Overview
Overview Rheumatoid arthritis is a common systemic inflammatory disease characterized by the presence of a destructive polyarthritis with a predisposition for affecting the small joints of the hands and feet and the wrists. Rheumatoid arthritis (RA) is the most common inflammatory arthritis, with a lifetime prevalence of up to 1 percent worldwide. Like many autoimmune diseases, the etiology of RA is multifactorial.
| Definition Arthritis: Inflammaed joint Arthlagia: Pain in a joint Rheumatoid arthritis: Characterized by symmetric polyarticular inflammation of the synovium, typically of the small joints of the hands (MCP and PIP), wrists and feet. This inflammation results in pain and stiffness, and can lead to progressive joint damage resulting in deformities and loss of function. Associated organ damage also contributes to severe disability. Juvenile Rheumatoid arthritis: Heterogeneous group of several disease subtypes that are characterized by the onset of arthritis before the age of 16 years and has symptoms lasting at least 6 weeks. |
Epidemiology
- Female more common 3:1
- Annually 25-30 new cases per 100,000
- Peak age of onset between 20 and 50 years of age
| Remember The main problem is RA is inflammation of the synovium. |
Risk Factors
- Older age
- Family history
- Female sex
- Current or prior smoking
- Early menarche and very irregular period associated with increased risk
| Side note Pregnancy often causes RA remission, likely because of immunologic tolerance. Breastfeeding decrease the risk of RA. |
Signs and Symptoms
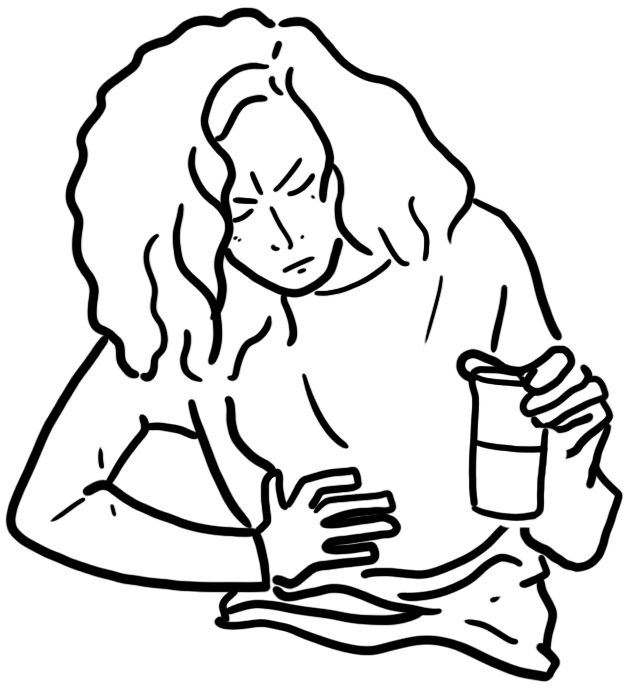
General Patients with RA typically present with pain and stiffness in multiple joints. The wrists, proximal interphalangeal joints, and metacarpophalangeal joints are most commonly involved. Morning stiffness lasting more than one hour suggests an inflammatory etiology.
