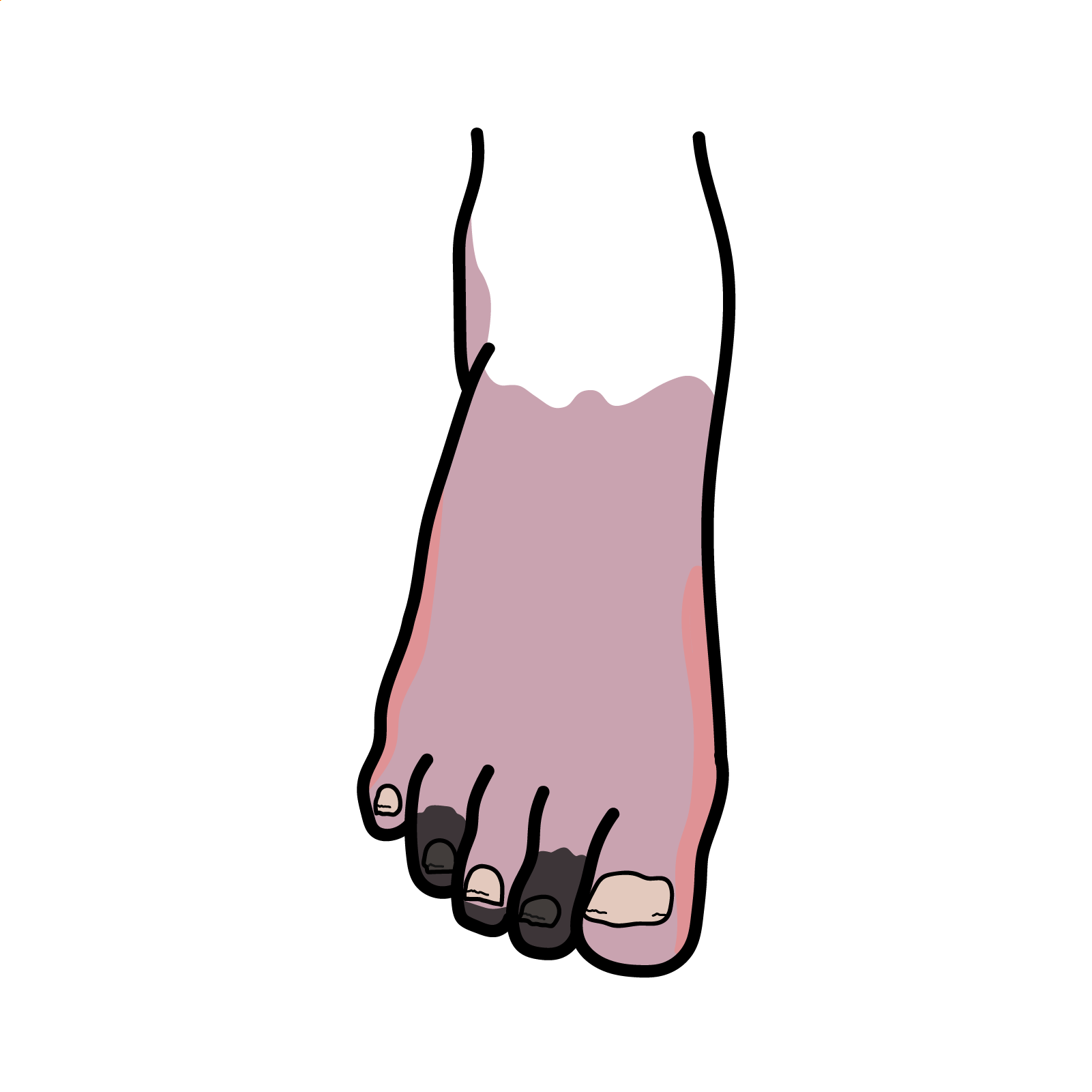
Critical limb ischemia is a severe form of chronic lower limb ischemia, which presents with tissue wounds like ulcers and gangrene, and rest pain worse at night and relieved by hanging the limb dependent.
