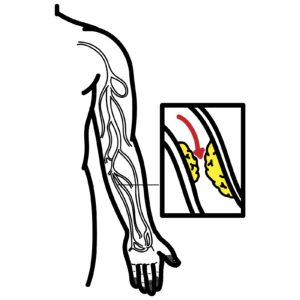
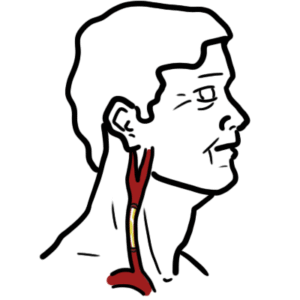
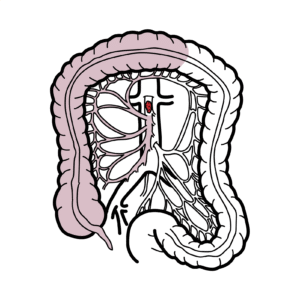
0:00 The crowded arteries are major blood vessels in the neck that supply blood to 0:09 the brain, 0:10 neck, and face. 0:12 We have two crowded arteries, one on the right side of the body and the other 0:16 on the left. 0:22 The right common crowded artery arises from a split or bifurcation of the brach 0:27 iocephalic 0:28 trunk. 0:29 The right subclavian is the other branch, which is a branch of the aortic arch. 0:39 This bifurcation occurs roughly at the level of the right sternoclavicular 0:45 joint, level 0:46 of T2 vertebrae. 0:56 The left common crowded artery branches directly from the arch of the aorta. 1:02 Both the left and right common crowded arteries travel up the neck. 1:11 At roughly the level of the third cartilage, and a cervical vertebrae 4 or C4, 1:18 the crowded 1:19 artery splits into the external and the internal branches. 1:25 This bifurcation happens in an anatomical area called the Crota Triangle. 1:36 Just above the bifurcation of the common crowded artery, there is an area 1:39 called the 1:40 Crota sinus. 1:43 In this area, the common-crotted and internal-crotted are slightly dilated. 1:50 This is an important area, as it contains baroreceptors, which are sensors that 1:55 help 1:55 the body detect and regulate blood pressure. 2:05 At the bifurcation of the common-crotted artery, there is also the carotid body 2:09 , a chemo receptor 2:11 important in maintaining oxygen levels in the blood. 2:20 First off, let's take a look at the external-crotted artery, which supplies 2:25 blood to the areas of the head and neck external to the cranium. 2:31 After arising from the common-crotted artery, it travels up the neck, passes 2:35 behind the 2:36 mandibular neck, and in front of the lobule of the ear. 2:42 The external-crotted artery has a number of branches. 2:45 In ascending order, these are superior thyroid artery, ascending pharyngeal 2:52 artery, lingual 2:54 artery, facial artery, occipital artery, posterior orricular artery, maxillary 3:03 artery, superficial 3:06 temporal artery. 3:13 The internal-crotted arteries, as their name suggests, takes a different path, 3:20 carrying 3:20 blood internally into the cranial cavity. 3:26 They do this via the carotid canal in the petrous part of the temporal bone. 3:32 Unlike the external-crotted artery, the internal-crotted artery do not supply 3:37 any structures 3:38 in the neck. 3:39 Instead, they supply the brain by joining and forming the circle of willis, the 3:52 eyes through 3:52 the ophthalmic artery and the forehead. 3:59 Now that we've given an overview of the anatomy of the carotid arteries, let's 4:04 take a look 4:04 at how these structures are clinically relevant. 4:09 Practical anatomy, carotid pulse. 4:12 The carotid arteries are a commonly used site for assessment of a patient's 4:17 pulse. 4:18 As the heart pushes blood through the arteries, the arteries expand and 4:23 contract with the flow 4:24 of blood. 4:26 Palpation of the carotid arteries in the neck can be used to assess the pulse 4:30 rate, though 4:31 the heart rhythm or character and the strength of the pulse. 4:37 The carotid arterial pulses are best examined with the patient supine and the 4:42 trunk of the 4:43 patient's body slightly elevated and is measured by placing the fingers behind 4:48 the larynx and 4:49 the anterior border of the sternoclonal mastoid muscle. 4:56 It is very important to not palpate both carotid arteries at the same time as 5:00 this reduces 5:01 blood flow to the brain. 5:09 Clinical anatomy, carotid artery hypersensitivity. 5:13 We previously talked about the carotid baroreceptors, which are sensors and 5:19 regulators of blood pressure. 