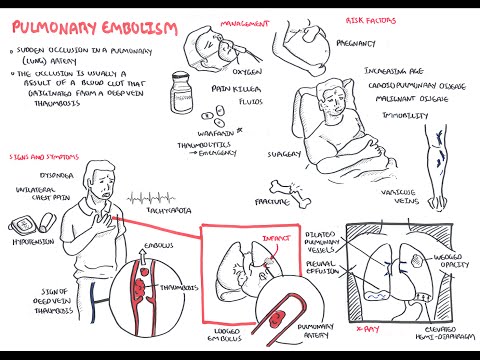
0:00 Okay, so diagnosing or the clinical signs of PE is very difficult to 0:15 differentiate from 0:17 other differentials. 0:20 So what's important when trying to see if a person has PE, it's important to 0:25 look at 0:25 their risk factors, and what has been developed is what's called Well's Crit 0:30 eria. 0:30 This is a modified version, but it's a Well's Criteria is essentially a list of 0:35 factors that 0:37 is given a score, and this will tell you if the patient is more likely to have 0:43 PE or not. 0:45 So these factors include DVT-like symptoms, which will give you a score of 0:51 three. 0:52 Alternative diagnosis less likely than PE will give you a score of three. 0:56 Hot rate greater than 100 will give you a score of 1.5, immobilization more 1:00 than three 1:00 days, or surgery in the previous four weeks will give you 1.5. 1:05 Previous DVT, 1.5, hematosis one, malignancies one. 1:10 And telling this up, you get a total score. 1:13 If your score is greater than four, pulmonary embolism is likely. 1:19 If you have it less or equal to four, pulmonary embolism is unlikely. 1:25 So using the Well's Criteria, the total score of the outcome you get, you use 1:29 that to help 1:30 in your diagnosis. 1:34 So what we will look at next is a diagnosis of PE, using an algorithm. 1:38 But before that, we have to learn more about the D-dimer essay, because it is a 1:43 important 1:44 part, you can say, of diagnosing or ruling out pulmonary embolism. 1:52 So going back to this previous diagram, where a thrombi occurs, remember that, 1:56 you know, 1:57 if fibrinogen becomes fibrin, and you get fibrin, fibrin, fibrin, cross-linking 2:03 , well, 2:03 let us look at this step in a bit more detail. 2:07 So here we have fibrinogen. 2:08 Fibrinogen is such that this yellow pot, it has segments on the outside of 2:12 these white 2:13 things that are called the D-segments. 2:15 Now in the presence of thrombin, which is clotting factor 2A, fibrinogen 2:21 becomes fibrin, 2:22 and these fibrin will essentially link together with their D-segments, it will 2:27 form cross-links 2:29 with their D-segments, so you get a fibrin cross-linking. 2:33 In the presence of plasmin, plasmin breaks down fibrin mesh. 2:38 So basically what the outcome is, you get these D-dimins being formed. 2:42 These D-dimins are essentially this fibrin breaking off, but the D-segments are 2:47 still 2:47 sort of connected with one another. 2:50 And you're measuring essentially this D-dimer in your D-dimer essay, and it 2:56 shows you basically 2:57 your, like, what's happening in your body if you have a coagulation occurring, 3:02 if you 3:02 have clotting occurring. 3:05 So back to the diagnosis algorithm and the Wells Criteria, using the Wells Crit 3:10 eria you 3:10 can either have whole pulmonary embolism unlikely or pulmonary embolism likely. 3:17 We'll begin by looking, if you have pulmonary embolism unlikely, and you do the 3:21 D-dimer 3:21 essay, and you can either get negative or you can get positive. 3:26 If it's negative and it's pulmonary embolism unlikely, then you most likely don 3:31 't have 3:32 PE, so you don't do treatment. 3:34 However, if pulmonary embolism is unlikely and you get a positive D-dimer essay 3:38 , you 3:39 have to do further investigations, which is the CT pulmonary angiogram. 3:45 Similarly, if pulmonary embolism was already likely, you go straight to CT 3:50 pulmonary angiogram. 3:52 After the CT pulmonary angiogram, you can have three outcomes. 3:56 It's either you are negative, positive, or unsure. 4:00 If you're a negative, you probably don't have, the person probably doesn't have 4:04 pulmonary 4:04 embolism, so you don't need to treat it. 4:06 If it's positive, pulmonary embolism is most likely is confirmed, and so you 4:12 begin treatment, 4:13 and treatment can be divided into three things, heparin, IV, low molecular 4:18 weight, heparin, 4:19 which is subcutaneous administration and warfarin, and we'll look into this in 4:23 a bit 4:24 more detail. 4:26 If after the CT pulmonary angiogram, you're unsure, there can be an additional 4:30 test performed 4:31 such as the ventilation perfusion scanning. 4:34 If it's positive, then you can rule in pulmonary embolism, but if it's negative 4:41 , the person 4:42 probably doesn't have PE, so it doesn't need treatment. 4:47 I hope that made sense, this algorithm for helping in the diagnosis of PE. 4:52 Let's look at the treatments. 4:55 Treatments can be divided into three parts, general, anticoagulant, or also 5:00 known as antithrombin, 5:02 ant thrombolytic therapy, thrombolytic therapy is essentially fibrinolysis, and 5:06 we'll talk 5:06 about it a little bit, but we'll go back to step one. 5:11 For general treatment, oxygen, you give oxygen for hypoxemia, you give them 5:17 fluids in case 5:18 of circulatory shock, and you have to avoid diuretics and vasodilators because 5:25 these drugs 5:26 decrease cardiac output and in P, in pulmonary embolism, you usually already 5:31 have a decrease 5:32 in cardiac output, so it's dangerous. 5:36 You can use opioids for pain, but you have to be careful of hypertension. 5:42 Then number two anticoagulants, which is very important, so anticoagulants is 5:46 essentially 5:47 to prevent new blood clots from forming, and it's used for a minimum of three 5:53 months. 5:54 Before introducing these anticoagulants and their mechanism of action, it's 5:58 actually 5:58 important to revise what the coagulation cascade is, just in a simplified 6:04 diagram. 6:05 Here I'm drawing a blood vessel. 6:07 The coagulation cascade can begin either from an intrinsic pathway from inside 6:13 within or 6:13 from an extrinsic pathway when there's a damaged tissue. 6:18 Either way, the intrinsic and extrinsic pathway will lead to a common pathway, 6:24 which will help 6:25 convert clotting factor 10 to 10A. 6:29 10A then will convert prothrombin, which is clotting factor 2 to thrombin, clot 6:35 ting factor 6:36 2A. 6:38 Thrombin, clotting factor 2A will then subsequently convert fibrinogen, and we 6:42 've already talked 6:43 about this, fibrinogen to fibrin, and then the fibrin will form a meshwork of 6:48 fibrin 6:48 and fibrin cross-linking. 6:50 If you remember, in the presence of plasmin, it's broken down, releasing the D- 6:54 dimas. 6:56 The D-dimas is used to basically measure coagulation activity in your blood. 7:04 Your D-dimer is one way of measuring your coagulation activity in circulation, 7:09 but there 7:10 are other ways to measure your coagulation activity in your blood, such as you 7:14 can measure 7:14 your PT and your APTT, which we will talk about in more detail towards the end 7:20 of the 7:21 video. 7:22 But essentially, measuring your PT and your APTT measures your coagulation 7:28 activity. 7:29 Your PT specifically measures your extrinsic pathway and your common pathway 7:35 clotting factors, 7:37 and your APTT measures your intrinsic pathway clotting factors as well as your 7:43 common pathway. 7:45 Measuring your PT and APTT is therefore useful to monitor or to see the effects 7:53 the anticoagulants 7:56 have on the body. 7:57 So let us now move on to the anticoagulants used for pulmonary embolism. 8:03 The two used are heparin and warfarin. 8:07 Usually heparin and warfarin are given together with individuals who have 8:12 pulmonary embolism. 8:14 There are two types of heparin, there's unfraction heparin, which is 8:18 administered intravenously, 8:20 or there is low molecular weight heparin, which is subcut, subcutaneously. 8:26 So the mode of action of heparin is basically that it inhibits their action or 8:30 the production 8:31 of clotting factors 10 and thrombin. 8:34 And so essentially it inhibits the formation of the fibrin meshwork. 8:40 Warfarin on the other hand is taken orally and takes up to five days to have an 8:46 effect. 