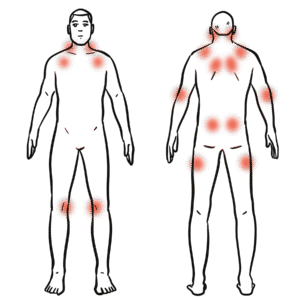
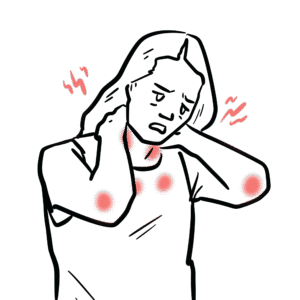
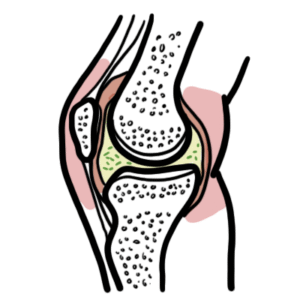
0:00 So this is a video really talking about sacrilege joint pain. 0:13 The sacrilege joints are joints that connect the sacrum, which is the base of 0:17 the spine 0:18 and the isleum, the pelvic bones on each side. 0:22 The main roles of the sacrilege joints is really load transfer from the spine 0:26 to the legs 0:27 and pelvic stability during standing, walking, stair climbing and turning in 0:32 bed. 0:33 Pain arising from this area is called sacrilege joint mediated pain. 0:40 If this is inflammatory, it may be termed sacrilegeitis, as initis is 0:46 inflammation, 0:46 so sacrilegeitis inflammation of the sacrilege joints. 0:55 So how does sacrilege joint pain present? 0:59 Well, it's very frustrating. 1:02 The pain itself can be sudden, chronic and intermittent. 1:08 Sacrilege joint is unique and has characteristic features, so it is important 1:13 to note that sacrilege 1:15 joint pain may also coexist with other lower back pain issues, including facet 1:20 joint arthritis 1:21 or even disc herniation. 1:25 In terms of the sacrilege joint pain itself, the pain itself is deep, 1:30 unilateral buttock 1:32 pain, so on one side, and often infra medial to the posterior superior iliac 1:39 spine, the 1:40 PSIS here. 1:42 The pain also may refer to the posturalateral thigh, so the back and the 1:48 lateral aspect 1:49 of the thigh and occasionally to the groin, but rarely below the knee. 1:54 There are aggravating factors, so obviously single leg stance, so you're 1:58 putting more 1:59 pressure on that, the sacrilege joint on that side. 2:02 So for example, putting on your pants, standing on one leg, walking up and down 2:06 stairs or 2:06 hills, getting in and out of the car, turning in bed, rolling over, prolonged 2:11 standing or 2:12 sitting in one position can also aggravate the pain. 2:16 Facing factors are really short periods of rest, sometimes lying supine with 2:21 knee slightly 2:21 bent, sometimes laying on the unaffected side relieves the pain. 2:29 Red flags to consider that goes against an isolated sacrilege joint pain is 2:35 really dominant 2:36 midline lumbar pain with true, ridiculous symptoms to the foot, so pain going 2:43 down to 2:44 the foot. 2:46 Red flags also include progressive neurological deficits, saddle anesthesia or 2:50 bowel and 2:51 bladder disturbance. 2:53 Lower back pain that is worse with coughing, sneezing or leaning forward is 2:57 more indicative 2:58 of discogenic pain, where the discs of the back are involved and likely 3:08 irritated. 3:10 What are common causes of sacrilege joint pain, well, the most common cause is 3:14 mechanical, 3:15 degenerative, so trauma, falling, twisting injury or lifting. 3:21 Pregnancy and postpartum pelvic girdle pain can also occur due to ligamentous 3:26 laxity, 3:27 when this happens the sacrilege joints become more irritable. 3:31 Leg length discrepancy alter gait, weak gluteal and core musculature causing 3:36 overload, this 3:36 occurs over time. 3:39 Adjacent segment stress after lumbar fusion, as this can also irritate the sac 3:48 rilege joint. 3:50 Sacrilege joint pain can also be caused by inflammatory causes, so it can be 3:54 inflamed 3:55 from autoimmune disease. 3:57 These conditions are the spondyloarthropathy, including ankylosing spondylitis, 4:02 psoriatic 4:02 spondyloarthritis and inflammatory bowel disease, IBD related spondyloarthritis 4:09 . 4:09 Features to suggest an inflammatory sacrilege is quite unique, so in 4:14 inflammatory causes 4:16 of sacrilege joint pain, it's typically chronic back buttock pain at a younger 4:22 age, less than 4:23 40. 