5:22 Baroreceptors are stretch and pressure receptors, so you can imagine if 5:27 external pressure was 5:28 placed on the carotid sinus, the baroreceptors within the carotid sinus would 5:33 think there 5:34 is an increase in blood pressure. 5:38 They would then communicate this with your brain to reduce your heart rate in 5:42 order to 5:42 reduce and restore blood pressure levels. 5:47 Normally, this is only a small amount. 5:52 However, in some people, the carotid sinus overreact to the external pressure, 5:59 making 5:59 their heart slow down or their blood pressure drop a significant amount. 6:06 And this is called carotid sinus hypersensitivity. 6:10 This overreaction can be triggered by wearing tight clothing around the neck or 6:15 even turning 6:15 the head. 6:21 The response is manifested clinically as syncope or presyncope and can lead to 6:28 falls in injury. 6:30 Carotid sinus hypersensitivity is only treated if people are symptomatic. 6:36 If the condition causes the patient's heart rate or heart rate and blood 6:39 pressure to fall 6:40 substantially, they are offered a pacemaker. 6:49 Alcohol anatomy, carotid plaque, atherosclerosis and ischemic stroke. 6:54 The next condition we are going to talk about is atherosclerosis. 6:59 Now, atherosclerosis is deposition of plaques or fatty material on the inner 7:04 wall of the 7:05 arteries. 7:06 When this occurs, blood flow is reduced. 7:11 Atherosclerosis usually occurs at bifurcations, branching regions and regions 7:16 where there is 7:17 high curvature of vessels. 7:22 The example in the bifurcation of the common carotid artery, for example, in 7:26 the bifurcation 7:27 of the common carotid artery into the internal and external carotid arteries. 7:34 The internal carotid artery is the most susceptible to atherosclerosis and can 7:39 result in reduced 7:40 blood flow to the brain, this can result in pre-sincopy or even syncopy. 7:50 Concerningly, if a piece of the plaque ruptures breaks off and migrates up, it 7:57 can occlude 7:59 the cerebral arteries causing an ischemic stroke. 8:05 To assess the severity of the vessel wall thickening in the carotid arteries, a 8:11 doppler study can 8:12 be used to enable estimation of the blood flow through the vessel. 8:19 If the condition is severe, if the plaque is severe enough, the artery can be 8:25 surgically 8:26 cut open and the arthromatous tunica intima that plaque can be removed to 8:32 restore the blood 8:33 flow. 8:36 This procedure is referred to as a carotid and dar terectomy. 8:42 If this is not possible, there is also carotid angioplasty and stenting, which 8:46 can be done. 8:56 Clinical Anatomy, carotid artery aneurysm. 9:01 Darkloresis is a risk factor for a condition called a carotid artery aneurysm, 9:07 which is 9:07 a balloon-like bulge or dilation of the carotid artery. 9:13 As the artery expands, the wall becomes progressively thinner, increasing the 9:18 chance that the aneurysm 9:20 will burst. 9:22 Any segment of the carotid artery can be affected, however the internal carotid 9:26 artery is the 9:27 most commonly involved. 9:32 Carotid artery aneurysms can be associated with certain diseases, including maf 9:37 an syndrome, 9:39 fibromuscular dysplasia, and giant cell arthritis. 9:46 Diagnosis of a carotid artery aneurysm may be made incidentally in patients who 9:51 are asymptomatic 9:52 or suspected due to the clinical manifestations. 9:56 These clinical manifestations include presence of a pulsatile mass in the neck. 10:04 It can be from a mass effect, so the aneurysm may push against nearby nerves. 10:10 For example, in the cavernous sinus, it can push against nerves here, causing o 10:17 phthalmoplasia. 