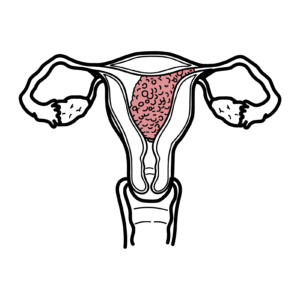
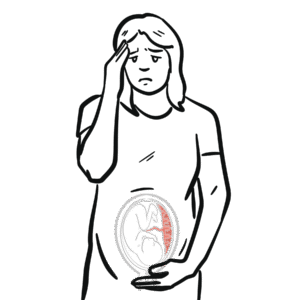
0:00 Hello, in this video we're going to talk about gestational diabetes myelitis, 0:09 or GDM 0:09 for short. 0:12 Gestational diabetes is a common condition that occurs during pregnancy, 0:17 specifically 0:18 diagnosed roughly in the third trimester of pregnancy. 0:23 As the name suggests, it essentially is similar to diabetes myelitis type 2, in 0:30 that you 0:30 have hyperglycemia and you have problems with insulin. 0:36 So let's look at what normally happens during pregnancy. 0:40 The pancreas is an organ responsible for producing the hormone insulin. 0:46 And here is the target cell, which insulin will target, eventually. 0:53 And here is the fetus, which is inside the uterus of the pregnant lady. 0:59 During pregnancy, there is beta cell hyperplasia. 1:04 Beta cells or B cells are cells in the pancreas that produces and secretes the 1:09 hormone insulin. 1:13 When a pregnant lady eats their blood glucose rises, there is hyperglycemia. 1:20 Hyperglycemia will stimulate the beta cells of the pancreas to release the 1:24 hormone insulin 1:25 into circulation. 1:28 The increase in insulin in the circulation will go around the body and then 1:32 target specific 1:33 cells, telling these cells to take up glucose from the blood, in the attempts 1:39 to reduce 1:40 blood glucose. 1:43 There is still enough blood glucose available in circulation to enter fetal 1:49 circulation. 1:50 The fetus requires glucose in order to gain energy and to grow. 1:56 And so the fetus will receive adequate glucose and so there will be normal 2:02 fetal growth. 2:03 The fetus will always receive glucose because of several reasons. 2:09 The first is that during pregnancy, insulin sensitivity decreases. 2:17 This means that the effects of insulin on maternal tissue is reduced. 2:24 Because the effects of insulin is reduced, there will be more glucose in the 2:30 blood. 2:31 Beta cell hyperplasia in the maternal pancreas occurs because of reduced 2:38 insulin sensitivity 2:40 in maternal tissue. 2:42 And this also is a cause of the factors released by the fetus, telling the 2:47 maternal body to feed 2:49 it. 2:51 What happens in gestational diabetes is that instead of a small decrease in 2:55 insulin sensitivity 2:57 in maternal tissue, there is a lot of insulin sensitivity decreasing and thus 3:03 also insulin 3:04 resistance. 3:07 Here is the pancreas of the mother with gestational diabetes. 3:12 And here is the target cell of insulin. 3:15 And here is the fetus in uterus. 3:18 After a mother eats, blood glucose increases. 3:21 There is hyperglycemia. 3:25 But glycemia stimulates the fetus cells of the pancreas to release the hormone 3:30 insulin 3:30 into circulation. 3:33 Insulin aims to target cells to increase glucose uptake in maternal tissue. 3:40 But in gestational diabetes, there is insulin resistance and therefore blood 3:45 glucose is not 3:46 taken up into maternal tissue as efficiently. 3:51 The result of insulin resistance is hyperglycemia of the maternal circulation. 3:57 With hyperglycemia, this also travels into fetal circulation. 4:02 And so there is an increase in blood glucose in the fetus. 4:09 Because of hyperglycemia in fetal circulation, the fetus, the fetal pancreas 4:16 thus will work 4:17 by producing its own insulin. 4:21 With more fetal insulin, the fetal tissue will take up more glucose that is 4:27 available. 4:28 And so there will be more growth of the fetus. 4:32 The growth of the fetus increases and you get a big baby. 4:37 Similarly, the increase in blood glucose in maternal circulation means that the 4:42 mother 4:42 can have symptoms of diabetes, which are the four P's, polyuria, polyphagea, 4:49 parastasia, 4:50 which is not actually common, but it's more so in chronic diabetes, and polyb 4:57 ipsia. 4:57 These symptoms are not very specific for gestational diabetes. 5:02 Instead gestational diabetes is rather asymptomatic. 5:06 The reason for a big decrease in insulin sensitivity and the development of 5:11 insulin 5:11 resistance in gestational diabetes is thought to be because of the placenta 5:18 producing hormones 5:19 such as growth hormones, CRH and placenta lactogen. 5:24 Placenta hormones cause a decrease in insulin sensitivity to try to tell the 5:30 mother to feed 5:31 it with more glucose. 5:37 Risk factors for gestational diabetes, myelitis, include a pregnant lady's age 5:44 greater than 5:45 35 years old, obesity, family history of GDM, polycystic ovarian syndrome, 5:54 certain ethnic 5:55 groups, including Southeast Asians, and also having a previous history of GDM. 6:03 The diagnosis of gestational diabetes is actually done during screening at 24 6:10 to 28 weeks, roughly, 6:11 gestation, and this is done with a fasting blood glucose or with the oral 6:15 glucose tolerance 6:16 test. 6:19 A fasting blood glucose is measured between weeks 24 to 28 weeks. 