Overview
Stroke is the third leading cause of death and a principal cause of long-term disability in much of the industrialized world. Stroke is often caused by atherosclerotic lesions of the carotid artery bifurcation. 10% of all strokes are due to carotid disease. The degree of internal carotid artery stenosis is the most important predictor of cerebral infarction among patients with extracranial carotid artery disease.
| Side note 30% of patients who present with suspected stroke have a ‘stroke mimic’ such as tumour, subdural haematoma, migraine, hypoglycaemia, postictal paralysis or cerebral abscess. |
| Definition Stroke: The development of an acute stroke or transient ischaemic attack is a medical emergency. Transient Ischaemia attack (TIA): Minor stroke or transient ischaemic attack, characterized as a brief episode of neurologic dysfunction caused by focal cerebral ischaemia without infarction. TIA is characterised by absence of infarction on imaging. Atherosclerosis: Progressive disease characterized by the accumulation of lipids and fibrous elements in the large arteries (plaque) Carotid artery stenosis: Typically the result of atherosclerosis at the bifurcation of the common carotid artery or in the origins of either the internal or the external carotid artery. Carotid body tumour |
| Remember Initial mortality of an ischaemic stroke ranges from 15-30%. Survivors remain at a high risk of subsequent stroke (50% of patient will experience a second event in 5 years). |
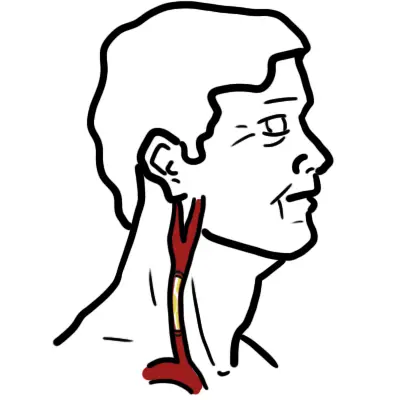
Anatomy of the Carotid Artery
The common carotid artery arises from the aortic arch (the right common carotid from the brachiocephalic trunk.
The common carotid artery gives rise to the internal and external carotid artery at the level of C6
The main branches of the supraclinoid artery (OPAAM)
- Opthalmic artery
- Posterior communicating artery
- Anterior communicating artery
- Anterior cerebral artery
- Middle cerebral artery
Each common carotid is contained within the carotid sheath which is derived from all 3 layers of the deep cervical fascia. In addition to containing the common carotid artery, the sheath also comprises the:
- Internal jugular vein
- Vagus nerve
Aetiology and Risk Factors
Risk Factors
- Advancing age
- Male gender
- Smoking
- Family history
- Atherosclerosis
- Hypertension
- Hypercholesterolaemia
- Other vascular aneurysm
Pathophysiology
The pathology of cerebrovascular disease (stroke or TIA) can be of:
- Intracranial origin
- Extracranial origin
- Flow-restrictive lesions - most common carotid artery stenosis
- Embolism
Carotid Artery Stenosis pathophysiology
- Artherosclerosis formation in carotid artery.
- Plaque instability and rupture create thromboembolic debris and lead to neurological injury.
- Plaque ulceration and thrombosis are associated with neurological symptoms, independent of the degree of stenosis
- During periods prone to ischaemia, collateral flow is critical for cerebral blood flow compensation and a major determinant of the severity of the ischaemic insult.
- Other factors include plaque morphology, duration of hypoperfusion, characteristics of the embolus, and cerebral vasoreactivity.
| Remember the most common lesion found in patients with extracranial cerebrovascular disease is an atherosclerotic plaque in the carotid bifurcation. This produces symptoms by reducing blood flow, by releasing embolic material. |
| Side note Carotid atherosclerosis and coronary atherosclerosis has distinct differences. Plaque ulceration, with embolisation of large amounts of necrotic core, is a common feature of carotid atherosclerosis. |
Another mechanism for infarction with carotid stenosis is a sudden drop in systemic blood pressure → ACA-MCA water-shed territory.
Clinical Manifestation
- Asymptomatic
- Transient Ischaemic Attack
- Stroke
| Think Although carotid artery stenosis is one of the main causes of cerebrovascular disease, the aortic arch should always be assessed as this too is a site for atherosclerosis. |
Middle cerebral artery occlusion
- Contralateral face-arm weakness
- Contralateral face-arm-leg weakness
- Contralateral sensory changes
- Contralateral visual field defects
- Aphasia or neglect
- +/- Ipsilateral monocular visual loss caused by occlusion to the ophthalmic artery (amaurosis fugax)
Clinical Examination
- Bruits over carotid arteries (best heard with the bell)
Diagnosis
Differential Diagnosis of Carotid artery disease
- Arteriosclerotic disease (most common)
- Non arteriosclerotic
- Fibromusclar dysplasia
- Dissection
- Vasospasm
- Aneurysm
- Arterio-venous fistula
- Takayasu arteritis
- Carotid body tumour
| Takayasu arteritis, a rare type of vasculitis, first described by Takayasu who say nonspecific type of arteritis in a 21 year old woman with peculiar capillary flush, with rust like arteriovenous anastomoses around the papilla and blindness owing to cataracts. |
Investigations
- Ultrasound carotids
- Doppler
- CT angiogram carotids (gold standard)
Treatment
Indications for intervention
- Symptomatic
- Stenosis >70%
- High risk of stroke
Medical Management
- Lifestyle modification
- Antiplatelets
- Statins
- Blood Pressure control
| Remember Patients with asymptomatic carotid stenosis ≤70% are managed with pharmacological therapy. |
Surgical Management
- Carotid endarectomy
- Carotid artery stenting
| Carotid endarterectomy is a procedure where the carotid artery is exposed surgically and temporarily clamped, the atherosclrotic material is shelled out, restoring cerebral blood flow and reduces the risk of cerebral ischemia. |
| Side note Carotid endarterectomy |
| Severe stenosis - between 70-99% luminal diameter - of the origin of the symptomatic internal carotid artery |
| Patients with a carotid stenosis of less than 70% or who have a totally occluded carotid artery do not benefit from carotid artery surgery and are best treated medically |
| All patient should receive best medical treatment (control of blood pressure, antiplatelet agents, cholesterol lowering through diet and drugs, lifestyle advice) |
Complications and Prognosis
Complications of stenosis
- Ischaemic stroke and all that comes with it
- Depression
Complications of endarterectomy and artery stenting
- Postoperative cerebral haemorrhage
- Cranial nerve injury
- Haematomas
- Stroke
- Myocardial infarction
Prognosis
- Prognosis depends of degree of stenosis
- Patients with a carotid stenosis of less than 70% or who have a totally occluded carotid artery do not benefit from carotid artery surgery and are best treated medically.