Chronic Upper Limb Ischaemia
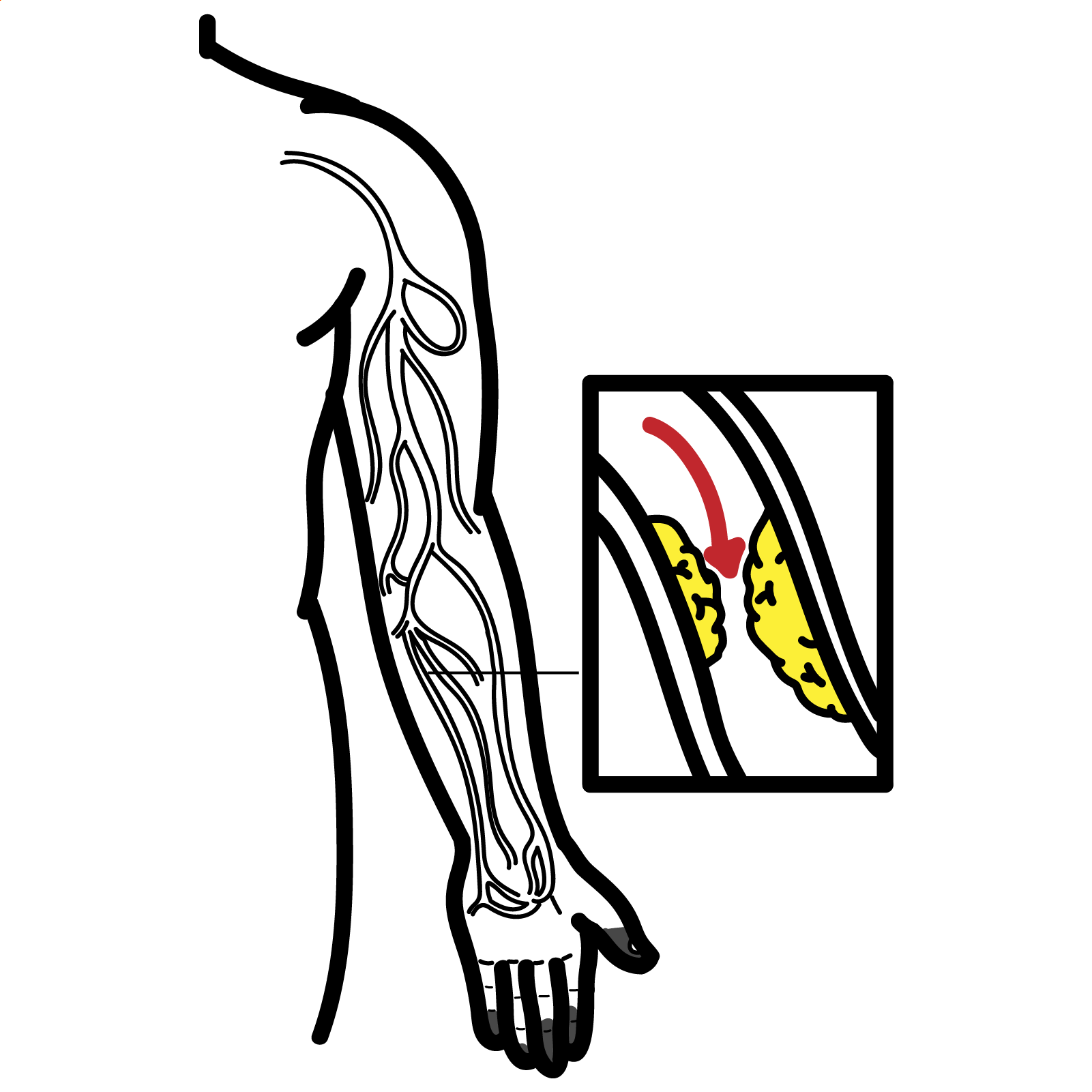
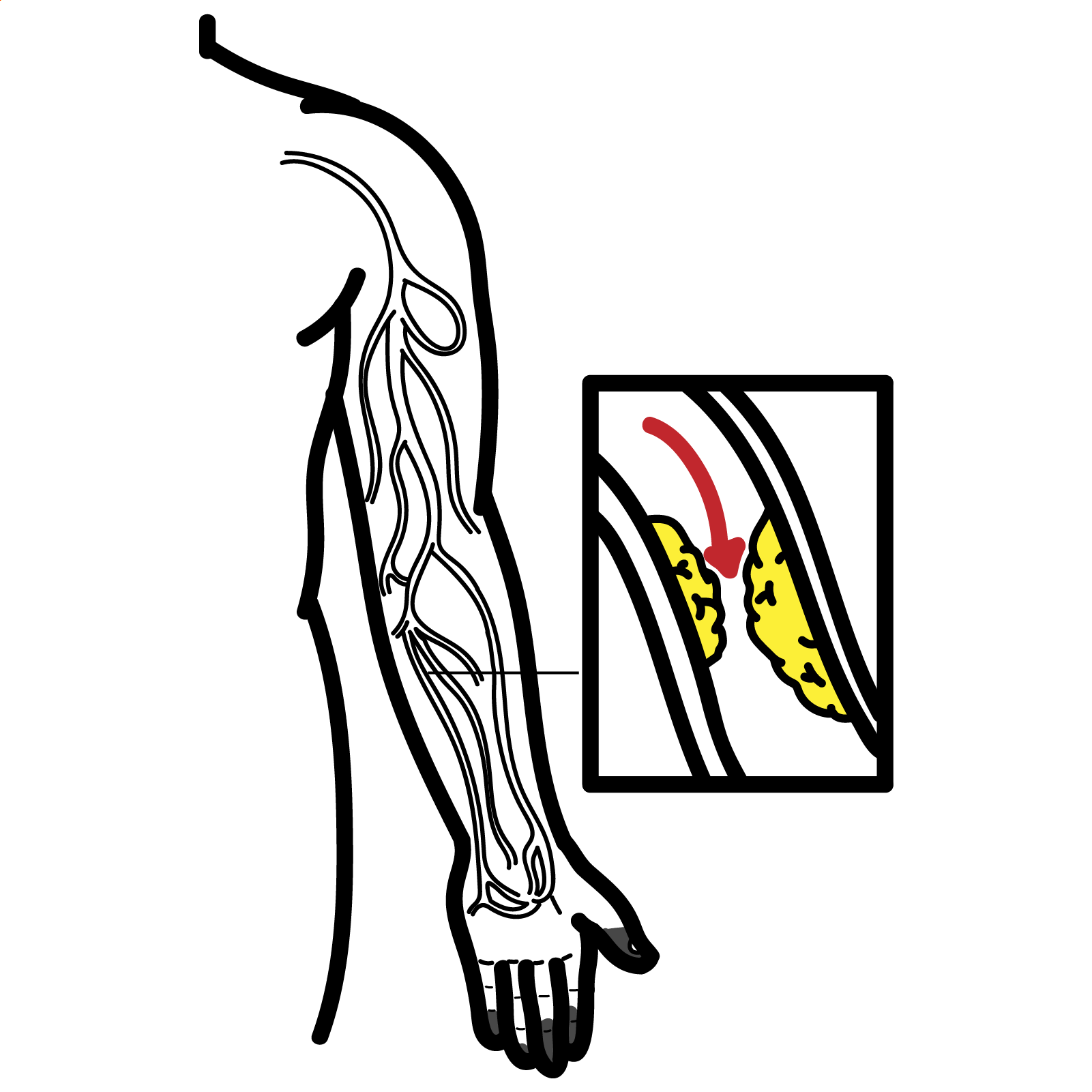
Chronic upper limb ischaemia is a form of peripheral arterial disease that results in a symptomatic reduced blood supply to the upper limb. The common symptoms are weakness, cramps, pain, and digital ischaemia/gangrene. Upper limb ischaemia occurs less frequently than lower limb ischaemia.
Peripheral artery disease (PAD) is a chronic obstruction of arteries supplying the extremities, usually caused by atherosclerosis; it is more common in the lower limb.
Chronic upper limb ischaemia refers to a reduction in arterial blood flow to the upper extremity due to progressive occlusion of vessels.
