
| Watch Pregnancy - Overview |
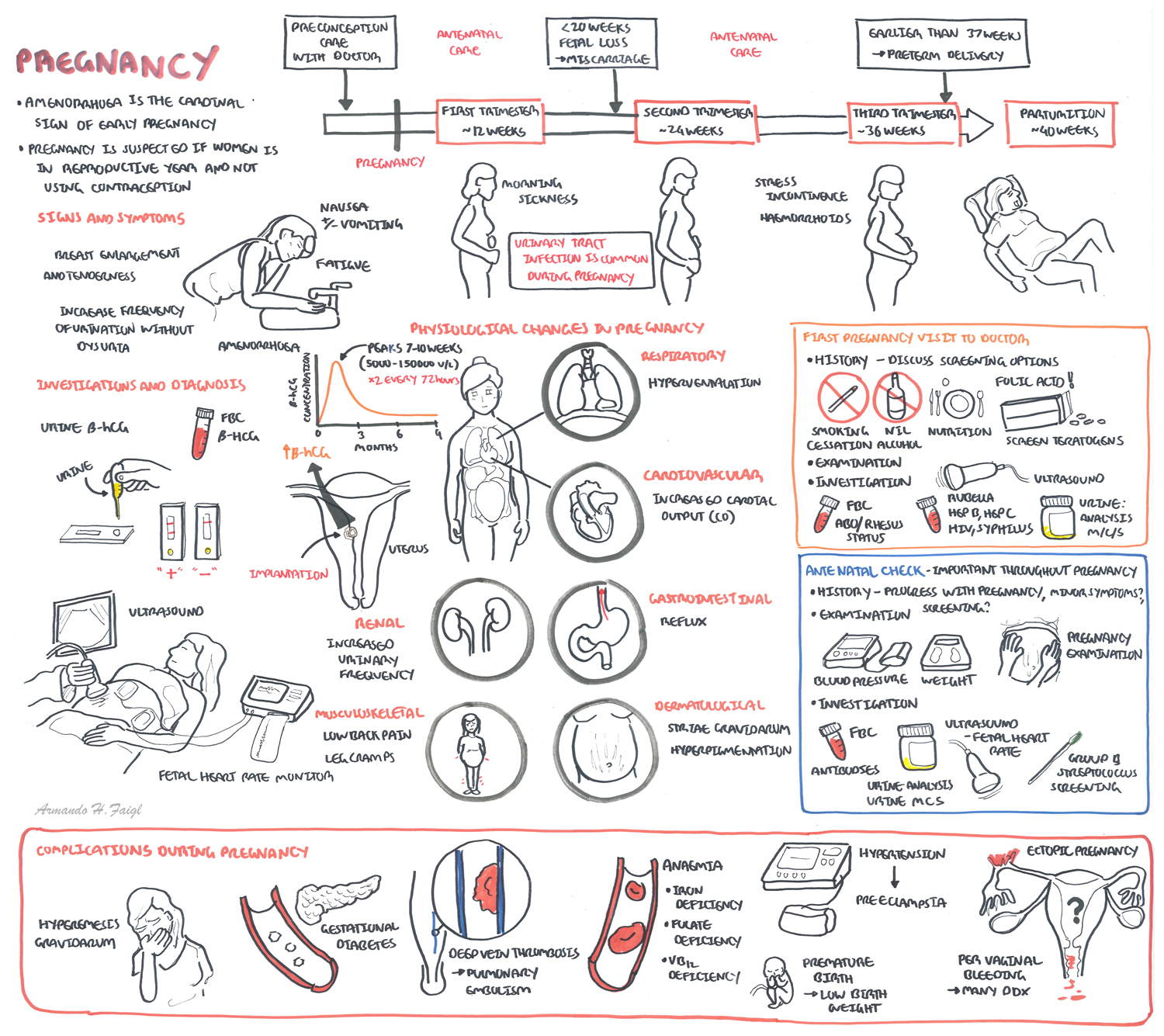
Uterus, Vagina and Breast Physiology changes
Uterus (Cervix + Isthmus + Body of uterus)
Vagina
Breast
Endocrine Physiology changes
Pituitary Gland
Thyroid hormones
| Remember that iodine, antithyroid drugs or antibodies associated with thyroid disease can cross the placenta and affect the fetal thyroid function |
Endocrine changes
Progesterone
Oestrogen
Human placentala lactogen
Haemtological Physiology Changes
Respiratory Physiology Changes
Cardiovascular Physiology Changes
Urinary Physiology Changes
Digestive Physiology changes
| Watch Video Physiological Changes during Pregnancy |
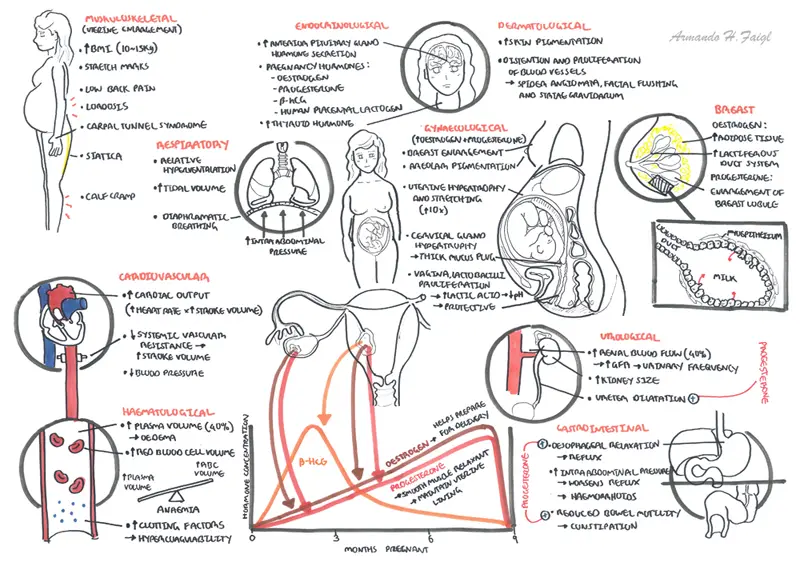
Early Pregnancy
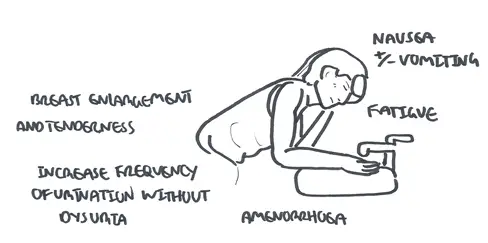
Late Pregnancy
Hormonal changes
Uterine Enlargement
Other
| Remember Urinary infections are common in pregnancy. Screen for UTIs! |
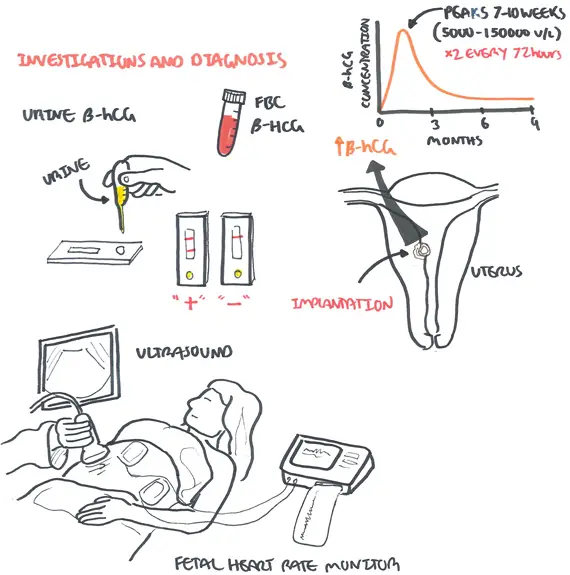
Any of the following:
Supported by:
| Side note ß-hCG is produced by synctiotrophoblast (outside of blastocyst that invades into uterine wall – implantation). ß-hCG prevents degeneration of the corpus luteum (and therefore can continue producing progesterone until placental progesterone can take over at about 6 weeks). B-hcG concentration doubles every 48 hours during first 30-40 days after implantation of a viable, intrauterine pregnancy. After which it slowly rises approximately to 10 weeks then declines until reaching a plateau in 2 nd and 3 rd trimester. |
| Remember Causes of slow rise in B-hCG: ectopic pregnancy, miscarriage (not possible to detect off single level - must do multiple tests) |
| Remember Causes of fall in B-hCG: can be physiological if at 10 weeks but mainly consistent with resolving ectopic, miscarriage |