- Pain
- Morning stiffness
- Myalgia
- Fatigue
- Weight loss
- Joint pain with or without overt swelling or radiological evidence of joint erosions
Examination
- Swelling of three or more joints
- Tenderness largely along the joint line
- Synovitis, producing a “boggy” or “doughy” swelling
- A positive “squeeze test”—pain on gently squeezing the metacarpophalangeal or metatarsophalangeal joints together
| Hand changes as rheumatoid arthritis progresses |
| Remember Consider rheumatoid arthritis in any patient presenting with joint pain, swelling, and morning stiffness of over 30 minutes. |
Extra-articular involvement
- Enlarged lymph nodes
- Splenomegaly
- Lung - pleuritis, nodules and fibrosis
- Heart - Pericarditis, myocarditis, nodules
- Muscle - Atrophy, myositis
- Bone - Osteoporosis
- Skin - Nodules
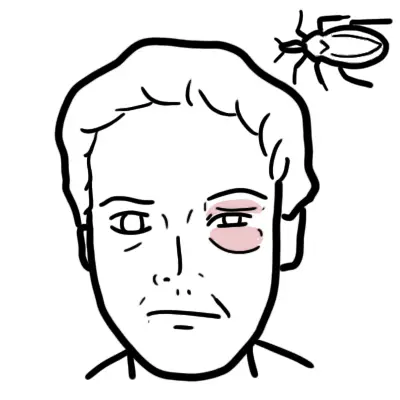
- Eyes - Sicca syndrome, Scleritis
- Nervous system - Nerve entrapment, mononeurititis multiplex
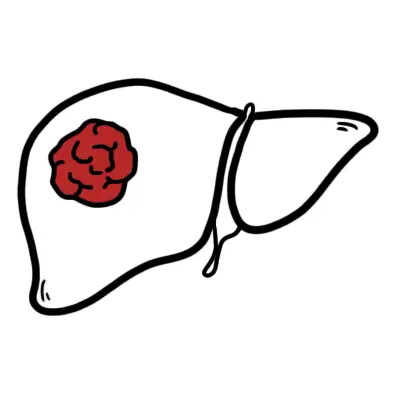
| Caplan's Syndrome Combination of rheumatoid arthritis and pneumoconiosis that manifests as intrapulmonary nodule. |
| Feltys' Syndrome Triad: Rheumatoid arthritis, splenomegaly, neutropaenia. |
Differential Diagnosis
Non-inflammatory Arthritis
Inflammatory Arthritis
- Crystal arthropathy
- Infectious
- Seronegative arthritis
- Ankylosing spondylitis
- Psoriatic arthritis
- Reactive arthritis
- IBD arthritis
- Seropositive arthritis
- Rheumatoid Arthritis
- Scleroderma
- Vasculitis
- Sjogren's
More info on the Differential Diagnosis of Arthritis
| Still's Disease (Systemic-onset juvenile idiopathic arthritis) Triad Persistent high spiking fevers, arthlagia, and a distinctive salmon-colored bumpy rash. |
Investigations
- FBC
- EUC
- LFT
- Antinuclear antibody
- Erythrocyte sedimentation rate
- C- reactive protein
- Rheumatoid factors
- Anti-citrullinated peptide antibodies
- Serum uric acid
- Synvoial fluid tests
- X-ray
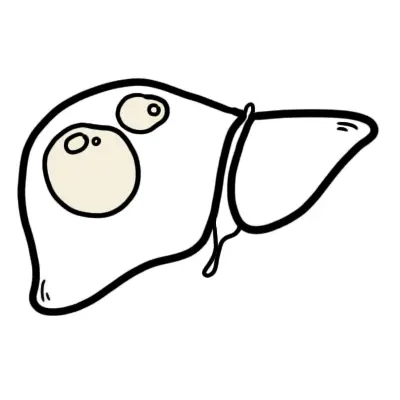
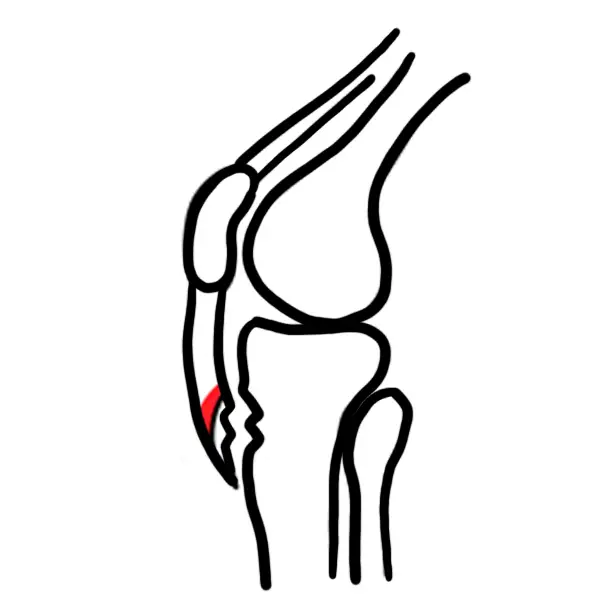
| RADIOLOGICAL CHANGES IN JOINT | |
| Rheumatoid Arthritis | Osteoarthritis |
| Loss of joint space | Loss of joint space |
