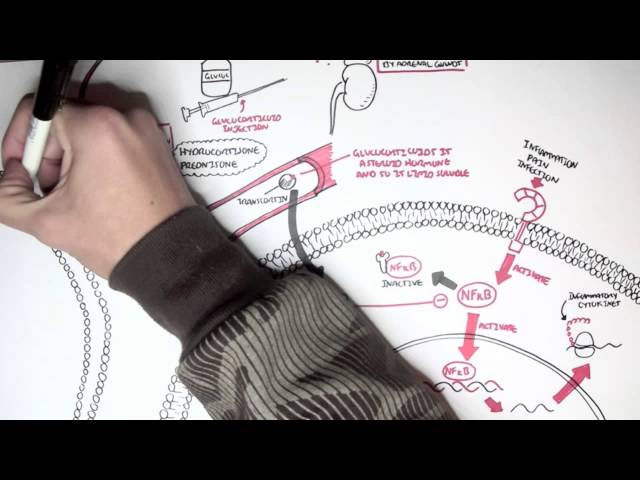
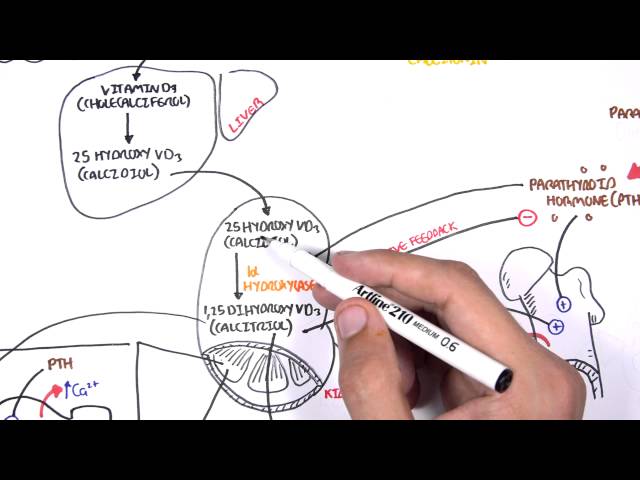
0:00 In this video we're going to talk about osteoporosis management focusing on the 0:09 pharmacology. 0:13 Osteoporosis is where you have low bone mass with microarchitecture disruption 0:18 and skeletal 0:18 fragility. 0:20 This results in a reduced bone strength and an increased risk of fracture. 0:27 This is asymptomatic until a fracture occurs. 0:32 Let's revise the physiology of bone breakdown information. 0:39 Your bone building cells are osteoblasts which respond to parathyroid hormone, 0:44 a hormone 0:44 secreted by the parathyroid glands. 0:50 Root hormone binds to the parathyroid receptors on osteoblasts, the bone 0:56 building cells. 0:57 This causes osteoblasts to express rank ligand, which binds onto the rank on 1:05 premature osteoclasts. 1:08 This interaction activates the premature osteoclasts, which are the bone 1:12 resolving cells, the bone 1:14 breaking cells. 1:16 Osteoclasts excavate characteristic pits and trails on the bone by pumping acid 1:22 to hydroxyapatite 1:24 the mineral component of bone. 1:27 Osteoclasts also release other enzymes that do help degrade or break down bone. 1:34 Osteoclasts formation is regulated primarily by macrophage colony stimulating 1:40 factor, MCSF, 1:43 which promotes the differentiation of myeloid progenitors into promonocytes and 1:49 then osteoclasts. 1:51 It's also regulated by rank ligand that causes the differentiation and fusion 1:55 of premature 1:56 osteoclasts into osteoclasts. 2:02 It's also regulated by a soluble inhibitor, osteoprotegerent, OPG. 2:09 OPG, interestingly, basically binds to rank L, inhibiting the interaction 2:14 between rank 2:15 L and rank, therefore, OPG prevents the activation of osteoclasts. 2:21 Osteoclasts formation is boosted strongly by hypoxia as well. 2:28 An increase in osteoclastic activity means bone breakdown, and this is termed 2:33 bone resorption. 2:35 An increased bone resorption means reduced bone mineral density. 2:40 By the time it gets to a certain stage, the low bone mineral density is termed 2:45 osteoporosis, 2:46 characterized by a T-score less than -2.5. 2:51 A T-score is a term used to describe how dense your bones are, usually measured 2:56 at your spine 2:57 or hip. 2:58 A T-score less than -2.5 is diagnostic of osteoporosis. 3:05 Many things can affect bone physiology and increase the risk of osteoporosis. 3:11 For example, increasing age and female sex, mainly because of postmenopause, 3:17 because estrogen 3:18 actually normally increases OPG expression, so low estrogen as in postmenopause 3:24 causes 3:25 a low OPG. 3:28 Low gonadism, or premature ovarian failure, also contributes. 3:34 Adrenal gland hyperplasia, or long-term glucocorticoids, increases osteoclastic 3:42 activity and so increases 3:43 risk of osteoporosis. 3:47 A low body mass index, immobilization, space travel, basically being weightless 3:53 , reduces 3:54 osteoblastic activity. 3:58 Other risks include when you have a certain ethnic background. 4:01 For example, white persons are at a higher risk than black persons. 4:05 Rheumatoid arthritis and bone cancer increases inflammatory states around bone, 4:10 which stimulates 4:11 osteoclastic activity and so increases the risk of fractures. 4:16 There's also smoking, alcohol abuse, vitamin D deficiency, as well as low 4:23 calcium intake. 4:29 So, the prevention of osteoporosis is quite straightforward. 4:33 Stop smoking, lower alcohol intake, make sure to have enough calcium and 4:40 vitamin D, and 4:41 there's also weight-bearing exercises, which are recommended for most women 4:47 with pre-menopausal 4:48 osteoporosis. 4:50 Interestingly, there's no convincing evidence that high-intensity exercise, 4:50 such as running, 4:56 is of greater benefit than lower intensity exercise, such as walking. 5:03 Now there are medications available to prevent and to treat osteoporosis. 