Overview
In the clinical setting, iron deficiency is the most common cause of anaemia. Iron Deficiency is lack of iron in the body resulting from inadequate iron intake, increased iron loss and increased iron demand which can lead to anaemia. Iron is an integral part of haemoglobin the oxygen carrying protein. Without iron, oxygen is unable to be carried resulting in anaemia.
| Definitions Anaemia (Anemia): The World Health Organization defines anaemia as a haemoglobin (Hb) concentration below 13 g/dl (130 g/L) in men over 15 years of age, below 12 g/dl (120g/L) in non-pregnant women over 15 years of age, and below 11 g/dl (110g/L) in pregnant women Iron deficiency anaemia: Most common type of anemia, and it occurs when your body doesn't have enough of the mineral iron Microcytic anemia Defined as the presence of small, often hypochromic, red blood cells in a peripheral blood smear and is usually characterized by a low mean cell volume (MCV) (<83 micron3). Iron deficiency is the most common cause of microcytic anemia. Normocytic anaemia: defined by a normal mean corpuscular volume (MCV), but the hemoglobin and hematocrit are decreased. Usually a result of hemolytic anaemia or anaemia of chronic disease Mactocytic anaemia (Macrocytosis): defined as a mean corpuscular volume greater than 100 fL, is frequently encountered when a complete blood count is performed. The most common etiologies are alcoholism, vitamin B12 and folate deficiencies, and medications. |
