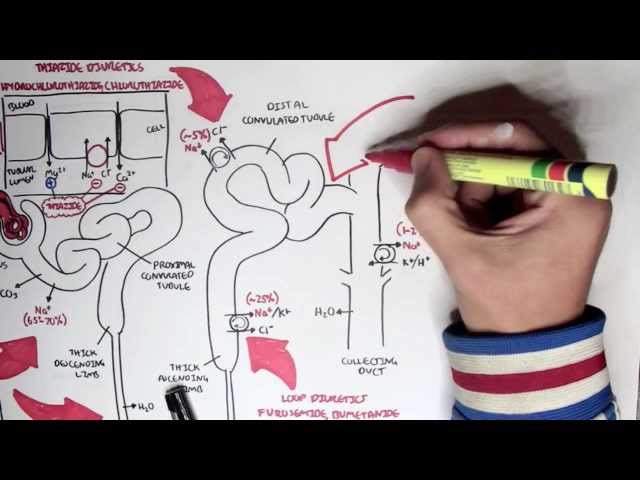
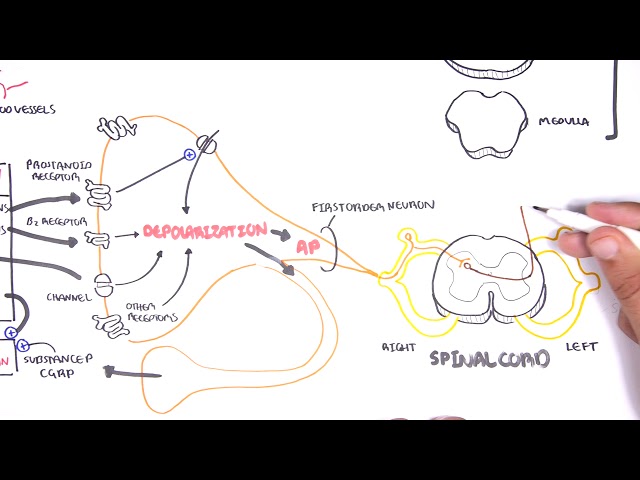
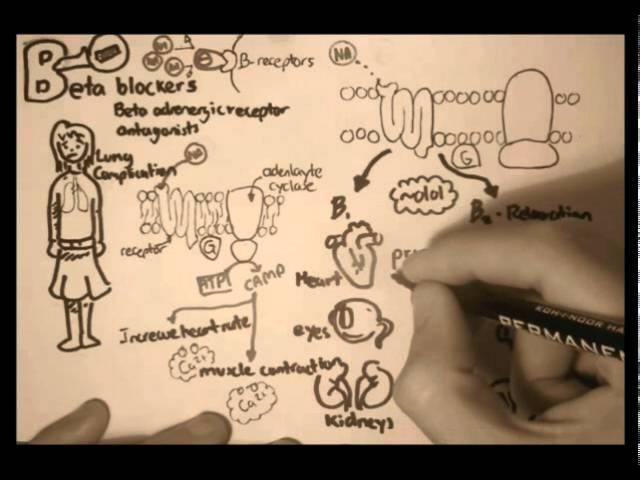
0:00 Hello, in this video, we're going to talk about anti-hypertensives, so 0:08 medication to 0:09 lower blood pressure. 0:12 So the hot pumps oxygenated blood around our body. 0:17 The hot first pumps this blood through the arteries, and this is in red here. 0:24 And then once the oxygenated blood is distributed around the body tissues, the 0:28 blood is then 0:29 brought back to the heart via the veins here in blue. 0:35 Focusing first on the heart, the heart actually pumps a certain amount of blood 0:41 each time 0:42 it contracts. 0:43 And this is the cardiac output. 0:46 The cardiac output allows blood to flow through the arteries and deliver oxygen 0:52 ated blood 0:52 to tissues before returning back to the heart via the veins. 0:58 The cardiac output itself has a big impact on blood pressure. 1:04 Other organs responsible for or plays a role in regulating blood pressure 1:08 include the liver, 1:09 lungs, kidneys, and the endocrine organ above the kidneys called the adrenal 1:15 glands. 1:16 When we talk about blood pressure, we are really talking about the arterial 1:21 blood pressure, 1:22 so the mean arterial pressure. 1:26 And this mean arterial pressure can be calculated by having cardiac output 1:32 multiplied by the 1:33 total peripheral resistance, TPR. 1:37 And TPR is the resistance of the vessels of the artery in this case. 1:45 To make things even more complicated, the blood pressure we know has two 1:49 numbers, one 1:50 on top called the systolic and one number on the bottom called the diastolic 1:56 blood pressure. 1:58 The systolic blood pressure is essentially the pressure of the arteries when 2:02 the heart 2:03 is pumping blood out. 2:05 And the diastolic blood pressure is the pressure in the arteries when the heart 2:10 is filling back 2:11 with blood. 2:13 High blood pressure is about 120 over 80. 2:20 Hypertension means high blood pressure. 2:23 Many things can cause hypertension. 2:26 Persistent, untreated, or unmanaged, hypertension can have serious consequences 2:32 . 2:33 And one way to treat hypertension is by using antihypertensives or medication 2:38 to treat hypertension. 2:40 And these medications can be remembered by the alphabet. 2:43 So A, B, C, D, and E. Let's begin by looking at A. So A includes ACE inhibitors 2:52 , angiotensin 2:54 receptor blockers, and alpha-one receptor blockers. 2:59 Now before focusing on these, let's just recap some physiology. 3:04 So the liver produces this molecule called angiotensinogen. 3:10 When there's a decrease in blood pressure in the arteries, the kidneys will 3:14 detect this 3:15 and then produce a molecule called renin. 3:19 Now renin enters circulation and is responsible for converting angiotensinogen 3:25 produced by 3:26 the liver into angiotensin-1. 3:30 Angiotensin-1 will then circulate around the body and get in contact with a 3:35 membrane-bound 3:36 enzyme called ACE. 3:39 Or angiotensin-converting enzyme, which mainly resides in the lung tissues. 3:45 So ACE converts angiotensin-1 to angiotensin-2. 3:51 Angiotensin-2 is an important regulator of blood pressure. 3:56 And what it does is basically it increases blood pressure via a number of 4:02 mechanisms. 4:04 Angiotensin-2 binds onto angiotensin-2 receptors on many different types of 4:09 cells around our 4:10 body. 4:12 And depending on what cell angiotensin binds to, its effect on the body differs 4:18 . 