Critical Limb Ischaemia
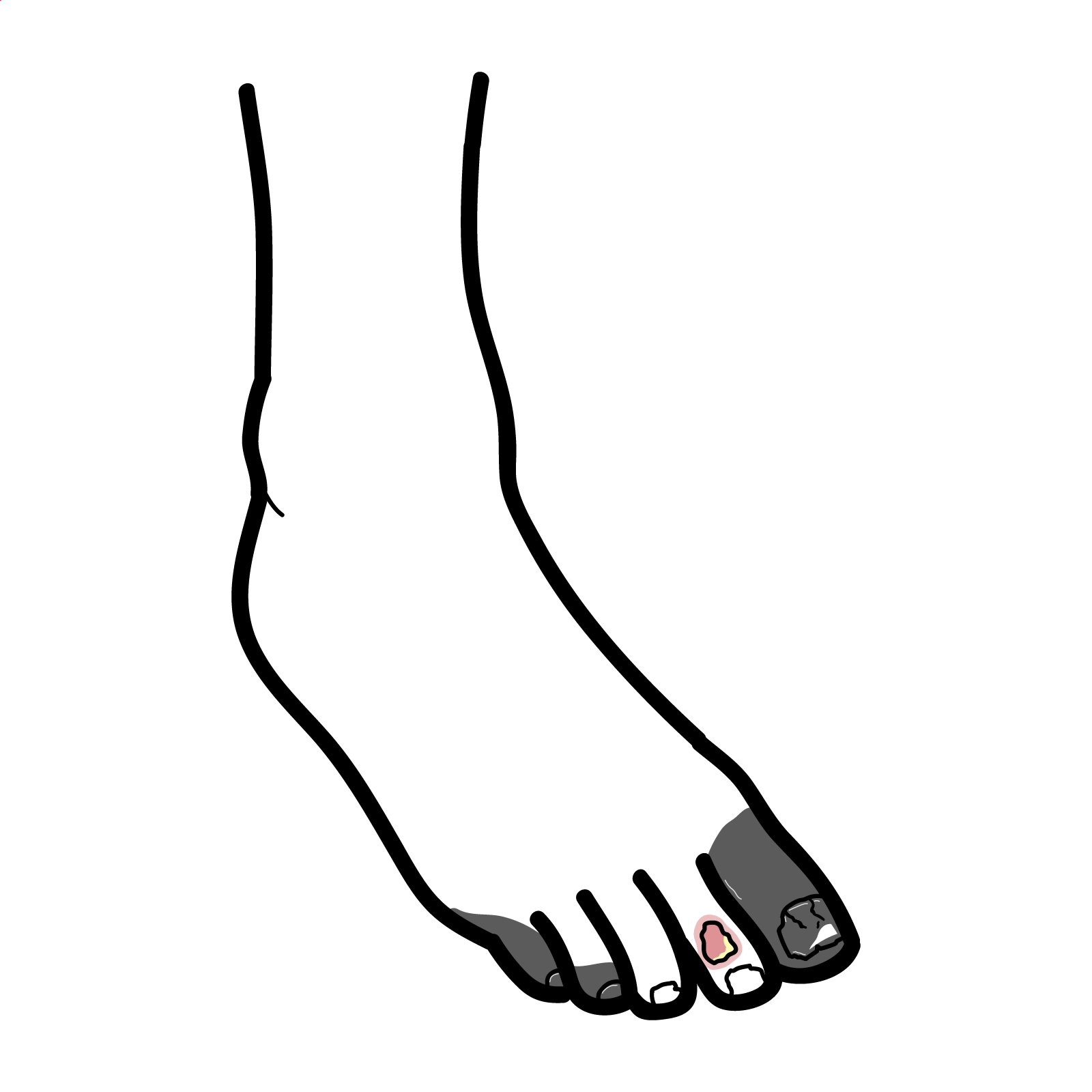
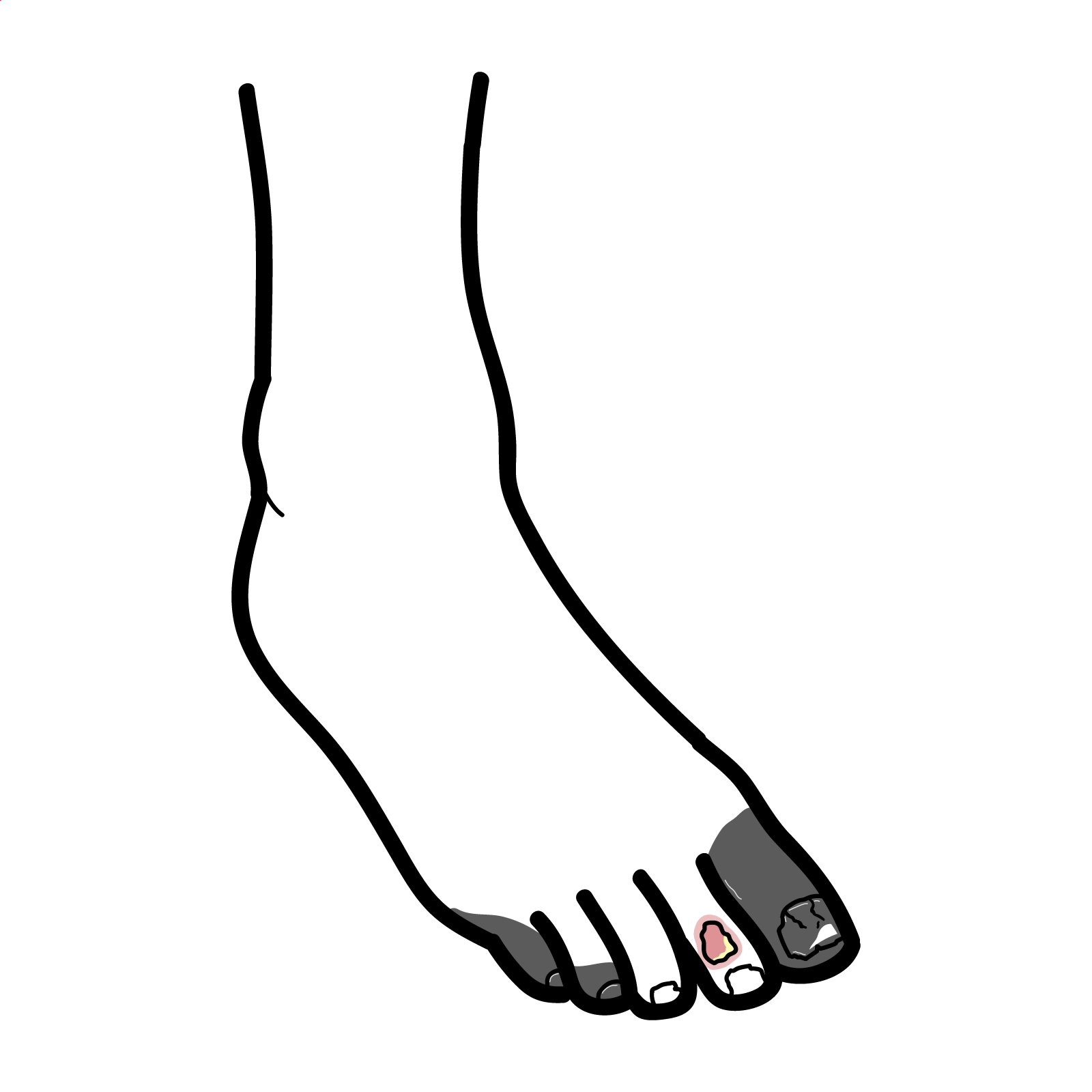
Critical limb ischaemia (CLI) represents grade III and IV chronic limb ischaemia (based on the Fontaine classification). It presents with rest pain, breakdown of skin and inability to heal an injury, which can lead to infection or gangrene. If left untreated it may be necessary to amputate the affected limb. CLI develops in 1% to 3% of patients with peripheral artery disease (PAD).