4:24 The pain is inflammatory, so it's typically in the morning with associated 4:29 stiffness and 4:31 improves with exercise, and it's not relieved by rest. 4:36 In fact, it gets worse, there's also a night pain, especially the second half 4:40 of the night. 4:43 Features to suggest inflammatory sacrilege is also, if you have a personal or 4:47 family 4:47 history of psoriasis, inflammatory bowel disease, uveitis or HLAB27 positivity. 4:58 Another very rare cause of sacrilege joint pain is infection, this is termed se 5:02 ptic sacrilege 5:04 itis. 5:05 It's typically acute, severe buttock or lower back pain with fever and systemic 5:10 symptoms. 5:10 There are risk factors, so if you're immunosuppressed, IV drug use, postpartum 5:14 state, or have a 5:15 recent infection, or even a procedure to that area. 5:18 I will not talk about this particular cause in more detail. 5:29 So how do you examine someone who you suspect has sacrilege joint pain? 5:33 Well, first of all, it's all about inspection and palpation. 5:36 They may have an ontology gate or altered pelvic alignment. 5:41 There's something called the 14 finger sign, the patient points with one finger 5:46 to an area 5:46 just infromedial to the posterior superior iliac spine as the site of maximal 5:54 pain. 5:55 They can also have local tenderness over the sacrilege joint and surrounding 6:01 ligaments. 6:02 There are provocation tests that can aggravate the symptoms and this can be 6:10 performed as 6:12 a cluster. 6:13 Positive tests really reproduce the familiar buttock sacrilege joint pain not 6:18 just a discomfort. 6:20 These tests include the Faber's test or Patrick's test, the patient essentially 6:24 performs hip 6:25 flexion, abduction, external rotation in a supine position. 6:30 Sacrilege joint or buttock pain suggests sacrilege joint involvement. 6:35 Growing pain suggests a hip pathology in this test. 6:39 Phi thrust test, the hip is flexed 90 degrees, axial force along the femur to 6:45 stress the 6:46 sacrilege joint. 6:48 Then you have the Gaineslens test, so one hip is flexed, other extended off the 6:54 bed, creating 6:55 torsion across a sacrilege joint. 6:57 Then you have the pelvic compression and distraction tests. 7:02 Essentially you're performing lateral compression, patient lying on their side 7:07 and anterior posterior 7:09 distraction where they're supine and you're stressing the sacrilege joint lig 7:14 aments. 7:15 A sacral thrust test is when you perform anterior force and you apply this over 7:21 the 7:21 sacrum with the patient prone. 7:24 This can again cause and irritate the sacrilege joint. 7:29 If you have three or more sacrilege joint provocation tests, this significantly 7:34 increases 7:35 the likelihood that the sacrilege joint is a primary pain generator. 7:45 Then you can obviously perform other examination, screening for differential 7:48 diagnosis. 7:49 So if there's a lumbar spine pathology, you want to assess range of motion. 7:53 You can palpate, there's central or paraspinal tenderness, and also on 7:57 extension in particular 7:58 you can load the facet joints causing pain. 8:02 You want to assess the neurology, so power reflexes sensations, straight leg 8:06 raise, a 8:07 slump test to exclude radiculopathy. 8:11 And you also got to consider if the pain is from the hip joint. 8:14 So you do internal rotation, hip flexion, log roll, vadir favor, fable for 8:19 intraarticulopathology 8:21 such as osteoarthritis or a labral tear of the hip. 8:29 Investigations include really imaging. 8:32 A plain extra of the sacrilege joint is useful to look for chronic sacrilege 8:37 itis. 8:38 This is essentially an autoimmune inflammatory cause. 8:41 You can see sclerosis, erosions, joint space narrowing and ankylosis. 