| Joint deformity | Osteophytes |
| Soft tissue swelling | Subarticular sclerosis |
| Juxtaarticular osteopaenia | Subchondral cysts |
- Ultrasound
- Biopsy
| Other Conditions with positive RF (sero-positive) |
| Sjogrens syndrome (<100%) |
| Felty's syndrome (<100%) |
| Rheumatoid arthritis (~75%) |
| Infection |
| Systemic lupus erythamtosus (<40%) |
| Systemic sclerosis |
| Mixed connective tissue disease |
| Remember Spondylarthropathies tend to have sero negative results (RhF negative). |
| Feltys' Syndrome Triad: Rheumatoid arthrits, splenomegaly, neutropaenia |
Diagnosis - 1987 American College of Rheumatology criteria
- Morning stiffness lasting for at least 1 hour for 6 weeks
- Arthritis of 3 or more joint areas
- Arthritis of hand joints
- Symmetric arthritis
- Rheumatoid nodules
- Serum positive rheumatoid factor
- Radiologic changes - erosions, particularly wrists, hands and feet
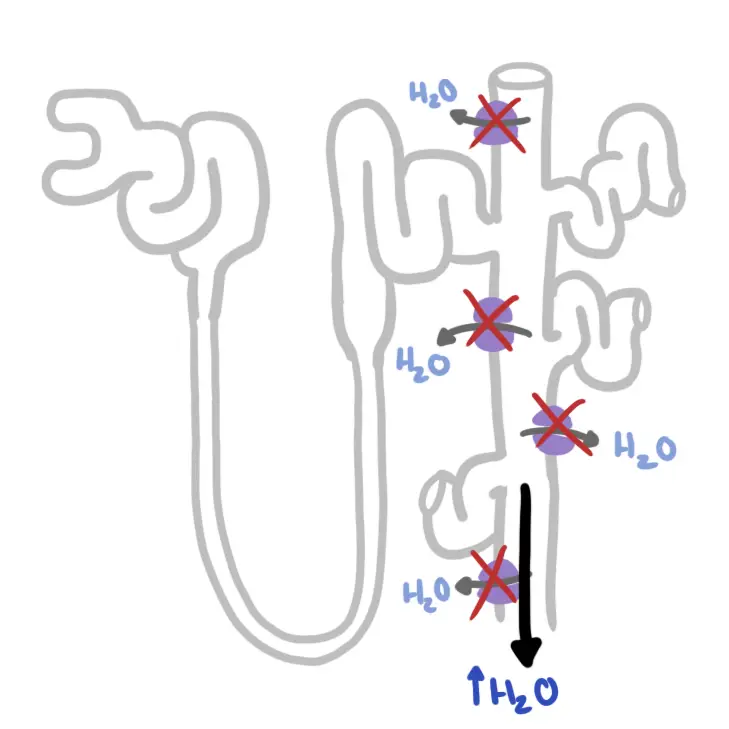
Pathophysiology
| Watch Video: Pathophysiology of Rheumatoid Arthritis |
Management
Principles of managing Rheumatoid arthritis
- Education and counselling
- Physiotherapy
- Occupational therapy
- Podiatry
- Medications
- Alternative treatment
- Surgery
| Remember A guided exercise program can improve quality of life and muscle strength in patients with RA. |
Pharmacological treatment
- NSAIDs
- Paracetamol
- Glucocorticoids
- DMARDs (first-line and recommended early in the disease, combination therapy is advised)
- Methotrexate
- Sulfasalazine
- Hydroxycholoroquine
| Remember Pregnancy do not use Methotrexate! change to hydroxychloroquine! |
- Biological therapies
- Anti-TNFα
- IL-1 receptor antagonist
- IL-6 antagonists
- For disease complications
- Anaemia- iron and erythropoeitin
- Osteoporosis - calcium and Vitamin D supplements, bisphosphanates
- Vasculitis - glucocorticoids, cyclophosphamide
- Amyloidosis - chlorambucil
| Side effects of NSAIDS | |
| Gastrointestinal Tract | Gastric bleeding and perforation (elderly, chronic use) |
| Renal | Fluid retention and papillary necrosis |
| Hypertension | Interference with drugs such as thiazide diuretics |
