Overview
The most common cause of hyperthyroidism are Graves disease, multinodular goitre, an autonomously functioning thyroid nodule (adenoma) and subacute thyroiditis. Graves Disease is more common in women. Multinodular goitre is more common in the elderly. Graves disease typically manifests in middle aged women. Thyroid diseases are more common in women.
| Definition Hyperthyroidism: denote conditions in which hyperfunction of the thyroid leads to thyrotoxicosis. Hypothyroidism: variety of abnormalities that cause insufficient secretion of thyroid hormones. The most common cause is autoimmune thyroid disease Thyrotoxicosis: denotes the clinical, physiological, and biochemical findings that result when the tissues are exposed to excess thyroid hormone. It can arise in a variety of ways (drugs, thyroiditis) |
Anatomy and Physiology
The thyroid gland is butterfly shaped endocrine organ that sits and wraps around the trachea. Anteriorly the thyroid glands are joined by the Isthmus. Developmentally, the thyroid isthmus can give rise to a structure contiguous called the pyramidal lobe, which extends upward.
Posteriorly the thyroid gland does not connect, however 4 parathyroid glands are attached onto the thyroid gland posteriorly.
The gland is in visceral compartment of the neck, along with the trachea, oesophagus and pharynx. The compartment is enclosed in the pre- tracheal fascia, which anchors the thyroid gland to the trachea, so that the thyroid moves up on swallowing.. The thyroid gland stands at the vertebral level C5-T1.
Embryologically, the thyroid gland begins its development at the base of the tongue before descending down to the trachea. This is the reason why thyroid ductal cysts can occur higher up on the neck, anywhere along the path of descent.
Arterial blood supply:
- Superior thyroid artery ← External Carotid
- Inferior thyroid artery ← Thyrocervical trunk
- Ima Artery (~3% of people) ← Brachiocephalic artery
Venous drainage:
- Superior thyroid vein → Internal Jugular
- Middle thyroid vein → Internal Jugular
- Inferior thyroid vein → Brachiocephalic Vein
Physiology The thyroid gland produces 3 hormones:
- Tridothyronine
- Thyroxine
- Calcitonin
Aetiology
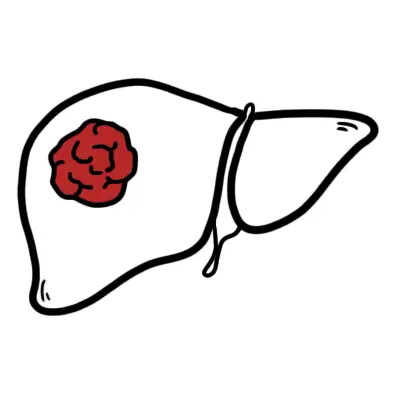
- Graves Disease (most common cause of hyperthyroidism)
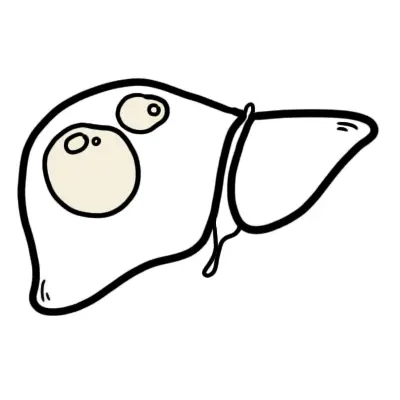
- Multinodular goitre (toxic)
- Thyroid adenoma (toxic)
- Thyroiditis (postpartum, bacterial, postviral, subacute, chronic)
- Exogenous (Amiodarone, Iodine excess, thyroid hormone medication)
- Pituitary adenoma → TSH → Thyroid gland → ↑Thyroid Hormone
| Side note 1/3 of Amiodarone is Iodine and so can cause hyperthyroidism because iodine is an ingredient for thyroid hormone production. |
Pathophysiology
The main cause of hyperthyroidism is graves disease, an autoimmune disease. In Graves disease, autoantibodies are produced that mimic thyroid stimulating hormone resulting in increase thyroid hormone production leading to hyperthyroidism.
Clinical Manifestation
- Hyperactivity, irritability, altered mood, insomnia
- Heat intolerance, sweating
- Palpitations
- Fatigue, weakness
- Dyspnea
- Weight loss with increased appetite (weight gain in 10% of patients)
- Pruritus
- Increased stool frequency
- Thirst and polyuria
- Oligomenorrhea or amenorrhea; loss of libido
Clinical Examination
- General: irritability, axious, weight loss, warm, moist skin, chorea, periodic paralysis (primarily in Asian males), psychosis (rare)
- Hands: onycholysis, fine tremor
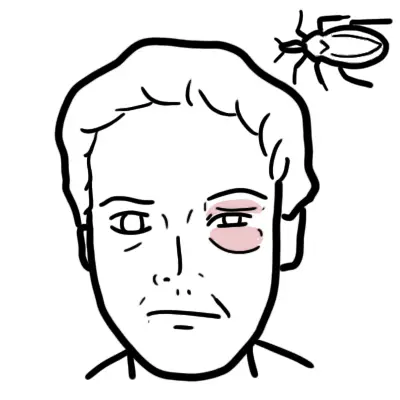
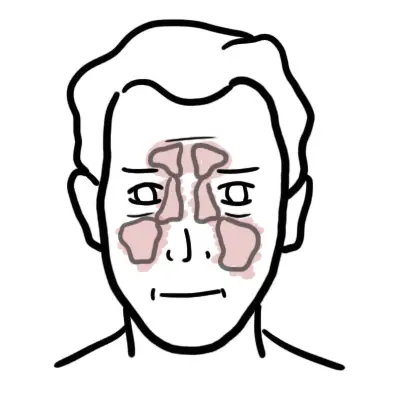
- Face: Hair loss, Graves opthalmology
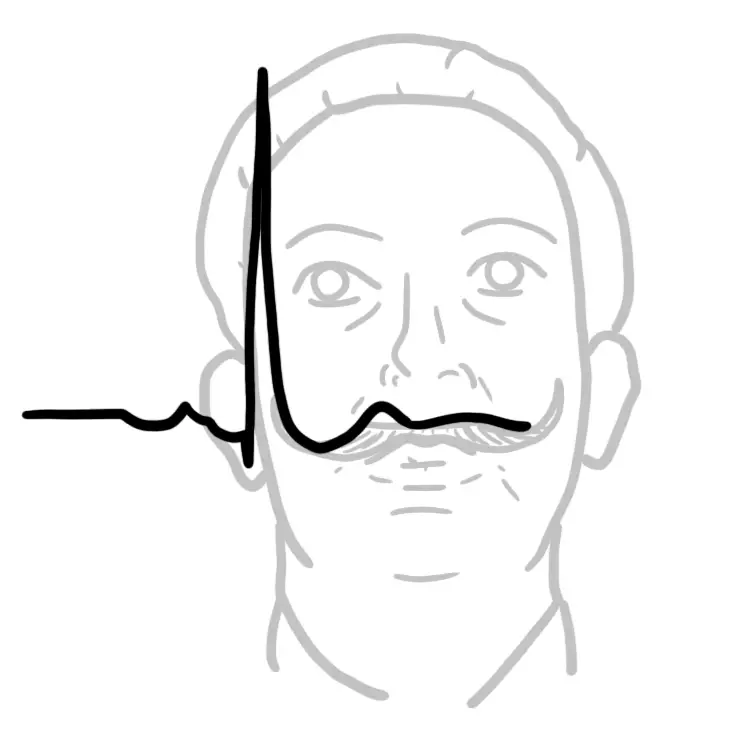
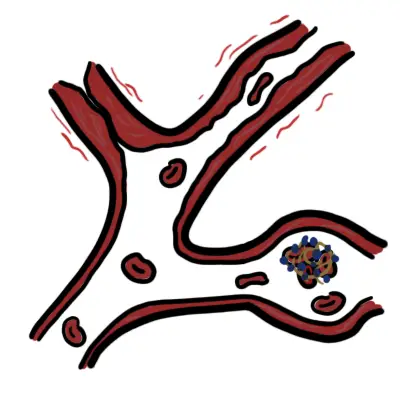
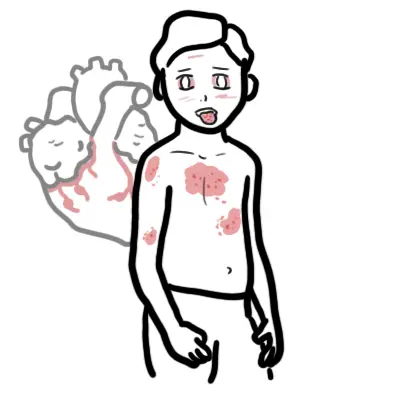
- Cardiovascular: Sinus tachycardia, atrial fibrillation, palmar erythema, congestive (high-output) heart failure,
- Neurological: hyperkinesia, hyperreflexia, muscle weakness and wasting
- Legs: pretibial myxoedema
| Features of Severe Hyperthyroidism |
| Atrial fibrillation |
| Heart Failure |
| Significant weight loss |
| Proximal myopathy |
Graves Disease Additional Manifestation
- Diffuse goiter
- Ophthalmopathy
- Localised dermopathy
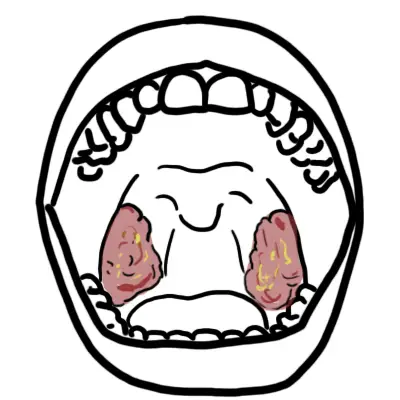
- lymphoid hyperplasia
- Thyroid acropachy

| Conditions associated with Graves Disease |
| Type 1 Diabetes |
| Addison’s Disease |
| Pernicious anaemia |
| Myasthenia Gravis |
| Celiac Disease |
| Vitiligo |
Diagnosis
- Toxic Multinodular Goitre
- Toxic Adenoma
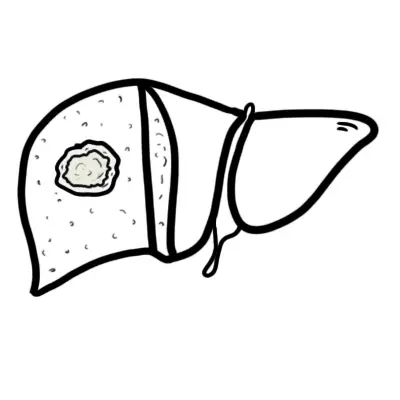
- Thyroiditis (can be painful or painless)
- De Quervain thyroiditis (painful)
- Graves Disease (most common cause of hyperthyroidism)
- Myasthenia Graves – causes opthalmopathy
| De Quervain’s thyroiditis is acute inflammation of the thyroid gland causing spillage of thyroid hormones into blood stream. Presents with ↑T4,T3, ↑ESR and decreased radioactive iodine uptake. |
Investigations
The clinical presentation of hyperthyroidism is diverse. Neither nuclear thyroid scanning not thyroid ultrasound is a mandatory investigation in hyperthyroidism. If hyperthyroidism has been confirmed by biochemical test (TFT), nuclear thyroid scanning should be considered if the thyroid is no palpable, a single thyroid nodule is detected or thyroiditis is suspected. A normal concentration of TSH rules out a diagnosis of hyperthyroidism.
| Grave’s Disease | De Quervain’s thyroiditis (↑ESR) | |
| TFT’s | Increased | Increased |
| Scintiscanning | Increased | Decreased |
| Management | Antithyroid, B-blocker, radioactive iodine, thyroidectomy | Symptomatic treatment because self resolving – b-blocker, steroids. |
Treatment
Medical Treatment aim is to induce remission in Graves’ disease, monitor for relapse of treatment and for patients who relapse to consider other treatment options such as radioiodine or surgery.
- Antithyroid drugs (treat for 18 months and review)
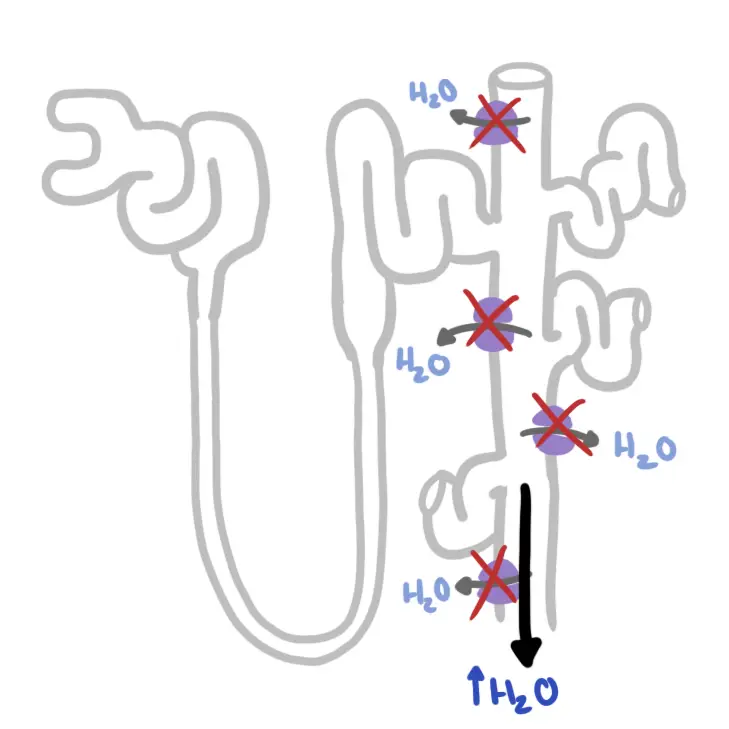
- Thionamides – inhibits thyroid hormone production
- B-blockers – to decrease the sympathetic activity
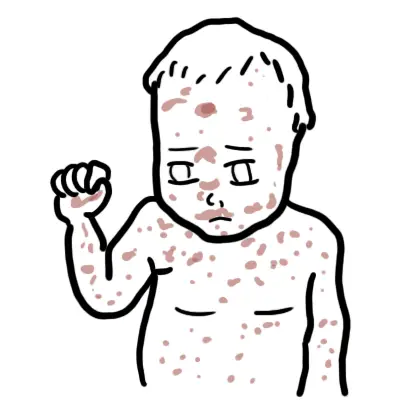
| Pharmacology Thionamides actively accumulates in thyrotoxic tissue and inhibits the action of thyroid peroxidase. Thyroid peroxidase is an enzyme that helps in thyroid hormone synthesis. Agranulocytosis is a life threatening side-effect. Itch and urticarial rash are common side-effects. |
| Remember Treat patient with antithyroid drug for 18months the aim is remission and prevent relapse. If relapse consider radioiodone or surgery. |
- Radioiodine therapy