Antenatal check refers to the health care provided to a pregnancy woman throughout pregnancy until labour. Basically a screening program intended to detect complications early, provide health education and implement effective health promotive and preventative interventions.
TIMING (4:2:1)
Normal, uncomplicated pregnancy
| Remember Role of ultrasounds: 1st trimester - Determining viable pregnancy versus miscarriage, incomplete miscarriage, molar pregnancy and ectopic pregnancy, Dating scan, Screening (Nuchal fold thickness) and fetal anatomy. 2nd trimester - Fetal anatomy, Fetal measurements, Placental location, Sex of baby (if parents want to know) |
| Indications for Ultrasound during pregnancy |
| Routine antenatal check |
| Antepartum Haemorrhage |
| Fundal height is small or large for dates |
| Medical complications of pregnancy – diabetes, Preeclampsia |
| Abnormal foetal presentation |
| Unstable lie at term |
| Placental location if previous scans show LLP |
Introduction: Confirmation of pregnancy and discussion of models of care
| Naegele's rule (Nagel's rule) predicts an estimated due date based on the woman's last menstrual period. |
| Remember Smoking is associated with premature birth, placental abruption, miscarriage, low birth weight, still birth, placenta previa |
| Remember With Alcohol there is no safe level during pregnancy however 2 standard drinks per day not associated with any adverse pregnancy outcomes. High levels associated with Fetal Alcohol Syndrome |
Examination
| Remember risk of UTI increases during pregnancy |
Investigations
More info Medical Complication During Pregnancy
Contraception