| Myocardial infarction | |
| Pulmonary | Exacerbation of asthma, pneumonitis (naproxen) |
| Skin | Hypersensitivity, erythema multiforme |
| CNS | Tinnitus, fatigue |
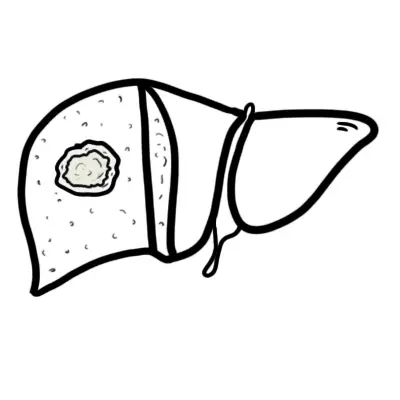
| Hepatic | Drug-induced hepatitis |
| Pharmacology Methotrexate Inhibits dihydrofolate reductase. Methotrexate is given weekly. Side effects: Liver effects, teratogenesis, hair loss, oral ulcers. Toxicity (stomatitis, GI disturbance, and alopecia) may be reduced by the addition of folic acid daily, without loss of therapeutic effect. May cause flare of rheumatoid nodule. NSAID use is contraindicated because there is the potential for interaction and hepatotoxicity. DMARD monitoring is needed to ensure patients do not suffer serious side-effects. |
| Remember Starting treatment with combination disease-modifying antirheumatic drugs (including methotrexate), especially within three months of symptom onset, can slow disease progression and improve symptoms, function, and quality of life. |
| Pharmacology Anti-TNFα biological agent. TNF-α is a potent pro-inflammatory cytokine whose levels are elevated in RA. Anti-TNFa inhibit action of TNF-α and causes immunosuppression. Side effects: Tuberculosis, opportunistic infection. |
Complications and Prognosis
Complications
- Extra-articular manifestation of Rheumatoid arthritis
- Nodules
- Lymphadenopathy
- Vasculitis
- Pulmonary fibrosis
- Pericardial disease (pericarditis, pericardial effusion)
- Raynauds
- Carpal tunnel syndrome
- Peripheral neuropathy
- Splenomegaly
- Atlantoaxial subluxation - Screen X-ray is important prior to surgery (intubation)
| Feltys' Syndrome Triad: Rheumatoid arthrits, splenomegaly, neutropaenia. |
- Depression
- Infection - caused by RA itself or use of immunosupressants
- Malignancy
- Lymphoma
- Lung cancer
- Skin cancer
Prognosis
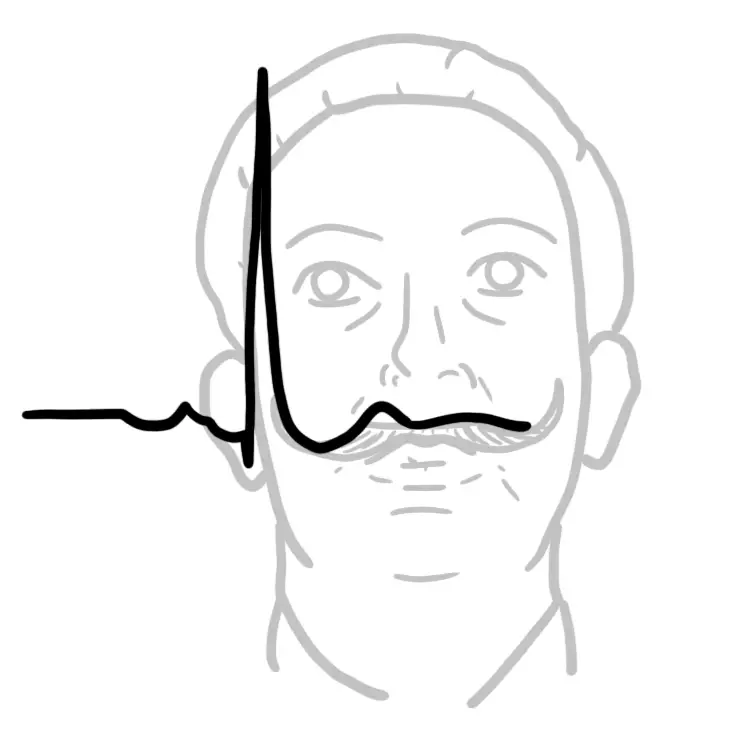
- Patients with RA live three to 12 years less than the general population
- Increased mortality in these patients is mainly due to accelerated cardiovascular disease, especially in those with high disease activity and chronic inflammation.