| Side note Contraindications of radioiodine therapy:Young children, because of the potential risk of thyroid carcinogenesisPregnant and lactating womenSituations where it is clear that the safety of other people cannot be guaranteed. |
Surgical treatment Thyroidectomy is rarely recommended for patients with Graves’ disease
| Indications for thyroidectomy |
| Suspicious or malignant thyroid nodule by FNAC |
| Pregnant mothers who are not adequately controlled by ATD |
| Patient reject or fear exposure to radiation |
| Poor compliance to medical treatment |
| Patients who wants rapid control of symptoms |
Complications
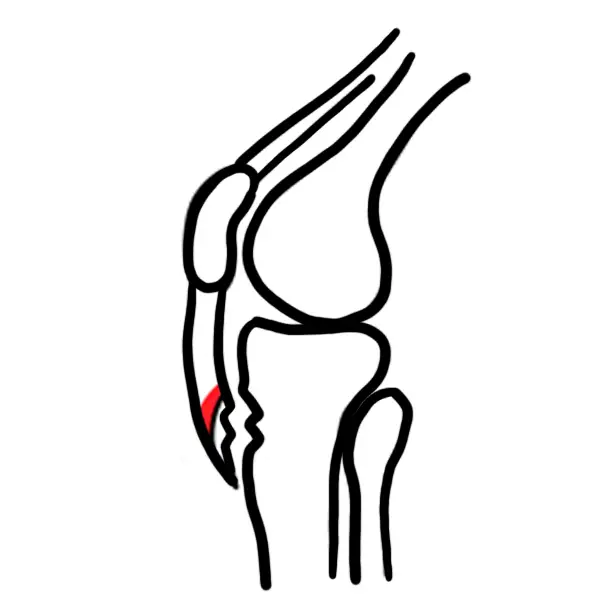
Complications of thyroidectomy
- Recurrent laryngeal nerve damage
- Hypoparathyroidism
- Thyroid crisis
- Local hemorrhage, causing laryngeal edema
- Wound infection
- Hypothyroidism
- Keloid formation
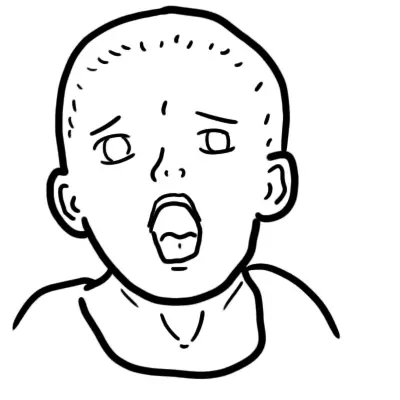
Thyroid Crisis (Storm)
Thyroid crisis represents a rare but life-threatening exacerbation of the manifestations of thyrotoxicosis.
Clinical signs suggestive of a thyroid storm
- Alteration in mental status
- High fever
- Tachycardia or tachyarrhythmias
- Severe clinical signs of hyperthyroidism
- Vomiting, jaundice, and diarrhea
- Multisystem decompensation: cardiac failure, respiratory distress, congestive hepatomegaly, dehydration, and renal failure
Management
- General supportive therapy
- Antiarrhythmic drugs may need to be used – digoxin (watch for Hypokalemia)
- Broad-spectrum antibiotics should be given if infection is suspected.
- Antithyroid drugs in large doses- to inhibit thyroid hormone synthesis completely.
- Potassium iodide 10 drops, twice daily, after starting antithyroid drugs, will inhibit thyroid hormone release.
- B-Adrenergic blocking agents are essential in management to control tachycardia, tremor, and other adrenergic manifestations.
- High doses of glucocorticoids are capable of blocking T4-to-T3conversion