Critical limb ischaemia is a severe form of chronic lower limb ischaemia, which presents with tissue wounds like ulcers and gangrene, and rest pain lasting more than 2 weeks, which gets worse at night and is relieved by hanging the limb dependent.
Peripheral artery disease (PAD) is a chronic obstruction of arteries supplying the extremities, usually caused by atherosclerosis; it is more common in the lower limb.
Chronic limb ischaemia is a form of PAD characterised by progressive reduction of arterial blood flow to the limbs resulting in cessation of nutrient and oxygen delivery, leading to symptoms such as pain and tissue loss.
Chronic limb ischaemia can be classified using the Fontaine classification:
I – asymptomatic
II – intermittent claudication
III – rest pain
IV – ulcers/gangrene
Grades III and IV are classified as Critical Limb Ischaemia.
Progressive narrowing and occlusion of arteries, mostly due to atherosclerosis, causes reduced blood flow to the extremities. Over time, there is impaired oxygen delivery, even at rest, which leads to tissue hypoxia. The tissue relies on anaerobic respiration, which leads to build up of lactic acid that activities pain receptors causing rest pain. Prolonged hypoxia results in cell death causing symptoms like non-healing ulcers and gangrene.
Occlusion of the aortoiliac segment can cause erectile dysfunction (Leriche syndrome).
Examination
Hanging the limb dependent causes increased blood flow to the limb, due to the forces of gravity, which helps relieve pain.
Pyoderma gangrenosum – skin ulceration that is associated with Inflammatory Bowel Disease; patient will complain of additional symptoms like diarrhea and abdominal pain.
Assess the severity of ischaemia:
Segmental blood pressure – measured at various points along the limb to help localise disease:
Imaging – to precisely identify location and severity of all arterial stenoses involved:
ABPI (Ankle-brachial Pressure Index) is used to assess blood flow in legs. It is calculated by dividing the systolic blood pressure at the ankle by the systolic blood pressure at the arm (brachial artery). ABPI values:
Risk factor modification:
Revascularise the limb via endovascular treatment or surgery:
Angiosome is a 3-dimensional block of tissue fed by specific arterial and venous source. In revascularisation, targeting the artery that supplies the affected angiosome (known as direct revascularisation) results in faster healing and reduced risk of major amputation.
Amputation (if limb is non-viable):
Mortality rate:
Major amputation rate:
1. Peripheral vascular disease. In: McLatchie G, Borley N, Agarwal A, Jeyarajah S, Harries R, Weerakkody R, et al., editors. Oxford Handbook of Clinical Surgery: Oxford University Press; 2022. p. 0. https://doi.org/10.1093/med/9780198799481.003.0019
2. Shishehbor MH, White CJ, Gray BH, Menard MT, Lookstein R, Rosenfield K, et al. Critical Limb Ischemia: An Expert Statement. Journal of the American College of Cardiology. 2016;68(18):2002-15. https://doi.org/10.1016/j.jacc.2016.04.071
3. Armstrong EJ, Armstrong DG. Vascular Disease Patient Information Page: Critical limb ischemia. Vascular Medicine. 2021;26(2):228-31. https://journals.sagepub.com/doi/pdf/10.1177/1358863X20987611?utm
4. Eun JC, Hiatt WR, Glebova NO. Nonatherosclerotic limb ischemia: Prompt evaluation and diagnosis. Cleveland Clinic Journal of Medicine. 2016;83(10):741-51. https://www.ccjm.org/content/ccjom/83/10/741.full.pdf
5. D 2.3 – Differential diagnosis of critical limb ischemia. Journal of Vascular Surgery. 2000;31(1, Supplement 1):S184-S8. https://doi.org/10.1016/S0741-5214(00)81030-7
6. Teraa M, Conte MS, Moll FL, Verhaar MC. Critical Limb Ischemia: Current Trends and Future Directions. Journal of the American Heart Association. 2016;5(2):e002938. https://doi.org/10.1161/JAHA.115.002938

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion