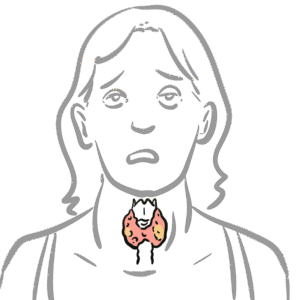
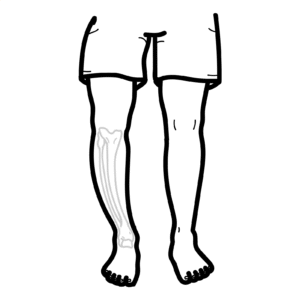
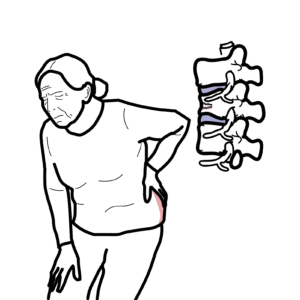
0:00 In this video we're going to look at diabetes myelitis 2, or diabetes type 2. 0:11 Diabetes type 2 is a progressive disorder defined by deficits in insulin 0:16 secretion 0:16 and action. 0:18 What I mean by deficit insulin action is insulin resistance. 0:24 For example, here we have a blood vessel and here a cell with an insulin 0:28 receptor. 0:29 In diabetes type 2 we have a decrease in insulin in the plasma and also insulin 0:35 resistance, 0:36 where the effect of insulin on the cell does not take place. 0:40 As a result of a decrease in insulin secretion and insulin resistance, we get 0:46 hyperglycemia 0:47 or high blood glucose. 0:50 Persistent high blood glucose results in diabetes. 0:54 Before we delve into the signs and symptoms and the pathology, pathophysio-di 0:59 abetes, let 0:59 us learn a bit more about insulin. 1:03 Let us zoom into this area of the abdomen where we can find the pancreas. 1:08 The pancreas is tucked under the stomach and connects to the small intestine. 1:12 The pancreas contains glands and ducts. 1:15 Let us zoom into this area of the pancreas. 1:19 Here I'm drawing the pancreatic ducts and glands. 1:22 These clusters here are known as pancreatic asinine. 1:28 These asinine contains exocrine cells, which release enzymes for digestion, 1:35 which then 1:36 go essentially to the small intestine. 1:41 Around the pancreatic asinine are clusters of cells known as eyelets of lany 1:46 ahan. 1:46 These cells are endocrine cells. 1:50 It is from these cells where the hormone insulin is secreted into the blood. 1:56 Insulin is an important hormone that has many effects on our body. 2:02 The main site insulin target skeletal muscles, liver, and adipose tissue or fat 2:11 . 2:11 In general, the main function of insulin is to store energy. 2:16 In skeletal muscle and adipose tissue, insulin increases glucose uptake and gly 2:23 colysis for 2:24 energy storage. 2:27 Insulin has a big effect on the liver, including increasing glycolysis, 2:32 increasing protein synthesis, 2:35 increasing lipogenesis. 2:38 Insulin also decreases gluconeogenesis, lipolysis, glycogenolysis, and protein 2:45 breakdown. 2:46 All in all, insulin promotes glucose uptake and energy storage, and inhibits 2:54 the release 2:56 of glucose to blood. 2:58 Let us take a closer look at the eyelids of lanyahan, where insulin is produced 3:05 . 3:06 So here are the asinine cells, which are your exocrine cells. 3:12 Next to them, we have islets of lanyahan, which are the cluster of endocrine 3:17 cells which 3:17 produce hormones. 3:20 The majority of endocrine cells within one islets of lanyahan are beta cells, 3:25 which are 3:26 the cells that actually produce insulin as well as amylin. 3:31 There are also other cells here, the alpha cells which produce glucagon and 3:35 delta cells, 3:36 which produce somatostatin. 3:38 It is important to know that glucagon is another hormone that does essentially 3:43 the opposite 3:44 function of insulin. 3:48 Now let us learn a bit more about how and when beta cells release insulin into 3:54 the blood. 3:55 So here I am drawing a beta cell of the pancreas. 4:00 The cell contains mitochondria, and on the cell membrane we find many channels, 4:05 including 4:05 glute2, not for a calcium voltage gated channel and potassium passive channel. 4:16 So let us look at the steps involved in insulin secretion by the beta cells. 4:22 After a meal, there is an increase in blood glucose. 4:25 An increase in blood glucose results in glucose entering the beta cells through 4:29 the glute2 4:30 transporter. 4:32 Glute glucose in the cell is then metabolized through glycolysis and Krebs 4:37 cycle in the cytoplasm 4:38 and the mitochondria, producing many ATP. 4:42 ATP is energy. 4:46 Normally in the beta cell, potassium flows out, creating a negative gradient 4:51 within the 4:52 cell. 4:53 However, the increase in ATP actually inhibits this process. 4:59 To step four, increase in ATP triggers depolarization cascade within the cell, 5:05 resulting in insulin 5:07 release. 5:09 So drawing it out, the increase in cellular potassium causes depolarization, 5:14 resulting 5:15 in opening of calcium voltage gated channels. 5:18 This causes an influx of positively charged calcium. 5:22 The calcium then triggers insulin release via the vesicles. 5:28 When insulin is secreted into the blood, it then targets cells and binds to the 5:33 insulin 5:33 cell receptor, telling the cell to increase the uptake of glucose and to store 5:39 it. 5:40 This is a normal process and results in a decrease in blood glucose level. 