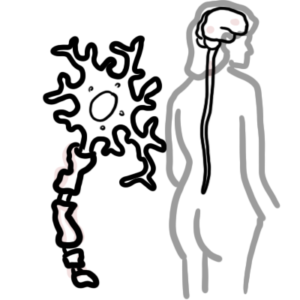
0:00 Hello, in this video we're going to talk about kidney stones. 0:10 Kidney stones or urinary stones have many names, including urolytheasis, which 0:15 is actually 0:16 formation of stones along the urinary tract, or nephrolithiasis, which is 0:22 stones forming 0:23 specifically in the nephron or the kidneys. 0:27 To make things even more confusing, urinary or kidney stones can also be called 0:33 renal 0:33 or urinary calcula. 0:37 Calcula essentially means stones, however these words are used interchangeably 0:43 but essentially 0:43 mean the same thing, kidney stones. 0:48 In order to understand kidney stones, we have to revise the anatomy. 0:54 Here the adrenal glands, which are endocrine glands, sit above the kidneys. 1:00 The kidneys form urine, urine will then travel down the ureter and be stored in 1:08 the bladder. 1:10 The bladder can stretch and once full, we urinate, the urine will flow through 1:17 the urethra 1:19 and then out. 1:22 The ureter has three sites of constriction, where it contracts the smooth 1:28 muscle and these 1:29 are important to know because these are the sites where narrowing can occur and 1:35 also the 1:35 site where urinary stones can lodge. 1:39 The sites of ureteric constriction include the pelvic ureteric junction, the 1:46 pelvic brim 1:49 and the vesicule ureteric junction. 1:53 The vesicule ureteric junction is actually the connection between the ureter 1:58 and the urinary 1:59 bladder which is sort of behind and under the urinary bladder. 2:07 The kidneys are organ responsible for filtering the blood and disposing of 2:12 waste, it's important 2:13 for regulating blood pressure and regulating electrolyte balance. 2:20 It is also responsible for producing some important hormones such as erythropo 2:25 ietin and 2:26 activation of vitamin D. 2:30 Here is the adrenal glands, which are again the endocrine glands that sit above 2:35 our kidneys. 2:38 Here is the ureter. 2:41 Looking inside the kidney, it consists of pyramids called the medulla pyramids. 2:48 Surrounding the medulla pyramids is the cortex. 2:52 The medulla pyramids joins, the tip of the medulla pyramids joins and forms the 2:59 calyx. 3:00 The calyx then join together and form and drain into the renal pelvis. 3:07 The renal pelvis has a renal artery and renal vein entering and exiting it. 3:14 Reciting around and within the medulla pyramids are the functional units of the 3:20 kidneys called 3:21 nephrons. 3:24 Nephrons are structures which filter our blood. 3:28 They secrete waste and allow reabsorption of things into the bloodstream. 3:35 Thus, it has a main role in regulating electrolyte and fluid balance in our 3:43 body. 3:44 The head of nephron is the bowman's capsule, where the afferent arterial brings 3:50 blood in, 3:51 forming the glomerulus, and then we have the efferent arterial leaving the gl 3:59 omerulus. 4:01 Once filtering has occurred within the bowman's capsule, the filtrate will 4:07 travel along the 4:09 tubule of the nephron. 4:11 Firstly, it will pass the proximal convoluted tubules, then it will go down 4:17 towards the 4:17 loop of Henley, the distal convoluted tubules, and then finally the collecting 4:25 duct. 4:26 Looking more closely at the tubule, the cells that line the nephron tubules are 4:32 predominantly 4:34 cuboidal epithelial cells. 4:39 Within the tubule of the nephrons, crystal-like structures can fall. 4:46 The crystal-like structures are essentially precipitants of some electrolytes 4:53 that have 4:54 accumulated there. 4:58 This crystal is actually a urinary stone. 5:03 If the crystal is small, it will just pass in the urine, but if it remains in 5:09 the kidneys 5:10 in the nephron, it can grow bigger and become a kidney stone. 5:15 A kidney stone again is basically a big crystal. 5:21 The kidney stone can lead to an obstruction. 5:25 The obstruction within the tubule can create a buildup of pressure in the tub 5:34 ule. 5:35 This pressure can cause irritation, and this irritation is read by the brain as 5:41 renal 5:41 colic. 5:46 There is also an inflammatory process going on due to the obstruction, and this 5:51 also leads 5:52 to the renal colic, the pain we feel when there is urinary stones in the body. 5:58 Alternatively, the urinary stone can lodge or get stuck within the ureter. 6:05 Remember the sites of constriction of the ureter? 6:08 Well, the stones can get stuck there, and when this happens, irritation and 6:13 pain can 6:14 occur due to stretching of the fibers that are there, which are caused again by 6:20 the 6:21 increase in pressure within the ureter. 6:26 With this increase in pressure proximally to the site of obstruction, and with 6:31 the irritation 6:32 going on, edema can occur, and the ureter will contract more vigorously, trying 6:41 to push 6:42 the stone out. 6:44 This is called hyperperistalsis. 6:51 And so, with this in mind, the clinical presentation of kidney stones can 6:57 include acute flank pain 6:59 which can radiate to the back or towards the groin and the flanks. 7:05 There can be associated fever because of the inflammation and nausea and 7:13 vomiting. 7:14 There can be also urinary frequency and urgency, hematuria, the person may 7:22 present to be obese. 