4:18 So, but essentially, it will result in an increase in blood pressure. 4:23 So for example, some of the effects of angiotensin-2 includes increasing 4:28 sympathetic activity, 4:31 vasocrytic restrictions, stimulating the release of aldosterone or hormone from 4:36 the 4:36 adrenal cortex. 4:38 And these effects, all of them, will lead to an increase in blood pressure. 4:45 ACE inhibitors, or angiotensin-converting enzyme inhibitors, is a very common 4:52 anti-hypertensive. 4:54 These medications can be remembered by the ending pril. 5:00 So for example, kaptopryl, ramopryl, they all end in prils usually. 5:06 The mechanism of action of ACE inhibitor is that it inhibits ACE, the enzyme 5:12 membrane 5:13 bound enzyme. 5:15 And so it inhibits the conversion of angiotensin-1 to angiotensin-2. 5:19 And because you have less angiotensin-2, it means that you will decrease blood 5:23 pressure 5:24 because it's not working. 5:26 Some side effects of ACE inhibitors include a dry cough, a rash, nausea 5:32 vomiting, diarrhea, 5:34 angioedema, and headache. 5:37 There are contraindications to using ACE inhibitors, or relative or absolute. 5:42 And these include being pregnant, having a bad asthma, chronic cough, being 5:48 allergic 5:49 to ACE inhibitors, having a kidney disease, particularly renal stenosis. 5:57 The other medication that starts with A is the angiotensin-receptor blocker. 6:02 And as the name suggests, the mechanism of action, it blocks the binding of ang 6:07 iotensin-2 6:08 to its receptor. 6:12 And so thus it will decrease the activity of angiotensin-2, which will result 6:17 in a decrease 6:17 in blood pressure. 6:20 The side effects of angiotensin-receptor blockers include headache, nausea, 6:24 diarrhea, dizziness, 6:26 and back pain. 6:28 Some contraindications include pregnancy, renal stenosis, bilaterally, and if 6:33 they are allergic 6:34 to angiotensin-receptor blockers. 6:38 It's interesting to note that angiotensin-receptor blockers are usually used as 6:41 an alternative 6:42 to ACE inhibitors, because people that use ACE inhibitors, getting a chronic or 6:47 getting 6:47 a dry cough is quite common. 6:49 And so sometimes people change to the angiotensin-receptor blockers. 6:56 Angiotensin-receptor blockers can be remembered because it usually ends in sart 7:02 an. 7:02 So for example, lost sartan, the sartans. 7:06 Anyway, the final anti-hypertensives that begin with A are the alpha-1 receptor 7:12 blockers. 7:13 And these guys aim is to work on the vessel epithelial cells. 7:19 So zooming into the blood vessels, here is the lumen of the blood vessel. 7:24 And surrounding the lumen is the endothelial cells and the smooth muscle cells. 7:31 The smooth muscle cells can contract usually and this will make the lumen of 7:36 the vessel 7:37 smaller. 7:39 Or the smooth muscle cells can relax and this will dilate the lumen, co-making 7:46 it wider. 7:47 So as you might suspect, when the smooth muscle cells contract and the lumen 7:51 becomes smaller, 7:52 the blood pressure increases. 7:56 The smooth muscle cells that surround the vessels have alpha-1 receptors. 8:02 These receptors react to noradrenaline, adrenaline, produced by the nerve 8:06 fibers or 8:07 from noradrenaline adrenaline in circulation. 8:11 Noradrenaline and adrenaline is the same thing as epinephrine or epinephrine. 