5:44 However, in diabetes type 2, this whole process gets messy. 5:49 In diabetes, you do not have enough insulin secretion and you develop insulin 5:54 resistance 5:55 as a result. 5:56 This results in blood glucose staying high. 6:02 Persistent high blood glucose results in the clinical manifestations we see in 6:06 a patient 6:07 who has diabetes. 6:09 A person with diabetes can be asymptomatic for some time. 6:15 But common signs and symptoms include infections, regular infections, fatigue, 6:21 blurred vision, 6:22 and the four P's, parastasia, polydipsia, polyurea, and polyphagea. 6:31 The risk factors for diabetes include older age, obese, having a family history 6:37 , having 6:38 other cardiovascular disease risk factors, gestational diabetes, and polycystic 6:44 ovarian 6:45 syndrome. 6:48 So we learned about the signs and symptoms and the risk factors for diabetes. 6:52 But what happens when diabetes progresses and is untreated? 6:57 As diabetes progresses is undiagnosed or untreated, several complications can 7:03 actually 7:04 occur. 7:05 These can be divided into microvascular and macrovascular complications. 7:11 So microvascular complications include retinopathy, neuropathy, and nephropathy 7:20 . 7:21 Other complications include coronary heart complications, cerebrovascular 7:26 complications, 7:27 and peripheral vascular complications. 7:32 Let's focus on microvascular complications, beginning with retinopathy. 7:37 The eyes of a person with diabetes should be examined regularly. 7:43 Internal changes such as cotton wool spots, micro hemorrhages, microannurisms, 7:48 and macular 7:49 thickening may occur. 7:51 Eye conditions such as glycoma and cataracts can may result. 7:59 Neuropathy complications can be divided into peripheral and autonomic neuro 8:05 pathy. 8:05 Peripheral neuropathy includes a decrease or increase in pain sensation, pain 8:11 less injuries, 8:12 and decrease in reflex. 8:15 Microvascular neuropathy include resting tachycardia, urinary frequency, and 8:19 erectile dysfunction 8:21 in men. 8:24 Nephropathy complications include glomerular sclerosis and pylo nephritis. 8:31 Pylo nephritis is infection of the kidney. 8:36 So that was microvascular complications due to diabetes. 8:40 Now we are looking at the macrovascular complications, which include coronary 8:45 heart complications, 8:47 and this can be chest pain, congestive heart failure, and dyspnea. 8:55 Cerebrovascular complications can result in hemorrhages, cerebral infacts, and 9:00 memory problems. 9:03 Microvascular disease complications include atherosclerosis, gangrene, and ul 9:08 cerations. 9:09 It is very important to have regular foot checks in a patient with diabetes, as 9:15 loss of sensation 9:17 together with a compromised vascular supply can lead to some serious problems 9:22 in the peripheral 9:23 tissue. 9:25 So here is a foot. 9:26 If you have atherosclerosis occurring, gangrene can occur. 9:31 Ocerations can occur, and at times amputations are necessary. 9:38 Ocerations can also occur in the foot of a person. 9:42 Without the person knowing it, common sites are on the sole of the foot, 9:46 commonly around 9:47 where most of the pressure is exerted. 9:55 Now we are going to look at the pathophysiology of these complications that 10:03 occur in diabetes, 10:04 and in order to understand this, we have to look at the vascular changes that 10:08 occurs. 10:09 These vascular changes are essentially what leads to the microvascular and 10:13 macrovascular 10:14 changes we see in diabetes. 10:18 Three things happen in the vessels of patients with diabetes. 10:23 Othroscurosis, arteriosclerosis, and inflammation. 10:28 Othroscurosis, remember, is the plot build-up in the vessel. 10:33 The alteration in vascular homeostasis due to endothelial and smooth muscle 10:38 cell dysfunction 10:39 are the main features of diabetic vascularcy. 10:44 Okay, let us zoom into the layer of the vessel. 10:49 This is the lumen endothelium, tunica intima, and tunica media. 10:55 Tunica media is where the smooth muscle layer is. 10:59 Within the lumen, we have red blood cells and other proteins. 11:03 This is also where glucose, you know, travels. 11:06 In diabetes, we have high blood glucose. 11:09 When there is high blood glucose, the endothelial cells will eventually take 11:15 most of it up. 11:16 The interesting thing here is that the endothelial cells of the vessels do not 11:23 need insulin to 11:24 take up glucose. 11:26 It just does it. 11:28 With so much glucose being taken inside the endothelial cells, the cells 11:32 produce a lot 11:33 of energy and as a by-product reactive oxygen species, or ROS. 11:39 The increase in reactive oxygen species, ROS, leads to a number of things. 