6:24 A fasting blood glucose of greater than 5.1 millimoles per liter can help 6:30 diagnose GDM. 6:33 The diagnosis of GDM can also be done with an oral glucose tolerance test. 6:40 If blood glucose is greater than 10 millimoles per liter after one hour of 6:46 taking oral glucose 6:48 or greater than 8.5 millimoles per liter after two hours of taking oral glucose 6:54 , these values 6:55 normally should be lower because insulin should be lowering blood glucose, but 7:02 with insulin 7:03 resistance or sensitivity, blood glucose takes a lot longer to go down after 7:08 eating glucose. 7:12 On a side note, diagnosing diabetes is different, what I mean is diagnosing 7:17 diabetes type 2 7:18 in non-pregnant women. 7:21 You can think of diagnosing diabetes type 2 as the 7-eleven rule, 7-eleven rule 7:29 meaning 7:29 a fasting glucose greater than 7 millimoles per liter or a random blood glucose 7:35 greater 7:36 than 11 millimoles per liter with symptoms of diabetes can help with the 7:41 diagnosis of 7:42 Alzheimer's diabetes type 2. 7:46 The complications of gestational diabetes can be divided into maternal 7:51 complications, 7:52 fetal complications, and infant complications. 7:58 Maternal complications or mother complications of gestational diabetes include 8:03 hypertensive 8:04 disorders, increased risk of infection, cesarean section, is a 50% risk of 8:12 developing future 8:13 diabetes type 2, a maternal complication can also be a treatment complication 8:21 where you 8:22 get insulin-related hypoglycemia. 8:30 Fetal complications occurs as a consequence of fetal hyperglycemia. 8:35 With fetal hyperglycemia you get fetal hyperinsulinemia. 8:41 Fetal hyperinsulinemia means that there will be more glucose uptake by fetal 8:47 tissues causing 8:48 macrosomeia or a big A/B. Fetal hyperglycemia means fetal osmotic diuresis 8:59 occurs which 8:59 means that the fetus will pee more because of the diuretic effects of glucose. 9:07 Because the fetus peeves more, more fluid will be within the amniotic sac 9:11 causing polyhydromnios. 9:16 Fetal hyperglycemia may lead to congenital abnormalities and even stillbirth. 9:24 Infant complications or baby complications tend to occur during delivery or 9:29 right after 9:30 delivery. 9:31 And this is because the fetus is larger than normal, there is macrosomeia, and 9:36 thus birth 9:37 trauma can occur, and this can be trauma to the baby or to the mother's genital 9:44 tract. 9:44 After delivery the fetus will not receive any more glucose from the mother 9:48 because the 9:49 umbilical cord is clamped. 9:52 Keep in mind that there is still fetal hyperinsulinemia present, and this means 9:57 that glucose will 9:58 be taken up still. 10:01 But with no more supply of glucose in the baby, this means that there is hyp 10:07 oglycemia. 10:09 Later, after delivery, the baby will also have subsequent hyperbilirubinemia, 10:18 hypotalcemia, 10:19 and increased risk of respiratory distress syndrome, which is a respiratory 10:24 problem which 10:25 is manageable. 10:29 There is also a long-term risk of the baby developing childhood obesity. 10:36 The management of gestational diabetes can be divided into managing the 10:41 pregnancy itself 10:41 and managing the baby after delivery. 10:46 The maternal management or pregnancy management involves a multidisciplinary 10:51 team where the 10:52 obstetrician plays a vital role as a woman with gestational diabetes is a high- 10:58 risk patient. 11:00 The management first line is diet and exercise. 11:06 Use of diabetic medications, including metformin, can also be used. 11:11 If this fails, or if the mother prefers, insulin injections can be used. 11:18 During this period of managing gestational diabetes, which again is diagnosed 11:24 roughly 11:24 between 24 to 28 weeks, which is a screening process, the pregnant woman needs 11:31 to continuously 11:32 monitor their blood glucose with a finger-prick test, for example, at least 11:36 four times a day. 11:37 Further, it is important to monitor the fetus inside the uterus using an 11:42 ultrasound to detect 11:44 any anatomical changes, to check for fetal size, to check for fetal blood flow, 11:51 and also 11:51 checking the fetal heart rate. 11:55 The management of the baby occurs postpartum after delivery and includes oxygen 12:01 ation because 12:01 of the risk of respiratory distress syndrome. 12:05 Because the baby is also in hypoglycemia, there can be also administration of 12:12 extras. 12:13 It is finally also important to monitor the bilirubin levels, the glucose 12:18 levels continuously, 12:19 and also the calcium levels.