8:15 Anyway, noradrenaline can bind to the alpha-1 receptor and this will cause or 8:22 stimulate 8:23 contraction of the smooth muscle cells. 8:26 The contraction of the smooth muscle cells that surround the vessel will cause 8:31 the vessel 8:32 to become more smaller, will narrow the lumen and this will lead to an increase 8:36 in blood 8:37 pressure. 8:40 Alpha-1 receptor blockers, they block alpha-1 receptors and thus the mechanism 8:44 of action 8:45 of alpha-1 receptor is that inhibits the adrenergic activity leading to the 8:50 decrease 8:50 in blood pressure. 8:53 Alpha-1 receptor blockers also have a role in decreasing total cholesterol in 8:57 the body. 8:58 Thus, it's a good option for people who have both high blood pressure and 9:02 cholesterol problems. 9:05 Side effects include it can lead to hypotension, so a drastic decrease in blood 9:12 pressure. 9:14 So they were the anti-hypertensives that begin with A. Let's look at the anti- 9:18 hypertensives 9:19 that begin with B. 9:21 It's easy, it's just beta blockers. 9:25 And beta blockers are very easy to remember, because they end usually in ollol, 9:29 like metaprolol 9:31 and libetalol, or lollolololololol. 9:34 Anyway, beta blockers block what are called beta receptors. 9:41 And beta receptors are important in the sympathetic activity. 9:46 So by blocking the beta receptors, you are blocking sympathetic activity, 9:50 essentially. 9:51 So there are beta receptors everywhere in the body, we mainly, we will mainly 9:56 concentrate 9:57 on the heart here. 9:59 So beta blockers can be selective and work specifically on the heart, or beta 10:06 blockers 10:06 can be non-selective and work on the periphery too, such as the blood vessels. 10:12 Well let's focus on the heart, the heart have these cells called pacemaker 10:18 cells, which 10:19 make up the conduction system of the heart. 10:22 The pacemaker cells regulate the heart rate, so how fast your heart is pumping. 10:28 The pacemaker cells can be influenced by many things, including the parasymp 10:33 athetic nervous 10:34 system and the sympathetic nervous system. 10:39 The pacemaker cells of the heart, they have receptors on them, the beta 1 10:45 receptors. 10:46 Adrenergic neurons, which are part of the sympathetic nervous system, target 10:51 these pacemaker 10:52 cells and release adrenaline and noradrenaline, which will bind onto these beta 10:56 1 receptors. 10:58 Thus, it will stimulate the pacemaker cells to fire more rapidly, which will 11:03 increase 11:03 the heart rate, and because you get an increase in heart rate, you will get an 11:08 increase in 11:09 blood pressure by increasing the cardiac output. 11:12 Further, the heart itself is a muscular organ, they are made up of cardiomy 11:19 ocytes, which are 11:20 basically the cardiac muscle cells. 11:24 The muscle cells of the heart, the cardiomyocytes, are the cells which contract 11:28 and help eject 11:29 blood out. 11:31 The heart muscle cells also contain beta 1 receptors, so noradrenaline and 11:37 adrenaline 11:38 released by adrenergic cells, the sympathetic nervous system, can stimulate the 11:43 beta 1 receptors 11:44 of the cardiac muscle cells, which will cause the cardiac muscle cells to 11:49 contract stronger. 11:51 And to be exact, it will lead to a more powerful contraction. 11:56 With a more powerful contraction, the heart is able to increase cardiac output, 12:01 and because 12:02 you are increasing cardiac output, you will increase blood pressure. 