Epidemiology More than one-quarter of the world's population is anaemic. Approximately one-half of this burden is a result of iron deficiency anaemia, being most prevalent among preschool children and women. Iron deficiency anaemia occurs in 2–5% of adult men and postmenopausal women in the developed world and is a common cause of referral to gastroenterologists.
Iron Metabolism
Overview Most body iron (ie, 2.6g of 3–4 g) circulates as haemoglobin (Hb), which is recycled when red cells senesce.
- One gram is stored in the liver, and 0.4 g in myoglobin and cytochromes.
- Small amounts (3 mg) circulate bound to plasma transferrin.
- Men and non-menstruating women lose about 1 mg of body iron per day
- Menstruating women may lose an additional 1 mg daily on average.
Dietary source of Iron
- Animal Meat
- Fish
- Green Vegetables
- Cereal
Risk Factors
Decrease in iron intake or impaired Absorption
- Vegan diet
- Low socioeconomic status
- Gastrectomy
- Coeliac Disease
Increase in iron loss
- Menorrhagia
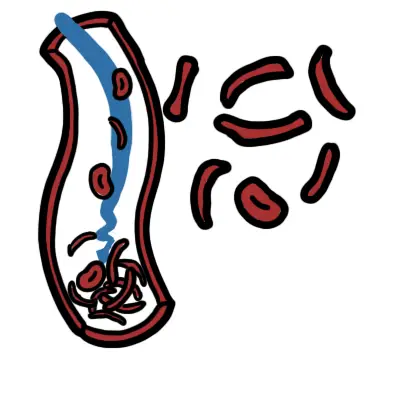
- Hookworm
- NSAID use
- Gastrointestinal Bleeding
Increase in iron demand
- Pregnancy
- Infancy
| Side note Our body needs iron 1mg/day. Pregnant women need 5-6mg/day. |
Sign and Symptoms
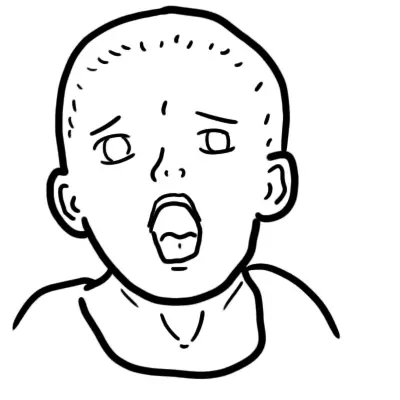
Anaemia
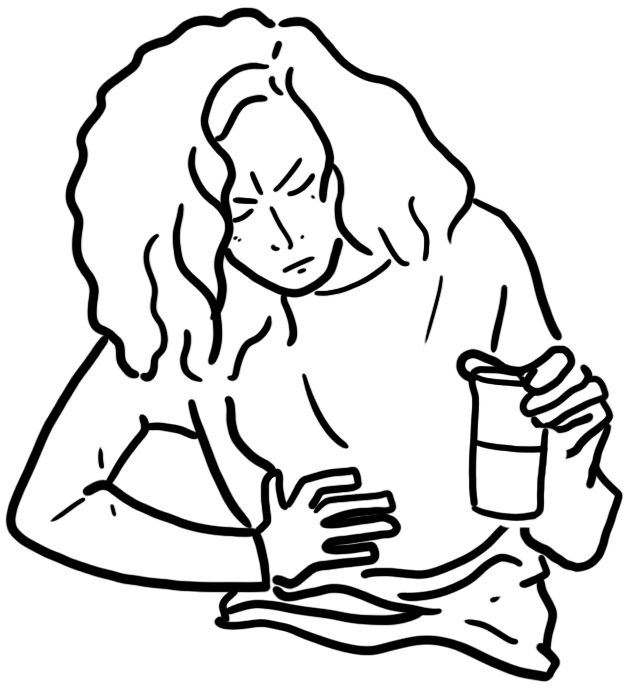
- Fatigue
- Headache
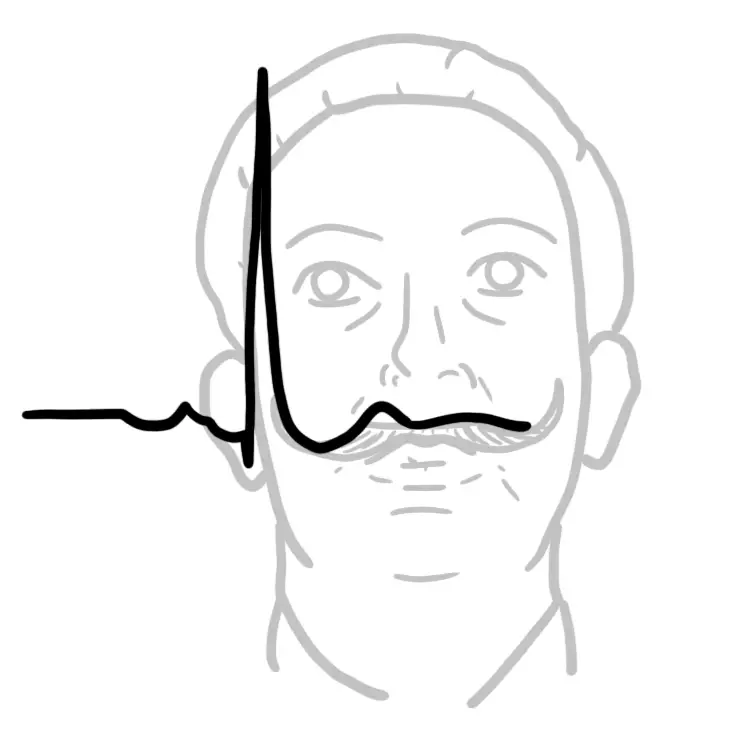
- Palpitations
- Pallor
- Nausea
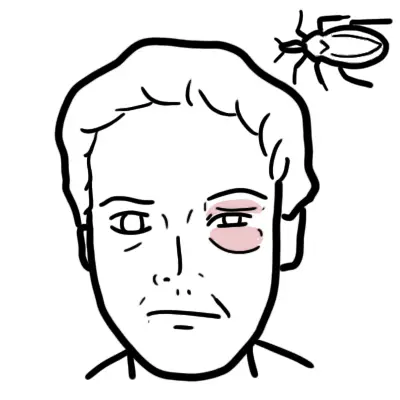
Iron Deficiency
- Pica (Pica is the abnormal craving or appetite for non-food substances, such as dirt, ice, paint, or clay.)