5:09 Medications to prevent osteoporosis are only for those at high risk of osteopor 5:15 osis. 5:15 This includes those taking high-dose steroids for a long duration. 5:21 If someone has a fragility fracture, then usually they are started on 5:24 medications for 5:25 osteoporosis, even if they haven't met the diagnosis based on the T-score, or 5:32 if they 5:32 are diagnosed with osteoporosis with a T-score less than -2.5. 5:37 Let's take a look at the classes of medication used for managing osteoporosis. 5:47 Dysphosphonates are one of the most important ones, and they are anti-resor 5:52 ptive agents. 5:53 Dysphosphonates work by binding to hydroxyapatide binding sites on the surface 5:59 of bone tissue. 6:00 Dysphosphonates components are then taken up by osteoclasts during the phases 6:04 of bone 6:04 resorption, and when this happens it actually interferes with osteoclasts 6:10 function and promotes 6:11 osteoclasts apoptosis, which causes them to die and so you have reduced bone 6:22 resorption. 6:24 Dysphosphonates are the first line treatment for osteoporosis in postmenopausal 6:28 women and 6:28 men over the age of 50. 6:31 In glucocorticoid induced osteoporosis with moderate to higher fracture risk, 6:34 oral bisphosphonates 6:35 are recommended as first line therapy, regardless of age. 6:41 The side effects of bisphosphonates include osteonichrosis of the jaw, which 6:44 can happen 6:45 at any time. 6:46 There's also atypical femoral fractures, which is associated with longer 6:51 duration of use. 6:54 Other side effects include hypocalcemia and hypophosphatemia, musculoskeletal 7:00 pain, atrial 7:01 fibrillation, renal impairment. 7:10 Oral bisphosphonates specifically can cause esophageal inflammation, as well as 7:15 ocular 7:15 inflammation and visual disturbances. 7:21 Contraindications to use bisphosphonates include that of a poor renal function 7:27 with an EGFR 7:28 less than 30 to 35. 7:32 Hypocalcemia, if you have an esophageal abnormality, such as a stricture, there 7:36 is also some relative 7:38 contraindication during the use in pregnancy, as well as lactation period. 7:45 Bisposphonates come in two forms. 7:47 There's oral bisphosphonates, such as alendronate, resendronate. 7:51 And then there's also the IV bisphosphonates, such as zolodronic acid. 7:57 IV bisphosphonates are usually used for those who have malignancy and who have 8:02 esophageal 8:03 abnormalities. 8:04 IV bisphosphonates specifically can cause flu-like symptoms, usually within 24 8:10 to 72 hours after 8:11 administration. 8:14 Bisposphonates should be taken in the morning and evening, at least 30 minutes 8:18 before meals 8:18 to prevent bisphosphonates from forming complexes with calcium. 8:23 This is to prevent esophageitis. 8:25 They should also be taken with plenty of water and an upright position should 8:30 be maintained, 8:31 for at least 30 minutes following the intake. 8:35 Interestingly, a drug holiday period, which is basically being off bisphosphon 8:39 ates, can 8:40 be considered if you've been taking bisphosphonates intravenously for three 8:45 years or five years 8:46 if you're taking oral bisphosphonates. 8:54 Zoloxophine is a selective estrogen receptor modulator, a serum. 9:02 Zoloxophine inhibits bone resorption and reduces the risk of vertebral 9:06 fractures, as well as 9:07 increases bone density. 9:12 It's quite common in postmenopausal women who have osteoporosis, as it also 9:17 reduces the 9:18 risk of breast cancer. 9:19 If someone has a risk of breast cancer, you would consider using this. 9:28 It's contraindicated in pre-metaposal women. 9:31 In pre-metaposal women, reloxophine would block estrogen action on bone and 9:36 would actually 9:37 cause a decrease in bone density and so increases the risk of osteoporosis. 9:42 Another contraindication of reloxophine is veno-thromboembolism, because the 9:46 side effects 9:47 of reloxophine is that it inhibits the estrogen action and so you get men 9:52 opausal symptoms, 9:54 hot flushes, leg cramps, and peripheral edema, as well as an increase in throm 10:00 boembolic events. 