8:47 And that is why we begin warfarin with heparin in order to wait for warfarin to 8:53 have an effect. 8:55 The mode of action of warfarin is that it is a vitamin K antagonist. 9:00 And therefore it antagonizes the synthesis of the clotting factors 2, 7, 9, and 9:07 10. 9:08 If you live in Australia, this is very, this is kind of easy to remember 9:11 because these 9:12 are the TV channels. 9:14 So 2, 7, 9, and 10. 9:17 So essentially the effects of warfarin is also like heparin in that inhibits 9:21 the formation 9:22 of here, clotting factor 10, and also to thrombin, thus preventing the 9:28 formation of fibrin mesh. 9:32 So we begin the pulmonary embolism patient with heparin and warfarin. 9:37 But then we will discontinue heparin, but keep the patient on warfarin as long 9:43 as the 9:44 INR is okay, as long as the INR is above 2 and below 3. 9:49 Now the INR is another calculation for measuring coagulation activity in the 9:55 body. 9:55 And we will talk about INR in more detail later on. 9:58 But essentially to check the effects of warfarin, the effects warfarin has on 10:02 the body, you 10:03 check the INR. 10:05 For heparin, you check APTT, not PT, sorry this is a mistake. 10:14 So when INR is above 2 and below 3, you can keep the person on warfarin and you 10:19 have to 10:20 monitor this person. 10:23 And they continue warfarin for about 3 months or lifelong if they are at high 10:29 risk of developing 10:31 another thrombus. 10:35 I hope that made sense. 10:37 The third treatment is thrombolytic therapy. 10:40 And thrombolytic therapy is essentially fibrenolitisis. 10:43 So your aim here is to break down the clots. 10:48 You're not preventing new clots from forming, but you're breaking down the cl 10:53 ots already. 10:54 And this is used for acute massive pulmonary embolism and shock because it is 11:05 an emergency. 11:07 So again, going back to the blood test we can use to check for coagulation 11:15 activity in 11:16 the blood. 11:17 We talked about D dimers. 11:18 We talked about INR. 11:20 We talked about protein, we talked about PT and APTT. 11:24 So now let's look at these anticoagulant studies in more detail. 11:28 And I'll talk about four main ones here because these relate to the heparin and 11:32 warfarin that 11:33 I just introduced. 11:37 These four are prothrombin time, the international normalized ratio INR, the 11:43 activated partial 11:44 thromboplastin time, APTT, and the bleeding time. 11:50 So your prothrombin time, your PT, is measuring the activity of your clotting 11:55 factors from 11:56 the extrinsic pathway and your common pathway, which are the clotting factors 12:01 produced by 12:02 the liver and so you're actually assessing the synthetic function of the liver 12:08 or you 12:08 can also use prothrombin time to monitor the effects of warfarin because warfar 12:14 in targets 12:15 the extrinsic pathway and your common pathway as well. 12:21 The international normalized ratio, your INR, is essentially like your PT but 12:25 it's a calculation 12:26 and it's to monitor the effects of warfarin. 12:29 So your extrinsic pathway, clotting factors, and your common pathway. 12:34 The normal INR means that you have normal coagulation. 12:38 A higher INR means that you are less coagulable. 12:42 A normal INR is one, you have normal coagulation. 12:47 A higher INR meaning two or three means that you are less coagulable, you will 12:52 bleed more 12:53 easily. 12:57 The third anticoagulant study is the activated thromboplastin time, partial th 13:01 romboplastin 13:01 time and this is to essentially monitor the effects of IV heparin on coag 13:07 ulation. 13:07 Number four is your bleeding time, which is the time it takes to stop bleeding, 13:11 which 13:12 is I think below 10 minutes is normal or 9 minutes. 13:18 So I hope you enjoyed this video on pulmonary embolism, thank you for watching. 13:27 [BLANK_AUDIO]