- Nail changes (koilonychia-spoon shaped nails)
- Hair Loss
- Glossitis and Angular stomatitis
- Restless Leg Syndrome
Patients with iron deficiency anemia are often asymptomatic and have limited findings on examination.
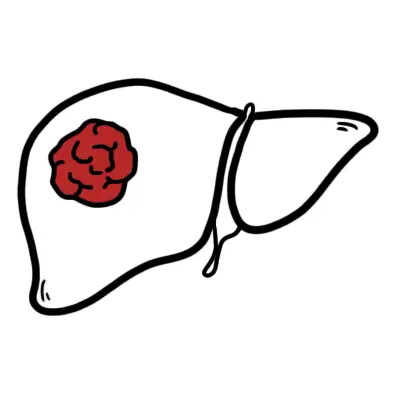
| Remember Elder patient presenting with iron deficiency must be investigated for colon cancer malignancy even in the absence of Foecal blood. |
Differential Diagnosis
Anaemia
- Vitamin B12 deficiency
- Folate deficiency
- Thalessemia - also hypochromic and microcytic
- Anaemia of chronic disease
- Sideroblastic
Iron Disorder
- Atransferrinaemia
- Lead toxicity
Investigations
The lower the haemoglobin the more likely there is to be serious underlying pathology and the more urgent is the need for investigation. Patients without a clear physiological explanation for iron deficiency (especially men and postmenopausal women) should be evaluated by gastroscopy/colonoscopy to exclude a source of gastrointestinal bleeding, particularly a malignant lesion.
- Full blood count
- Haemoglobin/Haematocrit: decreased
- Mean cell volume (MCV): decreased
- Red cell distribution of width: increased because as iron decreases cell become smaller increasing distribution
| Think In anaemia of chronic disease the RDW decreases the red blood cells are of similar size. |
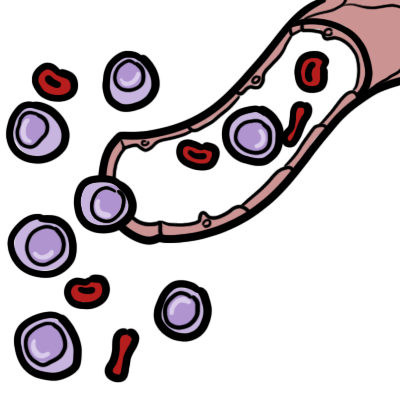
- Peripheral blood smear: microcytic, hypochromic red blood cells
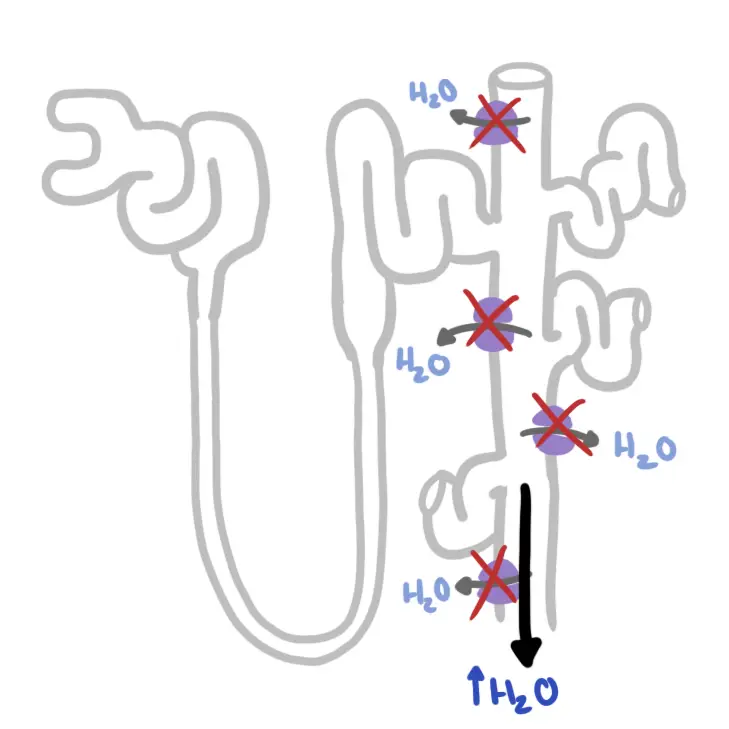
- Iron studies
- Serum iron: decreased
- Total iron-binding capacity: increased
- Transferrin Saturation: decreased (transferrin is being over produced to compensate for low iron)
- Serum Ferritin: reduced. Ferritin reflects iron stores and is the most accurate test to diagnose iron deficiency anemia
| INTERPRETING PLASMA IRON STUDIES | |||
| Condition | Iron | Total Iron Binding Capacity | Ferritin |
| Iron deficiency | ↓ | ↑ | ↓ |
| Anaemia of chronic disease | ↓ | ↓ | ↑ |
| Chronic Haemolysis | ↑ | ↓ | ↑ |
| Haemochromotosis | ↑ | ↓ (or ↔) | ↑ |
| Pregnancy | ↑ | ↑ | ↔ |
- Endoscopy: check for peptic ulcer disease, coeliac disease, other gastrointestinal bleeding conditions
- Colonoscopy
- Coeliac disease screening at any age?
| Remember IDA may be effectively diagnosed in most cases by full blood examination and serum ferritin level. Serum iron levels should not be used to diagnose iron deficiency. |
| Side note A complete blood count can be helpful to determine the mean corpuscular volume or red blood cell size. Although iron deficiency is the most common cause of microcytic anemia, up to 40 percent of patients with iron deficiency anemia will have normocytic erythrocytes. |