10:05 Another class of medications used to manage osteoporosis is those that inhibit 10:12 rank ligand. 10:13 The neusabab is a fully human monoclonal antibody that specifically binds to 10:18 rank ligand and 10:19 blocks the binding of rank ligand to rank, specifically binds to rank ligand 10:27 and blocks 10:27 the binding of rank ligand to rank, and thereby reduces the formation, the 10:32 function, and the 10:33 survival of osteoclasts, which results in a decrease in bone resorption and an 10:38 increase 10:39 in bone density. 10:41 The side effects of denusabab include hypocalcemia, back pain, pain in the 10:48 extremity, hypocolesterolemia, 10:50 musculoskeletal pain, as well as cystitis. 10:55 There is an increased rate of cellulitis and bronchitis. 11:01 Medication-related osteoporosis of the jaw and atypical femoral fracture have 11:05 been reported 11:06 with denusumab use as well. 11:10 Denusumab is administered twice yearly and it's a good alternative to bisphosph 11:15 onates, 11:16 especially if someone has renal failure. 11:19 That is why you see all dialysis patients or those with renal failure on denus 11:26 umab. 11:27 Interestingly, if denusumab is discontinued, you have to administer an 11:31 alternative therapy. 11:33 Typically, bisphosphonate, and this is to prevent for a rapid bone loss because 11:37 there's 11:37 an increased risk of vertebral fractures if you stop denusumab. 11:46 Another class of medications used to treat osteoporosis is parathyroid hormone 11:50 and parathyroid hormone-related protein 11:52 analogs, which belong to actually completely different class of osteoporosis 11:57 medications 11:58 called anabolic agents because they actually really increase bone formation. 12:07 Parathyroid hormone normally stimulates osteoblasts and so stimulates bone 12:12 formation, but also 12:13 osteoclasts, which causes bone resorption. 12:16 So it seems odd to use parathyroid hormone analogs or related peptides. 12:23 However, intermittent administration of parathyroid hormone has been shown to 12:29 stimulate bone formation 12:32 more than bone resorption. 12:35 Your parathyroid is a parathyroid hormone analog. 12:39 A belloparathyroid is a parathyroid hormone-related protein analog. 12:44 Both agents stimulate bone formation and require daily subcutaneous injection. 12:50 Treatment should be limited to two years. 12:57 The side effects of the parathyroid hormone analogs include hypercalcemia and 13:04 hypercalceuria. 13:05 And so you get increased risk of renal stones. 13:08 You also get an increased serum uric acid, which means that there's an 13:12 increased risk 13:13 of gout. 13:16 Another side effect is you're injecting yourself daily with this agent, which 13:20 could be quite 13:21 annoying. 13:23 And because the treatment of these agents are limited to two years, it's 13:27 important to transition 13:29 to an anti-resorptive agent to prevent the loss of the newly formed bone. 13:40 Another class used to treat osteoporosis are the sclerostin inhibitors. 13:45 There is a peptide called sclerostin. 13:48 In the skeletal tissue, sclerostin is a protein secreted by osteoclasts to 13:54 reduce bone formation 13:55 by interfering with the proliferation and function of osteoblasts. 14:01 Romo-sosumab is a humanized monoclonal antibody that inhibits sclerostin. 14:06 And so by inhibiting sclerostin, you're allowing the osteoblasts to build more 14:11 bone. 14:11 And so increase bone density. 14:16 So in summary, osteoporosis is where you have a low bone mineral density, 14:21 characterized 14:22 by a T score less than negative 2.5. 14:26 It's important to address the risk factors and to encourage stopping smoking, 14:32 stopping 14:33 alcohol intake, and some exercises, especially if you're in the pre-menopausal 14:39 state. 14:40 The drug classes used for osteoporosis include bisphosphonates, the rank ligand 14:46 inhibitors, 14:47 as well as the parathorin hormone analogs and the sclerostin inhibitors.