Acute limb ischemia is defined by a rapid drop in arterial blood flow resulting in cessation of nutrient and oxygen delivery to the tissues.
Most common sites involved are femoral and popliteal arteries3
| Parent Artery | Major Branches |
| Abdominal Aorta | Common Iliac Arteries |
| Common Iliac Artery | External Iliac Artery |
| Internal Iliac Artery | |
| External Iliac Artery | Femoral Artery |
| Femoral Artery | Deep Femoral Artery |
| Superficial Femoral Artery | |
| Deep Femoral Artery | Medial Femoral Circumflex Artery |
| Lateral Femoral Circumflex Artery | |
| Superficial Femoral Artery | Popliteal Artery |
| Popliteal Artery | Anterior Tibial Artery |
| Posterior Tibial Artery | |
| Posterior Tibial Artery | Fibular (Peroneal) Artery |
| Medial Plantar Artery | |
| Lateral Plantar Artery | |
| Anterior Tibial Artery | Dorsalis Pedis Artery |
| Dorsalis Pedis Artery | Arcuate Artery |
| First Metatarsal Artery | |
| Arcuate Artery | Second, Third and Fourth Metatarsal Arteries |
Buerger’s disease is acute inflammation and clotting of arteries and veins in hands and feet; it can lead to blockages and cause ischemia.
Popliteal artery entrapment syndrome is defined as compression of popliteal artery by surrounding muscles, particularly during exercise.
Atherosclerosis in the peripheral arteries of legs leads to an inadequate blood supply due to narrowing or hardening of the arteries. During exercise, increased oxygen demand leads muscles to operate anaerobically, producing lactic acid and other metabolites, which further lead to leg pain, aching, cramping or numbness in the calf, buttock, hip, thigh or arch of the foot. Lactic acid and other metabolites get washed away on rest, but the condition reiterates on further exercising.3
Erectile dysfunction → think aortoiliac disease (Leriche syndrome).
Examination
Chronic compartment syndrome: increase in pressure in a closed muscle compartment during activity leading to compression of blood vessels and nerves, causing swelling, tightness and pain.
Ankle-brachial Pressure Index (ABPI)
Segmental blood pressure (measured at various points along the limb to help localise disease)
Imaging:
ABPI (Ankle-brachial Pressure Index) is used to assess blood flow in legs. It is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure at the arm (brachial artery). ABPI values:1.0 – 1.4 – normal0.9 to 0.5 – intermittent claudication<0.5 – critical limb ischemia>1.4 – calcified vessels.
Risk factor modification is first-line:
Endovascular treatment:
Surgery:
Statins are drugs used to lower blood cholesterol and prevent progression of atherosclerosis. Mechanism of action: inhibit the enzyme HMG-CoA reductase, which is used to make cholesterol. They are used to reduce risk of heart attack, stroke and other ischemia. Side effects: myalgia (muscle pain) is most common, it can lead to rhabdomyolysis (breakdown of muscle fibers). Examples: rosuvastatin and atorvastatin.
Angioplasty is a procedure used to dilate narrow arteries. A catheter is placed in the vessel and a balloon is inflated at the point of narrowing causing the vessel lumen to dilate. A stent is often left in place to prevent recurrent narrowing.
Endarterectomy is a surgical procedure used to remove an atheroma (fatty buildup inside an artery). An incision is made in the arterial wall and the atheroma is removed; the vessel wall is then stitched back together. This procedure is used to prevent complications like stroke and limb ischemia.
Aspirin as an antiplatelet inhibits the COX-1 enzymes, reducing synthesis of thromboxane A2, which results in decreased platelet aggregation and reduced risk of thrombus formation. Aspirin can also be used to relieve pain, reduce inflammation and lower temperature. Side effects: gastrointestinal irritation, bleeding.
Complications
Critical limb ischemia is defined as grade III and IV chronic lower limb ischemia, while intermittent claudication is grade II.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion