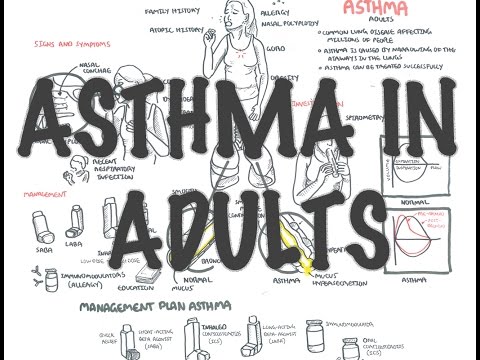
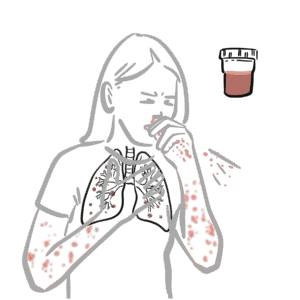
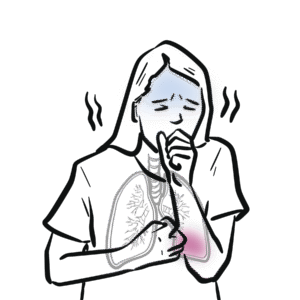
0:00 In this video we are going to talk about asthma. 0:13 So here I am drawing a human and his respiratory tract. 0:18 Asthma is defined as a chronic inflammation disorder of airways. 0:23 Asthma can be divided as either a topic or non-atopic. 0:29 Asthma is extrinsic asthma meaning it is triggered by the environment and this 0:38 type of asthma 0:39 is the most common. 0:41 A topic asthma involves inflammation mediated by systemic IgE production. 0:49 Non-atopic asthma on the other hand is an intrinsic asthma and this is far less 0:56 common. 0:57 Non-atomic asthma therefore refers to inflammation and constriction of the air 1:02 ways that is not 1:03 caused by exposure to an allergen. 1:07 The inflammation is mediated by local IgE production. 1:13 So now let us look at a cross-section of a normal lung, the bronchioles of a 1:17 normal 1:18 lung. 1:19 So here we have the mucous layer and we have pseudostratified endothelial cells 1:27 . 1:27 We have the lamina propria and we have the smooth muscles surrounding all this. 1:34 So that was normal and if we were to look at an asthmatic bronchiol, the lumen 1:41 here, 1:42 the inside is much narrower. 1:46 But before we focus on the asthmatic bronchiol and stuff like that, let us look 1:54 at the normal 1:55 histological layers of a bronchiol. 2:02 So here we have the mucous and on this layer we have the pseudostratified 2:08 columnar epithelial 2:10 cells. 2:12 Below this we have the basement membrane. 2:16 Within the epithelial layer we also can find goblet cells which are responsible 2:20 for secreting 2:21 mucus into the lumen. 2:27 Below the columnar cells we have the lamina propria which contain many cells 2:30 including 2:31 macrophages and mast cells. 2:34 Mast cells are responsible for secreting histamine. 2:38 Below the lamina propria or surrounding the lamina propria we have the smooth 2:43 muscles. 2:43 Now if we were to compare the normal bronchiolayer here to an asthmatic bronch 2:49 iolayer, we can 2:50 see many differences. 2:53 Firstly we can see that there is an increase in mucous production. 2:57 So there is an increase as well in goblet cells. 3:05 Also with this there is an increase in iscinephils in the mucus and tissue. 3:13 Here we have the pseudostratified columnar epithelial cells and below it the 3:18 basement 3:18 membrane thickens. 3:21 Lamina propria, within the lamina propria we see an increase in mast cell 3:26 numbers and 3:27 so we get an increase in histamine release. 3:31 We also have an increase in other cell types including neutrophils during 3:37 inflammation as 3:39 well as T helper cells. 3:43 We also can find that there is smooth muscle cell hypertrophy so smooth muscle 3:48 cells increase 3:49 in size and this is due to the constriction. 3:54 Now because of all these changes there are three characteristics of asthma, the 4:00 triad. 4:01 These are airflow obstruction, bronchiol hyper responsiveness, cause of hist 4:08 amine release and 4:10 inflammation due to the increase in neutrophils and other immune cells to the 4:16 area. 4:17 Symptoms of asthma include shortness of breath therefore, wheez, chest tight 4:23 ness and dry 4:24 irritating cough. 4:28 So now that we have identified some changes that occurs during in an asthmatic 4:34 bronchiol, 4:35 let us look at the pathophysiology. 4:40 So let's look at some players in the first in the pathophysiology of asthma. 4:45 So we have a main one, IgE antibodies. 4:51 Now IgE antibodies are important because they can bind to receptors on mast 4:56 cells forming 4:57 a mast cell IgE complex. 5:01 The mast cell IgE complex will recognize allergens and essentially begin 5:07 releasing heaps of histamine. 5:11 Other important players in the pathophysiology of asthma include is cinephils, 5:15 dendritic cells 5:17 as well as T helper cells. 