Diagnosis
Diagnosis of iron deficiency anemia requires laboratory-confirmed evidence of anemia, as well as evidence of low iron stores. Anemia is defined as a hemoglobin level two standard deviations below normal for age and sex
| Think Iron deficiency anaemia and thalassaemia trait are the commonest causes of microcytic anaemia, but they may coexist. Serum ferritin and haemoglobin A2 quantitation are the two most important investigations to distinguish between iron deficiency anaemia and thalassaemia trait. |
Aetiology
Once iron deficiency anaemia is identified, the goal is to determine the underlying aetiology.
- Decreased iron intake
- Poverty
- Starving
- Patient not taking oral iron therapy
- Patient taking an iron supplement or multivitamin tablet with insufficient iron content
- Inadequate diet or impaired absorption
- Concomitant consumption of inhibitors of iron absorption (eg, tea, calcium, antacids, tetracycline, within 2 hours of iron ingestion)
- Coexisting inflammation with functional iron deficiency
- Intestinal mucosal disorders (eg, coeliac disease, inflammatory bowel disease)
- Impaired gastric acid secretion (including use of proton pump inhibitors)
- Gastric/intestinal bypass procedures
- Helicobacter pylori colonisation
- Controlled-release iron formulations may contribute (ie, potential for limited iron absorption in some patients
- Increased iron loss
- Occult, undiagnosed or recurrent gastrointestinal blood loss (eg, peptic ulcer, malignancy, angiodysplasia, small bowel lesion, parasites)
- Other source of recurrent blood loss (eg, menorrhagia due to uterine pathology or an inherited bleeding disorder such as von Willebrand disorder)
- Multiple sources of recurrent blood loss (eg, hereditary haemorrhagic telangiectasia)
- Ongoing urinary iron losses (eg, significant valve haemolysis)
- Renal failure responding to erythropoietin-stimulating agents
- Increased iron requirements
- Coexisting condition interfering with bone marrow response
- Superimposed infection, inflammation, malignancy or renal failure
- Concomitant B12 or folate deficiency
- Coexisting primary bone marrow disease or suppression
- Unknown cause (congenital iron deficiency)
Patients with an underlying condition that causes iron deficiency anemia should be treated or referred to a subspecialist (e.g., gynecologist, gastroenterologist) for definitive treatment.
| Remember Gastrointestinal, Genitourinary sources of bleeding should always be excluded. |
Pathophysiology
1. Iron is required for the formation of the haem moiety in haemoglobin, myoglobin, and haem enzymes, also known as cytochromes.