10:19 It can also push against the vagus nerve, causing horse voice. 10:27 It can also push against the internal jugular vein, not a nerve, and when it 10:30 pushes against 10:32 an internal jugular vein, it causes compression and facial swelling from back 10:38 flow. 10:39 Finally, another clinical manifestation is that the aneurysm can rupture and 10:51 bleed. 10:52 Specific tests include a carotid angiography, which will reveal the aneurysm. 10:58 Here is an example. 11:03 Clinical anatomy, carotid artery dissection, a young person stroke. 11:10 This next condition we will be discussing is a carotid artery dissection. 11:15 This is a serious condition involving injury to the innermost wall of the carot 11:22 id artery. 11:24 This test creates two channels of blood flow. 11:27 The first is the normal lumen of the carotid artery, and the other is in the 11:32 wall where 11:33 blood remains stationary. 11:35 The blood that remains in the wall results in narrowing or stenosis or complete 11:42 occlusion 11:43 of the artery, resulting in reduction or elimination of the blood flow. 11:57 In the dissection, bloods can clot and form, and they can also break off from 12:02 the site of 12:03 the dissection. 12:05 They can form an emboli. 12:07 These can travel through the arteries of the brain and block blood supply in 12:12 the brain, 12:13 causing an ischemic stroke. 12:19 Crootid artery dissection is a common cause of stroke in young patients. 12:27 Classic presentation of a Croot artery dissection includes local pain to that 12:32 area, an ipsilateral 12:33 headache to one side or to the neck, an ipsilateral hornet syndrome, ischemic 12:40 stroke and retinal 12:42 ischemia. 12:47 The current gold standard first line investigation is digital subtraction angi 12:52 ography, and this 12:53 is a fluoroscopic technique which enables visualization of the blood vessels. 13:05 The last clinical anatomy we're going to talk about is amorosis fugex, and I'm 13:10 probably 13:10 pronouncing that last part wrong. 13:13 Amorosis fugex from the Greek amorosis, meaning dark and Latin fugax, meaning 13:19 fleeting, is 13:21 a temporary loss of vision in one or both eyes, caused by a blocked blood 13:29 vessel. 13:30 The most common cause of the blocked blood vessel is a cholesterol plaque or 13:35 blood clot, 13:36 and most cases are due to stenosis of the ipsilateral Crootid artery, the Croot 13:42 id artery 13:43 on the same side of the eye symptoms. 13:52 The symptoms of amorosis fugex are partial, or complete loss of vision in one 13:58 or both 14:00 eyes, that is sudden, painless, and temporary. 14:05 The vision loss is often referred to as curtain visual loss, as it appears like 14:10 a vertical 14:10 curtain coming down over the eye before resolving over several minutes. 14:18 Even though this vision loss is temporary, patients experiencing amorous fugex 14:24 are at 14:25 risk of strokes. 14:32 In summary, in this video we talked about the Crootid arteries, which are major 14:37 blood 14:37 vessels that supply blood to the brain, neck, and face. 14:42 We discussed that there are two Crootid arteries, one on each side of the body, 14:47 and the fact 14:48 that in the neck each common Crootid artery branches into two divisions, the 14:53 external 14:54 Crootid artery that supplies blood to the head and neck, external to the cr 14:59 anium, and 15:00 then the internal Crootid artery that supplies blood to the brain, eyes, and 15:04 forehead. 15:05 We also discussed why the Crootid arteries are clinically important and 15:09 relevant, such 15:09 as in the conditions of Crootid artery hypersensitivity, Crootid plaques, Croot 15:16 id artery aneurysm, Crootid 15:18 artery dissections, and amorous fugex. 15:22 Thank you for watching.