5:20 Now there are two types of T helper cells, main overall types. 5:24 There's T helper 1 and there's T helper 2. 5:28 Now T helper 1 is normally found in the lungs. 5:32 So in normal lungs, T helper 1 are normally found. 5:37 However, there is an imbalance in asthma because in asthma, T helper 2 cells 5:44 which are not 5:46 normally found in the lungs are upregulated in asthma. 5:52 So we have more T helper 2 cells in the lungs of asthmatics. 5:59 T helper 1 you see normally promotes inflammation by increasing cell mediated 6:06 immunity. 6:07 However, T helper 2 cells promotes inflammation by increasing the humoral 6:14 immunity, so promoting 6:16 antibody production. 6:18 So I hope you can see how this correlates. 6:21 Anyway, let's put all these cells together and try to create a diagram looking 6:27 at the 6:27 pathogenesis of asthma. 6:30 And we're specifically focusing on atopic asthma. 6:35 So here we have the columnar pseudostratified columnar epithelial cells with go 6:38 blet cells 6:39 which secrete mucus on top and here we have the lumen. 6:43 So the pseudostratified columnar epithelial cells, we have the laminopropia 6:50 where we have 6:52 mast cells and dendritic cells and macrophages. 6:57 And okay, so in asthma, okay, let's just say an asthmatic inhales an allogen 7:03 and this 7:04 allogen will trigger a reaction. 7:07 So few things can happen. 7:10 One thing is that the allogen will be engulfed by dendritic cells and activates 7:16 the dendritic 7:17 cells. 7:19 Also the columnar epithelial cells will recognize this and secrete a substance 7:24 called thymic 7:25 stromal lymphocytes. 7:30 Thymic stromal lymphocytes will condition activated dendritic cells to produce 7:35 chemokines 7:36 to attract specifically T helper 2 cells. 7:41 The activated dendritic cell itself will activate the T helper cells to 7:45 differentiate 7:46 into T helper 2 and also will secrete chemokines to attract the T helper 2 to 7:52 the area, to 7:54 the bronchioles or the lungs. 7:58 So the activated T helper 2 cells does several things. 8:05 Firstly, the T helper 2's role is to promote the humoral immunity. 8:09 So it will stimulate plasma cells through interleukin 13 and interleukin 4. 8:14 And this will promote IgE production by the plasma cells. 8:19 IgE will obviously help, will bind onto mast cells to create the IgE muscle 8:26 complex. 8:27 And T helper 2 itself through interleukin 9 will stimulate or promote mast cell 8:35 activity. 8:36 Another important function T helper 2 cells do is that it will stimulate iscine 8:42 phyl production 8:43 from the bone marrow through interleukin 5. 8:46 So interleukin 5 will stimulate iscinephyl production so you get more iscineph 8:52 yls. 8:52 And with more iscinephyls there is a chemotactic basically thing occurring 8:58 which will attract 9:00 the iscinephyls to the area, to the lungs. 9:03 And so we have increase in iscinephyl amounts in the lungs. 9:09 So the inhaled allogen will bind onto IgE muscle complex. 9:17 And this will cause the mast cell to release a few things mainly histamine, 9:23 prostaglandins 9:24 and leukotriene. 9:26 All this specifically histamine will stimulate smooth muscles in the airways to 9:32 cause constriction. 9:34 So we get bronchoconstriction. 9:37 Also during this whole process the endothelial cell will release stem cell 9:42 factors that will 9:44 essentially maintain the mast cells to the area. 9:51 And so you can imagine that if there is this IgE being produced, essentially 9:58 this memory 9:59 being produced, whenever the same type of allogen is inhaled it will trigger 10:05 this whole 10:06 process of histamine release and bronchoconstriction and you get more iscineph 10:11 yls. 10:12 So you get this whole process still occurring and occurring. 10:16 So I hope you enjoyed this video on asthma and the pathophysiology of asthma. 10:21 Hopefully it made sense. 10:22 Thank you.