- 20% will have mild disease
- 75% moderate disease with relapses and remissions
- 5% will have severe destructive disease.
Juvenile Rheumatoid Arthritis
Overview Juvenile idiopathic arthritis is the most common cause of chronic arthritis in childhood. It is characterised by joint inflammation that often leads to joint destruction with physical disability and chronic pain that affects daily life. The disease encompasses all forms of arthritis that begin before the age of 16 years, persist for more than six weeks, and are of unknown cause. The most common risk factors are infections in combination with genetic susceptibility. Many other factors, such as stress and maternal smoking, are thought to contribute to the pathogenesis.
| Remember Differences from adult RA include the problem of growth retardation, a tendency to early fusion of the carpal bones, and erosions at the distal interphalangeal joints. |
Clinical Presentation
- Arthralgia
Differential Diagnosis
- Arthritis
- Infective and reactive: Lyme disease, viral infection, mycoplasma infection, post-streptococcal reactive arthritis
- Juvenile idiopathic arthritis
- Connective tissues disorders: systemic lupus erythematosus, dermatomyositis, systemic sclerosis
- Systemic vasculitis: Henoch-Schönlein purpura, Kawasaki’s disease, polyarteritis nodosa
- Other: haemophilia, immunodeficiency (including periodic fever syndromes), sarcoidosis, inflammatory bowel disease
- Mechanical and degenerative causes
- Trauma: accidental and non-accidental
- Hypermobility
- Avascular necrosis including Perthes’ disease, Osgood-Schlatter’s disease, Scheuermann’s disease
- Slipped upper femoral epiphyses
- Anterior knee pain including chondromalacia patallae
- Non-organic causes
- Idiopathic pain syndromes: diffuse or localised (reflex sympathetic dystrophy)
- Benign nocturnal idiopathic limb pains (growing pains)
- Psychogenic causes
- Miscellaneous causes
- Osteomyelitis
- Tumours: malignant (leukaemia, neuroblastoma) or benign (osteoid osteoma, pigment villonodular synovitis)
- Endocrine and metabolic abnormalities: rickets, diabetes, hypophosphataemic rickets, hypothyroidism or hyperthyroidism
- Genetic disorders: skeletal dysplasias, mucopolysaccharidoses, collagen disorders (Ehlers-Danlos syndrome, Stickler’s syndrome)
Investigations
- Full blood examination
- Erythrocyte sedimentation rate, C reactive protein
- Rheumatoid factor
- Anti-CCP
- HLA B27
- Antinuclear antibodies (ANA)
- Radiography can detect narrowing of the joint spaces or erosions and might show maturation differences or growth abnormalities in bones from an early stage
- Magnetic resonance imaging - inflamed synovium and increased joint fluid
Diagnostic criteria
- Arthritis of one or more joints, defined as swelling
or effusion or two of:- joint warmth
- pain on motion or joint tenderness
- limitation of motion
- Duration of 6 weeks or longer
- Age of onset less than 16 years.
- Absence of other rheumatic disease, mechanical
causes or other identifiable joint disorder.
Management The disease currently has no cure, but clinical remission is a realistic treatment goal
- Non-pharmacological
- Rest
- Ice
- Hydrotherapy
- Physiotherapy - mobility
- Occupational therapist
- Psychologist
- Social worker
- Surgery
- Pharmacological
- NSAIDs
- DMARDs
- Methotrexate
- Biological DMARDs - for severe
- Anti-TNF
- Anti-Tcell (Abatacept)
- Anti-B cell (Rituximab)
Complications (Extra-articular manifestations)
- Intermittent fevers
- Rash - salmon pink macules
- Serositis
- Uveitits - most common
- Growth disturbance
| Remember Ophthalmology review is important in Juvenile Rheumatoid Arthritis. |