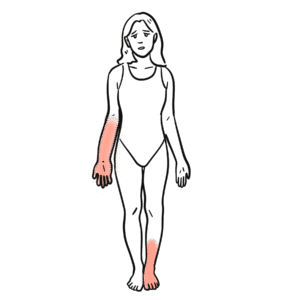
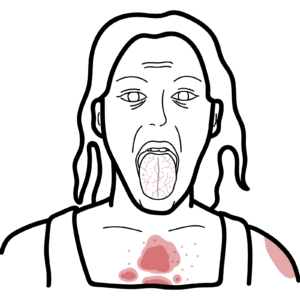
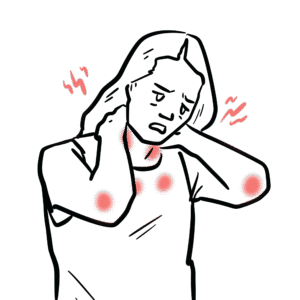
0:00 Hello, in this video, we're going to talk about inflammatory myopathies or my 0:08 ositis. 0:09 These are autoimmune diseases characterized by inflammation of the muscle, 0:15 leading to 0:16 muscle weakness and atrophy. 0:19 The two most commonly recognized types are dermatomyositis and polymyositis. 0:25 These typically present with proximal muscle weakness involving the shoulders 0:31 and hips. 0:32 The difference between the two is that dermatomyositis also have skin changes, 0:38 hence derm as in dermatology, 0:40 the skin. 0:42 Let's recap the function and the anatomy of the muscle. 0:47 Muscle is a specialized tissue found in animals designed to generate force and 0:52 motion. 0:53 If we were to pull the muscle itself, it's composed of different structures. 0:59 But essentially, the muscle tissue is composed of muscle cells called muscle 1:04 fibers, which 1:05 are elongated and designed to contract in response to stimulation. 1:10 These fibers are made up of smaller units called myofibrils, which in turn are 1:16 composed of even 1:17 smaller structures called sarcomeres. 1:20 The sarcomere is the functional unit of the muscle fibers and is responsible 1:24 for muscle 1:25 contraction. 1:29 Here we are looking at normal muscle tissue and we can find blood vessels 1:35 supplying it. 1:37 When you have inflammation of the muscle tissue, this is termed myositis. 1:42 And again, there are many causes of inflamed muscle tissue. 1:47 There could be infective causes, there could be traumatic causes, but we are 1:52 mainly focusing 1:53 on auto-immune causes, which are broadly referred to as inflammatory myopathies 1:59 . 1:59 Now, typically, inflammatory myopathies present with proximal muscle weakness, 2:05 affecting the 2:06 quadriceps and shoulders and biceps. 2:10 Historically, dermatomyositis and polymyositis were the primary types of 2:15 inflammatory myopathies. 2:17 However, six distinct types have now been identified, dermatomyositis, polymy 2:24 ositis, 2:25 anti-syntatase syndrome, overlap myositis, immune-mediated necrotizing myopathy 2:31 and inclusion 2:32 body myositis. 2:35 Each of these have their own unique features. 2:38 Common among these conditions is that you get an elevated creatinine kinase, a 2:43 muscle enzyme 2:44 released into the bloodstream during muscle inflammation. 2:49 But you also get other elevated enzymes, which are your AST and ALT, which are 2:54 typically 2:55 known as your liver enzymes, but these guys can also be found in muscles. 3:02 Other diagnostic tests include an MRI, MRI of the muscle specifically, to help 3:08 detect 3:09 inflammation, which will show as muscle edema. 3:13 The scans from the MRI can be used to help perform a muscle biopsy, which is 3:17 the gold 3:18 standard for diagnosing and also differentiating between the different types. 3:23 The presence of autoantibodies in the blood is another key diagnostic marker 3:28 and helps 3:29 support the diagnosis and differentiate between the different inflammatory my 3:37 ositis. 3:37 Let us now talk about the six different types of inflammatory myopathies. 3:42 Again, each of them present with proximal muscle weakness, typically involving 3:47 the shoulders 3:48 and thighs, however each of them have their own unique features. 3:53 The muscle weakness in itself usually has a history of difficulty getting up 3:56 the chair 3:57 without support and climbing upstairs. 4:02 Again you have the historical classification of polymyositis and dermatomyosit 4:07 is. 4:07 Let's focus on dermatomyositis, which presents with proximal muscle weakness 4:13 with skin changes. 4:14 There are distinct rashes, which include hillyotrope rash, which is purple or 4:18 red rash on the eyelids, 4:20 guttrens papules, red patches over the knuckles, elbows and knees, photos 4:26 ensitive rash, which 4:27 include the shawl sign over the back and V sign over the chest, as well as nail 4:32 changes, 4:32 which include redness, erythema. 