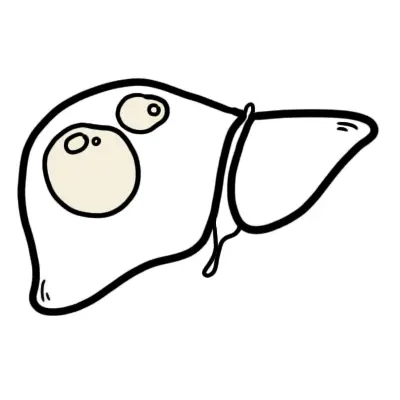
2. Iron can also be stored in the form of ferritin
3. Iron Deficiency can be a result of:
- Decreased iron intake because of inadequate diet or impaired absorption
- Increased iron loss
- Increased iron requirements
- Depletion of Iron stores
4. Anaemia then results in decreased oxygen-carrying capacity and the resultant symptoms of fatigue, low energy level, and dyspnoea on exertion.
Treatment and Management
- Oral iron replacement OR
- Parenteral iron replacement
- Blood transfusion - serious cases with low haemoglobulin
- Ascorbic acid (helps in the absorption of iron)
- Improve diet
| Remember Oral iron therapy, in appropriate doses and for a sufficient duration, is an effective first-line strategy for most patients. |
Complications and Prognosis
Complications
- Diastolic heart failure
- Impaired muscular performance
- Cognitive impairment
- Developmental delays
Prognosis
With treatment, the outcome is likely to be good. However, it does depend on the cause (i.e the cause is cancer). Once haemoglobin is corrected, it takes an additional 6 months or so of iron replacement therapy to restore iron stores.
Iron-deficiency Anaemia and Children
Overview Worldwide, anemia affects up to one-half of children younger than five years. Anemia is defined as a hemoglobin level that is two standard deviations below the mean for age.
| Remember Anemia can be categorized as microcytic, normocytic, or macrocytic. Microcytic iron deficiency anemia is a common cause of childhood anemia, whereas macrocytic anemia is rare in children |
Risk Factors
- Low birth weight
- History of prematurity
- Exposure to lead
- Exclusive breastfeeding beyond four months of life
- Weaning to whole milk and complementary foods without iron-fortified foods.
Although iron deficiency anemia is associated with cognitive delays in children, it is unclear if iron supplementation improves cognitive outcomes.
Signs and Symptoms
- Early symptoms: poor attention span, irritability
- Later symptoms & signs: cognitive deficits, lethargy, pallor, poor growth, weakness, listlessness, dyspnoea/ tachypnoea, conjunctival pallor, tachycardia pica, poor feeding, cardiomegaly & signs of cardiac failure
Other differentials of microcytic anaemia to consider in children
Thalassaemia minor
- microcytosis with normal or bordeline low Hb
- diagnosed on Hb electrophoresis - HbA2 > 3.5%
- South East Asian, Mediterranean, Arabic families
- usually asymptomatic; often positive family history
- pre-pregnancy carrier testing of partner important
Alpha Thalassaemia
- microcytosis with normal or bordeline low Hb
- South East Asian, African Arabic families
- cannot be easily diagnosed on Hb electrophoresis - dna testing usually required (not a first-line investigation - exclude other causes first)
Rare causes of Microcytic Anaemia
- Chronic inflammation
- Chronic lead poisoning (high blood lead level)
- Sideroblastic anaemia
Hypoplastic/Aplastic Anaemia
(eg. acute leukaemia, aplastic anaemia, infiltrative disorders)
- Consider if white cells and/or platelets also depressed
- May be due to drugs eg. cytotoxics, chloramphenicol, sulfonamides
- If isolated anaemia, consider transient erythroblastopenia of childhood (response to viral infection) or congenital forms (eg. Diamond-Blackfan syndrome)
- Bone marrow aspirate is usually required for diagnosis