8:46 Here is an example x-ray of someone who has ankylosing spondylitis with chronic 8:50 x-ray 8:51 changes. 8:53 It can be often normal in early or even purely mechanical sacrilege joint pain. 8:59 MRI for sacrilege joint is useful, with stir, fat suppress sequences, and it's 9:04 the modality 9:05 of choice for early inflammatory sacrilegeitis. 9:09 So again, something like ankylosing spondylitis. 9:13 It looks for bone marrow edema, erosions, fat, metaplasia, ankylosis, and also 9:19 surrounding 9:19 soft tissue inflammation. 9:22 A CT scan is better for detailed bony anatomy, for fractures. 9:29 Also chronic structural change, it's less sensitive for early bone marrow edema 9:35 . 9:35 Here is another image example of someone with sacrilegeitis seen in ankylosing 9:40 spondylitis. 9:41 You can see it's nearly fused to sacrilege joints. 9:51 Investigations I've added here is image guided sacrilege joint injection, which 9:55 is a treatment 9:56 option. 9:58 This is through CT or fluoroscopy guided injection of local anesthetic and cort 10:03 icosteroid. 10:04 If they have 75% short-term pain relief, this strongly supports sacrilege joint 10:10 as the dominant 10:11 pain generator. 10:14 Other investigations also include blood work, so laboratory tests when 10:18 indicated. 10:19 So inflammatory markers such as ESR, CRP, blood cultures, if infection is 10:24 suspected. 10:26 HLAB27, autoimmune in GI markers if spondyloarthritis or IBD is suspected. 10:39 Practical approach to management of sacrilege joint pain is really to divide 10:42 into mechanical, 10:43 non-inflammatory sacrilege joint pain or inflammatory like an autoimmune sacri 10:47 lege joint pain. 10:49 So for mechanical, non-inflammatory pain it's really about education, 10:53 explaining the diagnosis, 10:56 reassurance, activity modification, avoid prolonged single leg loading or quid 11:01 lifting. 11:02 Physiotherapy is very important, lumbopelvic stabilization, strengthening glute 11:07 us medius, 11:08 gluteus maximus deep core muscles, correct gait and posture, manual therapy as 11:14 an adjunct. 11:15 Other allied health professionals can also be helpful and have people have 11:19 found benefit, 11:20 this includes chiropractors, massage therapists, analgesia, paracetamol and 11:26 short-term oral 11:27 anti-inflammatories, non-strotal anti-inflammatories are very important. 11:31 Pelvic sacrilege joint belt can be considered particularly in pregnancy, post 11:36 partum, pelvic 11:38 girdle pain. 11:40 Injections I've already talked about, image-guided corticosteroid injections 11:43 for persistent, focal 11:45 sacrilege joint pain, not responding to conservative care. 11:48 Finally, interventional options really rare and really in refractory cases, 11:55 radiofrequency 11:56 ablation, neurotomy of lateral branches supplying the sacrilege joint and sacri 12:01 lege joint fusion 12:03 only after multidisciplinary assessment. 12:11 For inflammatory sacrilege, so this is autoimmune sacrilege, we recommend 12:19 regular non-strotal 12:21 anti-inflammatory drugs if tolerated and a structured exercise program. 12:26 Weight optimization and smoking sensation, there is a role for escalation to bi 12:33 ologic 12:33 or targeted synthetic demands for autoimmune causes of sacrileitis. 12:43 What about prognosis? 12:44 Well, most mechanical sacrilege joint pain improves with the combination of 12:48 education, 12:49 load modification, target physiotherapy and if needed, injection therapy, 12:54 rarely surgeries 12:55 perform. 12:57 The pain may be chronic and intermittent. 13:01 This inflammatory sacrilege is also good with management by a rheumatologist. 13:06 Thank you for watching.