12:10 Beta blockers selective for the heart work by inhibiting beta 1 receptors. 12:17 The mechanism of action of beta blockers is that they block the sympathetic 12:21 function on 12:21 the heart by blocking the beta 1 receptors. 12:25 And they do this by two ways. 12:26 First, by decreasing the heart rate, which will decrease cardiac output and 12:30 then decrease 12:31 blood pressure, or they will decrease the myocardial contraction, the strength, 12:36 and thus 12:37 decreasing cardiac output, which will subsequently decrease blood pressure. 12:41 Side effects of beta blockers include radiocaria, fatigue, hypotension, 12:46 decrease in libido, 12:48 impotence, and bronchoconstriction. 12:52 Contradications include obstructive lung disease and peripheral vascular 12:58 disease. 12:59 So that was the anti-hypertensives with B. Let's look at C, anti-hypertensives. 13:04 And the Cs are the calcium channel blockers. 13:09 Most names for calcium channel blockers, they end in or sound something like 13:17 the pain 13:18 or like mill. 13:21 So for example, varapamil. 13:23 But these guys are kind of hard to remember, but hopefully you get the idea. 13:29 Anyway, in order to understand calcium channel blockers, we need to understand 13:34 calcium and 13:35 its role in the body. 13:37 When you think of calcium, think of muscle contraction, think of excitability. 13:43 Calcium channels are important channels in our body that allow the movement of 13:47 calcium 13:48 in and out of cells or cellular organelles. 13:53 There are two main calcium channels we will talk about. 13:56 And these are the T-type calcium channels and the L-type calcium channels. 14:01 But what these drugs do is that, as the name suggests, they block calcium 14:07 channels. 14:08 More specifically, they block T-type calcium channels and/or L-type calcium 14:13 channels. 14:14 So there are L-type calcium channel blockers or T-type calcium channel blockers 14:20 or both. 14:21 And it's important to know this because these channels are found in different 14:25 parts of our 14:26 body. 14:27 For example, in the heart, going back to our pacemaker cells which control the 14:31 heart rate, 14:32 there are T-type calcium channels. 14:36 Calcium activity in the pacemaker cells causes the heart to pump faster and so 14:41 it contributes 14:42 to increasing the blood pressure. 14:46 Think of T-type calcium channels as time, so T for time, because the pacemaker 14:52 cells 14:52 of the heart control the heart time, the heart rate. 14:57 And so by using the T-type calcium channel blockers, it will block calcium 15:02 activity and 15:03 thus decrease heart rate, decreasing cardiac output and then decreasing blood 15:10 pressure. 15:11 This might get confusing, but there are three types of T-type calcium channel 15:16 blockers. 15:17 These are the phenyl alkalines such as verapamil, the benzothiazapine such as d 15:23 iltiazim, and 15:24 the dihydroperidine such as the ones that end in the pain. 15:29 So they are all different, but to put it simply, they just work differently and 15:35 they also work 15:35 on L-type calcium channels. 15:38 But anyway. 15:40 So for example, here is verapamil, a common calcium channel blocker, which will 15:45 block 15:46 the T-type calcium channels of the pacemaker cells. 15:50 Let's talk about the L-type calcium channels, which are found on smooth muscle 15:55 cells. 15:56 So here we have the blood vessel, which as we know contains smooth muscles. 