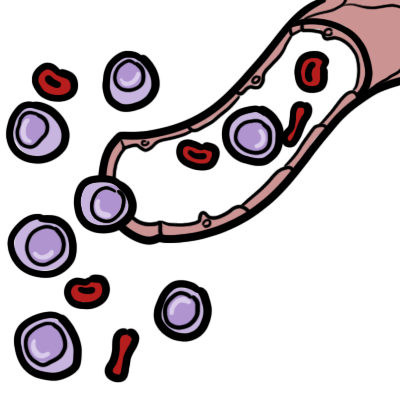
Overview Leukemia is a common malignancy in children and adults that occurs when alterations in normal cell regulatory processes cause uncontrolled proliferation of hematopoietic stem cells in the bone marrow.
| Definitions Leukaemia: Clonal proliferation of hematopoietic stem cells in the bone marrow Acute Leukaemia: Clonal proliferation of hematopoietic stem cells in the bone marrow that develops rapidly, requires immediate treatment and often presents with symptoms. In acute leukaemia the cells in the bone marrow are immature (blasts). Chronic Leukaemia: clonal proliferation of hematopoietic stem cells in the bone marrow that develops slowly, treatment may be delated and often presents asymptomatically. In chronic leukaemia the cells in the bone marrow are still able to mature. Lymphoma: Heterogeneous group of haematological neoplasms, characterised by proliferation of malignantly transformed T or B lymphocytes. The proliferation occur typically in the lymph nodes unlike leukaemia which occir in the bone marrow and result in overcrowding. |
| Watch Video An introduction to Haematopoesis |
Classification
Its important to know that Leukaemia can be divided into acute and chronic and then further divided into its cell lineage. Remember that this makes each of them very different diseases.
- Acute leukaemia
- Acute Myeloid leukaemia (adults)
- Acute Lymphoblastic leukaemia (children)
- Chronic Leukaemia
- Chronic Myeloid leukaemia (adults)
- Chronic Lymphoblastic leukaemia (older adults)
- Myelodysplastic syndromes
- Leukemoid reaction
| Remember Acute lymphoblastic leukemia occurs more often in children, whereas the other subtypes are more common in adults. |
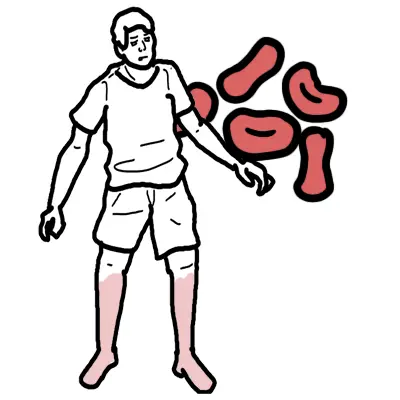
Clinical Presentation
- Acute Leukaemia – pancytopaenia
- Acute Lymphoblastic Leukaemia (more common in children)
- Fever
- Lethargy
- Bleeding
- Hepatomegaly
- Splenomegaly
- Lymphadenopathy
- Bone pain
- Acute Lymphoblastic Leukaemia (more common in children)
| Remember Patients will AML fall ill suddenly and deteriorate fast, because of Infection, Bleeding (low platelets) and Hyperviscosity. |
- Acute Myelogenous Leukaemia
- Constitutional symptoms: Fever, Weight loss, Night sweats
- Anaemia symptoms: Shortness of breath, chest pain
- Thrombocytopaenia symptoms: excessive bruising, nosebleeds, or heavy menstrual periods in women
- Less likely: Bone pain, hepatomegaly and splenomegaly
| Causes of Panytopaenia |
| Bone marrow failure – Aplastic anaemia |
| Drugs |
| Bone marrow infiltration – Lymphoma, leukaemia, myeloproliferative disease, myelodysplastic |
| Hypersplenism |
| SLE |
| Sepsis |
| Alcohol |
| Radiation |
- Chronic Leukaemia – white cell count is high (but nonfunctioning)
- Chronic Lymphoblastic Leukaemia (more common in older adults)
- 50% are asymptomatic
- Hepaosplenomegaly
- Lymphadenopathy
- Chronic Myelogenous Leukaemia
- 20% are asymptomatic
- Splenomegaly
- Chronic Lymphoblastic Leukaemia (more common in older adults)
| SUMMARY OF MAJOR LEUKAEMIA | ||
| Subtype | Description | Typical Group affects |
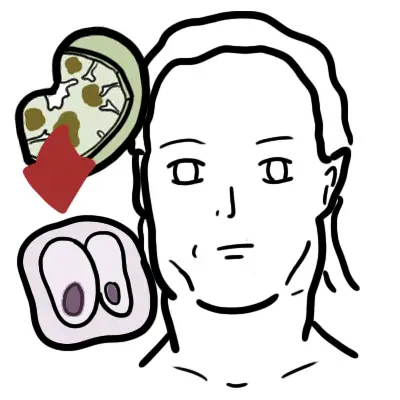
| Acute lymphoblastic leukaemia | Blast cells on peripheral blood smear or bone marrow aspirate | Children (53% <20yo) |
| Acute Myelogenous leukaemia | Blast cells on peripheral blood smear or bone marrow aspirate; Auer rods on peripheral smear | Adults |
| Chronic lymphoblastic leukaemia | Clonal expansion of at least 5,000 B lymphocytes per μL (5.0 × 109 per L) in the peripheral blood | Older adults (85% >65yo) |
| Chronic Myelogenous leukaemia | Philadelphia chromosome (BCR-ABL1fusion gene) | Adults |
Investigations for Leukaemia
- Bone marrow aspirate
- Bone marrow biopsy
- Cytogenetic testing
- Flow cytometry with immunophenotyping
- Molecular testing
- Peripheral smear
Treatment
- A patient with suspected leukemia should be referred to a hematologist-oncologist to confirm the diagnosis and initiate treatment.
- Treatment depends on type of leukaemia
Complications of Leukaemia
- Tumour Lysis Syndrome
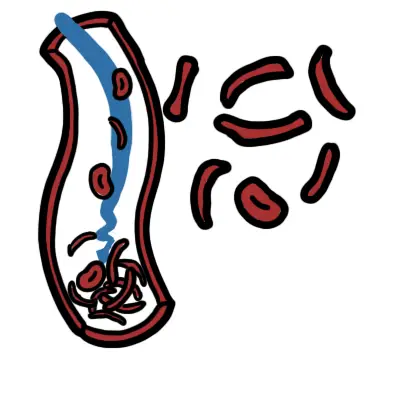
- Disseminated Intravascular Coagulopathy – Widespread activation of coagulation, from release of procoagulants into the circulation with consumption of clotting factors and platelets, with ↑risk of bleeding
- Hyperviscosity
- Death




Discussion