Acute limb ischaemia is defined by a rapid drop in arterial blood flow resulting in cessation of nutrient and oxygen delivery to the tissues.
| Parent Artery | Major Branches |
| Aortic arch | Left subclavian artery |
| Left common carotid | |
| Brachiocephalic trunk | |
| Brachiocephalic trunk | Right subclavian artery |
| Right common carotid artery | |
| Subclavian artery | Axillary artery |
| Vertebral artery | |
| Axillary artery | Brachial artery |
| Anterior humeral circumflex artery | |
| Posterior humeral circumflex artery | |
| Brachial artery | Deep brachial artery |
| Radial artery | |
| Ulnar artery | |
| Radial artery | Deep palmar arch (main contributor) |
| Superficial palmar arch | |
| Ulnar artery | Deep palmar arch |
| Superficial palmar arch (main contributor) | |
| Superficial palmar arch | Common palmar digital arteries |
| Common palmar digital artery | Proper palmar digital arteries |
Most common sites involved are subclavian, axillary and brachial artery.
Acute upper limb ischaemia presents suddenly with the “6 P’s” (pain, pallor, pulselessness, paraesthesia, paralysis, perishingly cold) due to embolism or thrombosis, whereas chronic upper limb ischaemia develops gradually from atherosclerosis or compression, allowing collaterals and causing exertional symptoms like claudication rather than sudden limb threat.
Excess use or injury of shoulder increases the likelihood of anatomical change, which increases the risk of potential vessel obstruction.
Progressive arterial narrowing leads to reduced perfusion, which results in chronic hypoxia. This forces the tissue to rely on anaerobic respiration and leads to build up of lactic acid that activates pain receptors. As the hypoxia worsens, the tissue slowly starts to undergo necrosis. The blood supply may be compensated by collateral vessel formation but this is not always sufficient, especially in severe occlusions or during increased demand.
Examination
Obstruction of subclavian artery is characterised by bruits in the supraclavicular fossa and blood pressure difference between the two arms of >15-20 mmHg. More distal obstruction will not cause such a large discrepancy in blood pressure between the two arms.
Wrist-brachial index (WBI)
Segmental blood pressure (measured at various points along the limb to help localise disease)
Imaging:
Pathology of neurological origin can be differentiated by the presence of normal pulses.
Risk factors modification
Medication
Endovascular treatment
Surgery
1. Peripheral vascular disease. In: McLatchie G, Borley N, Agarwal A, Jeyarajah S, Harries R, Weerakkody R, et al., editors. Oxford Handbook of Clinical Surgery: Oxford University Press; 2022. p. 0. https://doi.org/10.1093/med/9780198799481.003.0019
2. Marle Jv. Upper Limb Ischaemia. The University of Cape Town General Surgery Textbook for Undergraduates.
https://vula.uct.ac.za/access/content/group/9c29ba04-b1ee-49b9-8c85 9a468b556ce2/Open%20access%20textbook%20of%20general%20surgery/content.html
3. Shah PS, Gates JD. Overview of upper extremity ischemia. UpToDate. 2024. https://www-uptodate-com.ezproxy.newcastle.edu.au/contents/overview-of-upper-extremity-ischemia
4. Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL. Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. The Lancet. 2012;379(9819):905-14. https://doi.org/10.1016/S0140-6736(11)61710-8
5. Mitchell EL. Noninvasive diagnosis of uppper and lower extremity arterial disease. UpToDate. 2024. https://www-uptodate-com.ezproxy.newcastle.edu.au/contents/noninvasive-diagnosis-of-upper-and-lower-extremity-arterial-disease
6. Cheun TJ, Jayakumar L, Sheehan MK, Sideman MJ, Pounds LL, Davies MG. Outcomes of upper extremity interventions for chronic critical ischemia. Journal of Vascular Surgery. 2019;69(1):120-8.e2. https://doi.org/10.1016/j.jvs.2018.04.056
7. Eskandari MK. Upper-Extremity Arterial Occlusive Disease. Medscape. 2024. https://emedicine.medscape.com/article/462289-overview#a2

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion