Overview
Community acquired pneumonia occur in individuals who are not in hospital (or have been in hospital in the past 48 hours) and who are not significantly immunocompromised. The World Health Organization estimates that lower respiratory tract infection is the most common infectious cause of death in the world. Choice of antibiotics are usually empirical because the aetiology is not known for at least 48 hours. For assessing severity and need for admission consider CORB or CURB -65.
| Definition Community Acquired Pneumonia: pneumonia occurring in individuals who are not in hospital (or have been in hospital for less than 48 hours) and who are not significantly immunocompromised. Nosocomial Pneumonia: pneumonia occurring within 48 hours of hospital admission. Early onset nosocomial pneumommniae is most often due to microorgniams that are also associated with CAP |
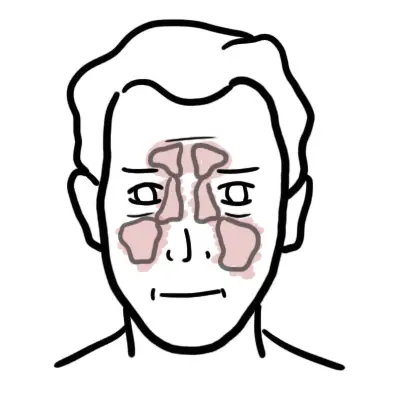
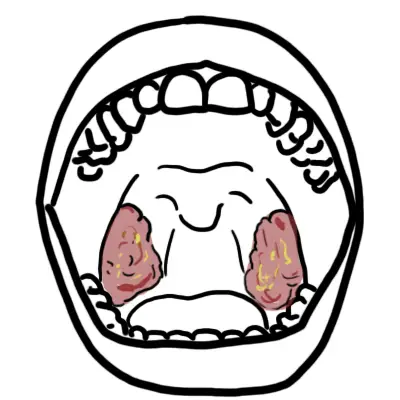
Respiratory System Defenses
The respiratory system is responsible for respiration. There is the upper respiratory tract (URT) and the lower respiratory tract (LRT).
The respiratory tract is thus a site where microbes can easily invade. Fortunately out respiratory system have defences in place to protect out body everyday. These defences include the cough reflex, mucus that lines all of our tract and alveolar macrophages.
The upper respiratory tract contain commensal microorganisms whereas the lower respiratory tract (LRT) is sterile. The commensal microbes of the URT can cause infection in certain situation such as when a person is immunocompromised.
Aetiology and Risk Factors
Aetiology
There are hundreds of microbes that can cause community acquired pneumonia. The most common being bacterial and viral. Streptococcus pneumonia is the most common cause of CAP. Some bacteria and virus can cause a more severe pneumonia that requires hospitalisation these include gram negative bacteria as well as staphylococcus aureus. Fungal pneumonia are more common in the elderly and immunocompromised. Whereas parasitic causes are more common in tropical, non-suburban areas.
Aetiology by age group Streptococcus pneumonia is the most common cause of CAP and is prevalent in all age groups. Viral causes are more common in young children and neonates, where as the gram negative bacteria and S. Aureus are more common in older adults.
Risk Factors
- Elderly
- Recent antibiotic use
- Smoking
- Recent travels
- Immunocompromised
- Respiratory disease
- Recent respiratory infection
Clinical Manifestation
Clinical presentation
- Fever or hypothermia
- Sweats, rigors or chills
- Cough, sputum production
- Dyspnoea
- Pleurisy
- Pulmonary lesions observed on radiographic examination
- Nonspecific symptoms are common, including loss of appetite, fatigue, and confusion.
Examination – consolidated lobe
- Dullness on percussion
- Bronchial breath sounds
- Reduced air entry
- Crepitations
- Increased vocal resonance
Diagnosis
- Sepsis
- Asthma exacerbation
- COPD exacerbation
- Acute bronchitis
- Acute exacerbation of bronchiectasis
- Acute exacerbation of pulmonary fibrosis
- Acute eosinophilic pneumonitis
- Pulmonary infarction
- Congestive heart failure (pulmonary oedema)
- Pulmonary infarct/haemorrhage
- Lung cancer
- Tuberculosis
Investigations
Investigations Chest X-ray may show site of consolidation. Arterial blood gas is done to check for severity. Normal blood tests should be ordered. Microbiology tests including sputum and blood cultures are ordered before administering antibiotics. in most cases the pneumonia resolves without the causative agent identified. Other specific investigations include urinary antigen for pneumococcal and legionnaires disease.
Classification
There are over 100 microbes (virus, bacteria, parasite, fungi) that can cause community-acquired pneumonia. Bacteria are the most common cause of CAP and have traditionally been divided into two groups, “typical” and “atypical” agents.
Typical: S. pneumoniae, H. influenzae, S. aureus, group A streptococci, Moraxella catarrhalis, anaerobes, and aerobic gram-negative bacteria.
Atypical: Legionella spp, M. pneumoniae, C. pneumoniae, and C. psittaci
The severity of pneumonia can help guide the need for hospitalisation, management and predict mortality. There are a few indices developed for assessing the severity of pneumonia including: CURB-65, SMART-COP and PSI. CURB- 65 is less complex and allows for quick assessment.
Treatment
- Oxygen
- Analgesia for chest pain
- Antibiotics (IV or oral)
- Steroids (could be considered in severe pneumonia although
| Side note Antibiotic therapy depends on severity of pneumonia. For mild pneumonia oral antibiotics, and IV are used for moderate and severe cases. Usually a combination therapy with beta-lactams (for gram positive) and macrolide/erythromycin (for gram negative). |
| Remember Most patients with non-severe CAP can be treated for 3-5 days with antibiotics. |
Complications and Prognosis
Complications
- Acute Respiratory Distress Syndrome
- Empyema
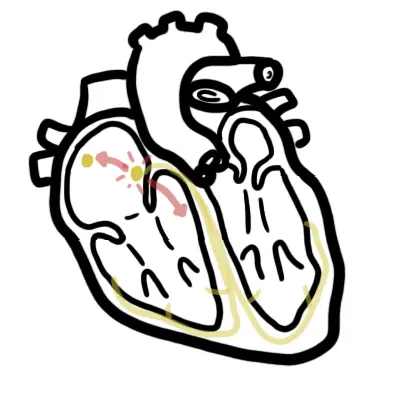
- Exacerbation of congestive cardiac failure
- Acute coronary syndrome
- Cardiac arrhythmia
- Clostridium difficile associated diarrhoea with overuse of antibiotics
| Remember Studies have found a close link between the inflammatory state in pneumonia and risk of a cardiovascular event. It is important to be aware of potential complications of pneumonia both short and long term. |















Discussion