4:35 People with dermatomyositis typically have positive antibodies, and there are 4:40 many. 4:41 Most important ones to remember are TIF1 gamma and NXP2, which are dermatomy 4:47 ositis-specific 4:48 antibodies associated with malignancy. 4:53 Polymyositis is the other side of the spectrum, again presenting with proximal, 4:58 symmetrical 4:59 muscle weakness, involving the shoulders, hips, thighs and even neck. 5:03 But importantly, there is no rash. 5:07 Patients are often seronegative, meaning that they don't have any muscle- 5:11 associated antibody. 5:14 Now going to the right side of this image, where the skin rash is, we can 5:18 identify two 5:19 other types of autoimmune inflammatory myopathies, the first being anti-synthet 5:24 ase syndrome, 5:25 which is a unique syndrome in that they present with a number of things. 5:29 Real muscle weakness, they can have inflammatory arthritis, raynodes phenomenon 5:35 , which is discoloration 5:36 of the fingers, especially during cold weather, something called mechanics hand 5:40 , which are 5:40 roughing of the essentially palma aspect of the hand, and interstitial lung 5:48 disease. 5:50 Anti-synthetase syndrome can also have features of dermatomyositis within it. 5:55 There are specific anti-synthetase syndrome antibodies. 5:59 Show one is the most common. 6:03 The other type of inflammatory myopathy that I'm putting on the right side here 6:06 is overlapped 6:07 myositis, because it is also associated with skin changes, such as those seen 6:13 in dermatomyositis. 6:14 But people who have overlapped myositis usually have an underlying autoimmune 6:19 disease, such 6:20 as shroganes, lupus, or scleroderma, with, again, unique antibodies, such as PM 6:28 , SCL, 6:28 rho52, anticu, and U1RMP. 6:35 The next type of inflammatory myositis is immune-mediated necrotizing myopathy, 6:41 which I put on the left 6:42 side here because it is not associated with the rash. 6:46 It again presents with proximal muscle weakness, and hamstring involvement is 6:50 particularly affected. 6:52 It is common in females, and is very much associated with statin use, a lipid 6:58 lowering 6:58 agent, which is an HMG-CoA reductase inhibitor. 7:03 Interestingly enough, patients with immune-mediated necrotizing myopathy may 7:07 have, associated 7:08 with statin use, develop HMG-CoA reductase-OTO antibodies. 7:17 The last type of inflammatory myositis is inclusion body myositis. 7:21 In this group, there is no dermatomyositis, there is no rash, but interestingly 7:26 , people 7:26 have often sudden onset disease, with not only proximal muscle weakness but 7:32 distal muscle 7:33 weakness, particularly in the finger flexors, which is not as common in other 7:38 types. 7:39 Very frequently, inclusion body myositis is associated with dysphagia, 7:43 difficulty swallowing. 7:45 Inclusion body myositis is more common in men, those above 50. 7:51 There is usually normal or slightly elevated creatinine kinase. 7:57 Treatment of all these inflammatory myopathies or myositis include immunosupp 8:01 ression in the 8:02 form of corticosteroids followed by intravenous immunoglobulins or other immun 8:07 osuppressants. 8:08 Interestingly, inclusion body myositis in particular is a type that does not 8:12 respond to immunosuppression. 8:15 Another final important point is that muscles also help with breathing and 8:20 swallowing. 8:21 So in these inflammatory myositis conditions, it can also cause poor 8:26 respiratory effort, 8:28 difficulty breathing and dysphagia, difficulty swallowing. 8:32 So in summary, inflammatory myositis is a group of autoimmune conditions, 8:35 whereby the muscles 8:37 become inflamed. 8:38 This leads to a rise in creatinine kinase and AST and ALT. 8:43 Myositis now can be divided into six phenotypes, dermatomyositis, polymyositis, 8:47 anti-synthetase 8:48 syndrome, overlap myositis, necrotizing autoimmune myopathy and inclusion body 8:54 myositis. 8:54 Thank you for watching.