7:28 The risk factors for developing a kidney stone include a high protein diet, 7:34 high salt diet, 7:35 male caucasian, obesity, dehydration, medications including antacids, and 7:48 carbonic and hydrasinhibitors. 7:52 Sodium and calcium containing medications also increases the risk of developing 7:58 kidney stones. 8:01 Crystal urea is also a risk factor as well as having a family history. 8:07 These risk factors will lead to a number of things. 8:11 First, some of these risk factors will increase urinary solute concentration, 8:19 including concentrations 8:21 of calcium, uric acid, and calcium oxalate and sodium. 8:27 Some of these risk factors will also decrease the stone forming inhibitors, 8:33 which include 8:34 citrate and magnesium. 8:37 The increase in urinary solutes and the decrease in urinary stone inhibitors 8:44 causes urine supersaturation 8:47 leading to urinary crystal formation, or urinary stone formation. 8:55 A decrease in urinary volume such as in dehydration and an excessive increase 9:01 or decrease in urinary 9:03 pH also contributes to urine supersaturation. 9:09 So in summary, urine supersaturation with stone forming salts results in 9:15 crystal formation. 9:18 Urinary stone formation. 9:22 And as I mentioned, there are a lot of types of urinary forming salts, such as 9:27 calcium, 9:27 uric acid, and oxalate. 9:31 And because of this, there are many types of stones, kidney stones. 9:35 The stone pathology can be broadly divided into five different types. 9:40 These include calcium oxalate stones, which make up the majority 75%. 9:45 There is also the calcium phosphate as well. 9:49 Stuvite is common in chronic urinary tract infections. 9:53 There is also uric acid stones and cysteine stones. 10:00 Negations for suspected renal calculae, renal stones include a full blood count 10:07 , CRP, magnesium 10:08 calcium phosphate levels, urinalysis, which may show hematuria, a 24-hour urine 10:18 calcium 10:19 level, phosphate level, oxalate, urate, cysteine, and xanthine levels. 10:26 And this can show us what type of kidney stone it might be. 10:33 X-ray can be performed to detect a kidney stone, and ultrasound can also detect 10:39 a kidney stone. 10:41 Kidney stone and ultrasound may show acoustic shadowing. 10:50 It may also reveal hydronephrosis if the obstruction is within a ureter causing 10:57 backflow of urine, 10:59 which will dilate the ureter, approximately. 11:03 Finally, a CT scan can also be used, which can show kidney stones. 11:10 Let's look at an algorithm. 11:14 Again, the clinical presentation of kidney stones include fever, nausea 11:21 vomiting, acute 11:23 flank pain, radiating to the groin or the back. 11:27 The pain is often described as stabbing and severe. 11:31 There is tachycardia with or without hematuria. 11:37 To try it for urinary or kidney stones, some say is fever, vomiting, and acute 11:43 flank pain. 11:49 So in an acute setting, analgesia is given with or without an anti-ametic to 11:55 prevent vomiting. 11:56 IV fluids are administered carefully. 12:03 Most urinary stones, if small, less than half a centimeter, will pass 12:09 spontaneously without 12:10 any intervention. 12:12 However, if intervention is required, it is either done electively or as soon 12:18 as possible. 12:19 By intervention, I mean surgical management. 12:24 And surgical management will depend on how big the kidney stone is, as well as 12:29 where the 12:30 kidney stone is if it is within the uretta or within the actual kidney. 12:39 Percutaneous nephrostomy allows placement of a small flexible rubber tube, a 12:45 catheter, 12:46 through the skin and into the kidney. 12:49 And this is in order to drain urine out if there is signs of obstruction. 12:56 This is more of a symptomatic relief. 12:59 In terms of removal of the kidney stone, there is ureteric stent insertion. 13:08 Here is the uretta, and let us say the stone is lodged within the uretta. 13:13 Well, a stent, a rod can be fed up through the urethra, through the bladder, 13:19 and up the 13:20 uretta to the side of obstruction. 13:22 And the stent can be placed there. 13:25 The stent will allow drainage of the urine, essentially bypassing the blockage. 13:32 The urine can then just drain straight into the bladder. 13:38 If the urinary stone is within the kidney, a procedure called a percutaneous ne 13:44 phrolithotomy 13:46 can be performed. 13:49 In this procedure, the aim is to remove the stone from the kidney by a small 13:55 puncture wound 13:56 through the skin. 13:59 It is most suitable for removal of stones that are more than, let us say, two 14:04 centimeters 14:04 in size, and which are present around the pelvic region of the kidney. 14:11 Another surgical procedure that can be done for urinary stones within the ure 14:15 ter or within 14:16 the kidneys is a simple endoscopic procedure that will break down the stone 14:22 within the 14:22 kidneys or the ureter. 14:24 Alternatively, there is open surgery to remove and break the stone. 14:29 Finally, there is the extra corporeal shockwave lithotripsy, which uses shock 14:36 waves to break 14:37 up stones that form in the kidneys to enable easy passage of these fragments 14:43 out of the 14:44 body within your own.