16:02 And here is the lumen of the vessel for example. 16:06 The L-type calcium channels allow influx of calcium into the muscle filaments 16:10 which will 16:10 cause contraction. 16:12 This will increase the blood pressure because it causes the vessels to contract 16:15 and become 16:16 more narrow. 16:19 But the L-type calcium channels are also found in the cardiomyocytes and thus 16:25 they will increase 16:27 the power of contraction of the cardiomyocytes, which will further increase 16:32 cardiac output 16:33 and so blood pressure. 16:37 L-type calcium channel blockers are the dihydropyridines, where that end in the 16:42 pain. 16:44 Some of the drugs from dihydropyridine also block T-type calcium channels, and 16:50 so is also 16:50 part of the T-type calcium channel category. 16:55 A common example of a L-type calcium channel blocker is nephidipine. 17:02 And effects of the dihydropyridines, like a lot of anti-apartensives, are fl 17:06 ushing, headache, 17:07 dizziness from hypotension, palpitations, and peripheral edema. 17:14 Contradications of calcium channel blockers are congestive heart failure, heart 17:18 block, 17:19 hypotension, and ventricular tachycardia. 17:22 And this is unique to calcium channel blockers because in heart failure, the 17:27 heart is trying 17:27 to compensate by contracting a lot harder. 17:32 And so if you use a calcium channel blocker, specifically an L-type calcium 17:36 channel blocker, 17:37 you are weakening, or you are reducing the strength of contraction of the heart 17:42 . 17:42 And this is what you do not want to do in people who have heart failure. 17:47 So that was the C anti-apartensives medication, the calcium channel blockers. 17:51 Next is D for diuretics. 17:53 So when we think of diuretics, we think of the kidneys. 17:59 Diuretics works on the kidneys, and what they essentially do is induce diuresis 18:03 , cause peeing. 18:05 So when we pee, the water in our body, it drops, and this will then, you know, 18:10 drop blood pressure. 18:13 So here is the kidneys with the adrenal glands above it. 18:17 And the functional unit of the kidneys, or the main players of the kidneys, are 18:22 these 18:23 things called nephrons, and there are millions of nephrons in the kidneys. 18:27 And this is where diuretics work. 18:31 And it's important to understand that the nephron, the functional unit of the 18:35 kidneys, 18:36 they filter things from blood, and they allow for secretion and reabsorption of 18:42 things 18:43 in and out of the blood vessel. 18:45 So here I'm just going to draw a vessel, a vein, let's just say, a vessel. 18:50 And so the mechanism of action of diuretics, again, is to increase urine output 18:57 , decrease 18:58 fluid overload, and this will decrease blood pressure. 19:04 And there are three types of diuretics, three main ones. 19:08 These are the lube diuretics, which is the strongest of the lot, the thiazide 19:12 diuretics 19:13 and the potassium sparing diuretics. 19:16 The nephron is divided into different sections, one of which is the lube of Hen 19:23 le. 19:23 In the lube of Henle, in the ascending part, there is this channel, a symptom 19:28 which transports 19:29 one sodium molecule, two chloride molecules, and one potassium from the nephron 19:34 back into 19:35 circulation, back into the blood vessel. 19:38 When sodium is reabsorbed in the blood, water follows. 19:43 Lube diuretics inhibit the transport, this transporter by inhibiting the 19:49 movement of chloride ions, 19:52 which will disrupt the whole transport. 