11:44 Some formation of advanced glycolated protein products. 11:52 Reactive oxygen species stimulates protein kinase c activity, which sort of 11:58 forms a sort 11:58 of a continuous stimulatory cycle. 12:03 Activation of protein kinase c leads to also a number of things, including 12:08 increased production 12:09 of VEGF and other growth factors, resulting in angiogenesis and cell growth. 12:16 Protein kinase c also increases production of endothelin, which stimulates 12:21 platelet aggregation. 12:24 Protein kinase c also results in increase in nucleophacter capabib within the 12:30 cell. 12:31 Nucleophacter capabib is an inflammatory transcription factor that promotes the 12:35 inflammatory process. 12:37 The end result includes increased expression of receptors for inflammatory 12:43 cells, as well 12:45 as increasing the vascular permeability through produced stimulating cytokine 12:51 production. 12:52 Essentially, the increase in vascular permeability and receptor expression 12:59 allows monocytes 13:01 circulating the blood to pass through the endothelial layer and enter the tun 13:08 ica intima. 13:10 The increase in vascular permeability also allows LDLs to pass through. 13:16 LDLs are low-density lipoproteins. 13:20 So now we have LDLs within the tunica intima, and monocytes. 13:25 The monocytes have become macrophages. 13:29 It has become macrophages as they enter the tissue. 13:35 What happens next is what we see in atherosclerosis. 13:38 The macrophages engulfs the LDL, becoming what is known as a foam cell. 13:44 During this process, the macrophage and foam cell release inflammatory cytok 13:50 ines, such 13:51 as TNF alpha, interleukin 1, which causes further inflammation. 13:58 The foam cells also secrete some growth factors causing smooth muscle 14:03 proliferation and migration 14:04 into the tunica intima. 14:08 The foam cells, which contain a lot of lipids, eventually cluster together and 14:14 rupture within 14:14 the tunica intima. 14:16 The lipids are released, inflammatory cytokines are released, and growth 14:21 factors within the 14:22 foam cells are released when the cell ruptures. 14:25 And this all essentially will create a plaque. 14:30 This whole process we just saw right from the beginning, from reactive oxygen 14:35 species, 14:36 protein kinase C to foam cells, all are what lead to the vascular changes. 14:45 The vascular changes are, you know, there's increase in metabolic toxins. 14:52 The vascular changes are, we see, an increase in metabolic toxins and also athe 15:02 rosclerosis. 15:04 So to summarize the whole process, starting from diabetes, so we have genetics, 15:12 and obesity, 15:13 and other risk factors, increase in age, leads to insulin resistance. 15:21 Insulin resistance leads to the B cell, the beta cell failure. 15:27 The beta cell failure with impaired glucose tolerance leads to insulin 15:34 deficiency. 15:35 Insulin deficiency results in hyperglycemia, or high blood glucose. 15:42 With high blood glucose, the glucose enters the endothelial cells of the 15:46 vessels, resulting 15:47 in the formation of, or stimulating the function of protein kinase C, reactive 15:53 oxygen species, 15:55 AGP, NVEGF, and other growth factors. 16:00 All this causes toxic diabetic metabolism, endothelial dysfunction, and 16:10 vascular inflammation. 16:13 This also leads to atherosclerosis. 16:18 Together, they eventually lead to the microvascular and macrovascular changes 16:24 we see in diabetes, 16:27 which if you remember, microvascular include retinopathy, neuropathy, and neph 16:33 ropathy. 16:34 Microvascular changes include cardiovascular, coronary heart disease, cerebrov 16:40 ascular 16:41 disease, and peripheral vascular complications. 16:46 A note to make is that insulin deficiency can lead to some serious outcomes, 16:51 and these 16:52 include diabetic ketoacidosis, hyperosmolar state, as well as a hyperglycemic 16:58 state. 16:58 Now all these are different, however they're interconnected. 17:02 So diabetic ketoacidosis occurs because insulin doesn't work, and because of 17:07 that, fatty 17:08 acids are broken down, and ketone bodies are released into the blood, 17:14 increasing the acidity 17:15 of the blood. 17:17 In the hyperosmolar state, what happens is that because you have so much 17:21 glucose in the 17:22 blood, it gets urinated out, and thus dragging water with it. 17:30 And this leads to an hyperosmolar state, essentially a dehydrated state. 17:35 And then you have the hyperglycemic state, which is essentially high blood 17:38 glucose levels 17:39 in the blood. 17:41 So I hope you enjoyed this video on diabetes, as well as the pathophysiology of 17:46 the complications 17:47 associated with diabetes. 17:49 Thank you for watching.