19:55 And so you don't get sodium moving into the blood vessel, and so you don't get 20:00 water 20:01 following, and so you don't get an increase in blood pressure. 20:06 Phiazide diuretics work on the distal part of the nephron. 20:10 There is a transporter here which reabsorbs sodium and chloride together. 20:16 This will then draw water back into the blood as well, which will increase the 20:20 blood pressure 20:21 in the body. 20:22 Phiazide diuretics block this transporter, and so block sodium reabsorption and 20:28 thus water 20:30 reabsorption causing a decrease in blood pressure. 20:34 In the distal part of the nephron, there is also this other transporter exch 20:38 anger, which 20:39 reabsorbs sodium, but secretes potassium. 20:45 And potassium sparing diuretics inhibit this transporter, and by inhibiting 20:51 this transporter, 20:53 you actually decrease the reabsorption of sodium, which means you decrease the 20:56 reabsorption 20:57 of water, which subsequently decreases blood pressure, but you also prevent the 21:03 secretion 21:04 of potassium. 21:05 And this is why it is called a potassium sparing diuretic, because you are 21:10 sparing potassium. 21:12 And so all these diuretics, they essentially inhibit sodium from going into the 21:17 blood, and 21:18 so you have more sodium being peed out, which means that you have more water 21:22 being peed 21:22 out, which means that you will decrease blood pressure. 21:27 Side effects of lube diuretics and thiazide diuretics include hypokalemia, hyp 21:33 onaturemia, 21:34 hypovolemia, hypotension, hyper uresemia, which increases the risk of gout, 21:42 hyperglycemia, 21:44 hypercalcemia, metabolic alkalosis, and pancreatitis. 21:52 The side effects of potassium sparing diuretics is quite different in that they 21:56 can cause hypercolemia, 21:58 metabolic acidosis, and gynecomastia. 22:03 If you want to know more about diuretics, I have a separate video on the 22:07 pharmacology 22:07 of diuretics. 22:08 Finally, E and anti-hypertensives is for endothelium receptor antagonist. 22:15 And these guys basically relax the blood vessel, causing vasodilation, which 22:19 will cause a decrease 22:20 in blood pressure. 22:22 They work on the blood vessel. 22:24 The smooth muscle cells contain endothelin-1 receptors, which when endothelin, 22:30 a molecule 22:31 produced by the blood vessel itself, binds onto it, it will cause contraction 22:35 and narrowing 22:36 of the blood vessel, which will cause an increase in blood pressure, of course. 22:40 While endothelin receptor antagonists, as the name suggests, inhibits this 22:46 receptor, which 22:47 means you don't get contraction of the vessel, which means that you will lower 22:52 the blood 22:53 pressure. 22:56 The side effects of endothelin receptor antagonists include headache, 23:01 peripheral edema, nasal congestion, 23:04 nausea, hypotension, and palpitations. 23:10 So that concludes the video on the anti-hypertensive medications. 23:13 We looked at A, B, C, D, and E, A for ACE inhibitors, angiotensin receptor 23:18 blockers, and alpha-1 23:21 receptor antagonists, and we also looked at B for beta blockers, C for calcium 23:26 channel 23:26 blockers, D for diuretics. 23:28 And finally, we just looked at E for endothelin receptor antagonists. 23:31 Anyway, I hope you enjoyed this video. 23:33 I hope it was helpful. 23:34 Thank you for watching. 23:35 Bye.