Anal Haemorrhoids
Haemorrhoid Plexi are normal anatomical structures located within the anal canal. The term “Anal Haemorrhoids” usually refers to a pathology where the Haemorrhoidal Plexi are enlarged. They are mainly caused by chronic constipation and frequent defecation leading to dilation and engorgement of haemorrhoidal tissue. Common symptoms are bleeding, pain and itching. There are internal and external haemorrhoids.
Haemorrhoid plexus: venous drainage of the anal canal being at the haemorrhoid plexi. There is an internal and external haemorrhoid plexus. Dilatation of a haemorrhoid plexus causes haemorrhoids.
Anal haemorrhoids: collections of submucosal, fibrovascular, arteriovenous sinusoids that are part of normal anorectum; sometimes referred to as “varicose veins” of the anorectum.
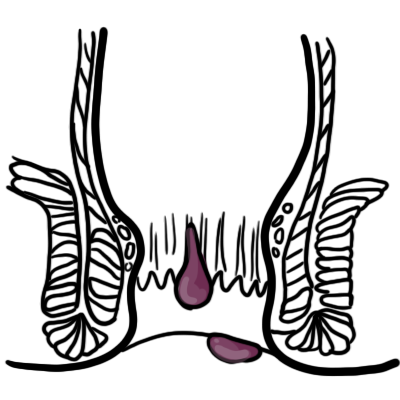
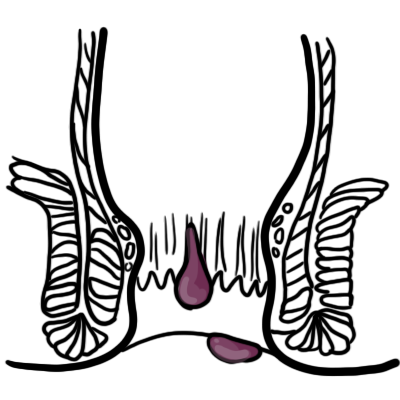
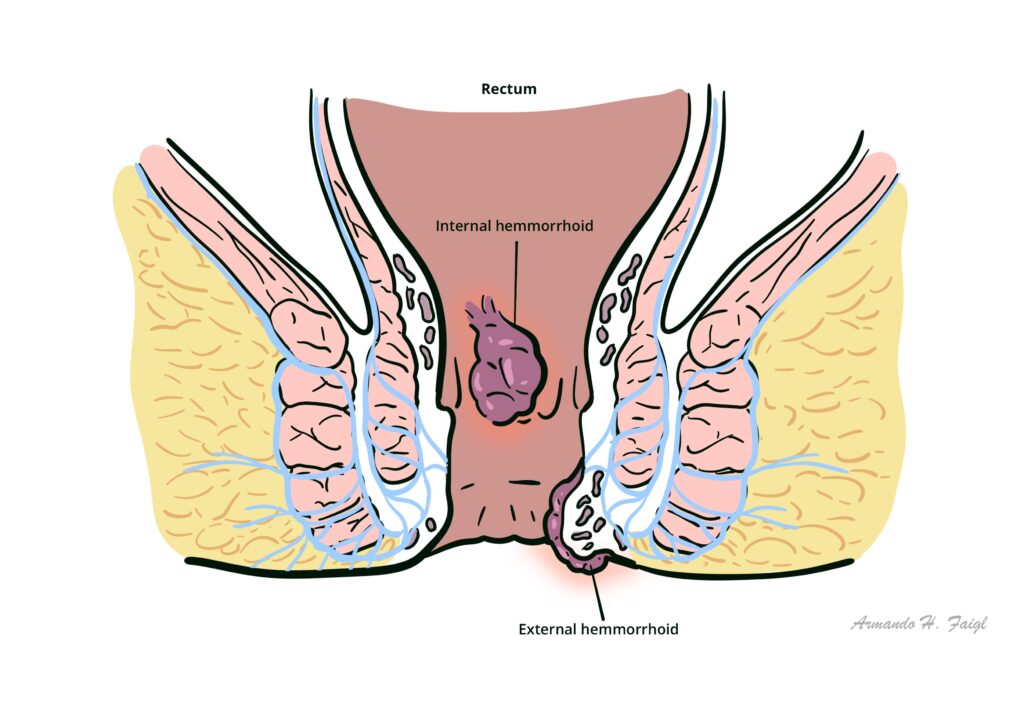
Internal haemorrhoids: originate proximal to the dentate line and are covered by insensate transitional epithelium.
Prolapsed haemorrhoids: severe and painful form of internal haemorrhoids that push through the anus and hang out of the body.
External haemorrhoids: located distal to the dentate line and are covered by sensate anoderm or skin.
Anal cushions – normal vascular cushions at 3, 7 and 11 o’clock positions; composed of venous sinusoids, connective tissue and smooth muscle. Their function is to help with anal continence by contributing to mucosal sealing; haemorrhoids as pathology occur when these cushions enlarge, prolapse and become symptomatic.
Typically haemorrhoids occur in the same location as the main anal blood vessels pedicles (described as 3, 7 and 11 o’clock positions as seen in the supine position).
Anal canal – channel connecting the rectum to the anus, located within the anal triangle of the perineum, between the two ischioanal fossae
Anal Sphincters
Intersphincteric plane
Anal glands
Dentate (pectinate) line
| Distinction | Above Dentate line | Below Dentate line |
| Embryology | Hindgut (endoderm) | Proctodeum (ectoderm) |
| Epithelium | Columnar | Stratified squamous |
| Arterial supply | Superior rectal a. | Middle rectal a.Inferior rectal a. |
| Venous drainage | Superior rectal v. | Middle rectal v.Inferior rectal v. |
| Innervation | Visceral – Inferior hypogastric plexus(insensitive to pain) | Somatic – Inferior rectal nerves: branches of Pudendal nerve(sensitive to pain) |
| Lymph drainage | Internal iliac | Superficial inguinal |
| Haemorrhoids | Internal | External |
Hilton’s Line also called while line/anocutaneous line indicates lower end of the internal sphincter. Ischiorectal abscess when communicating with anal canal usually opens at or below Hilton’s line.
Portal hypertension increases the risk of developing rectal varices, which present similarly to haemorrhoids.
Haemorrhoids are a normal component of the anal canal – they become pathological when they cause symptoms
↓
Increased venous pressure/weakening of supporting structures
↓
Engorgement of haemorrhoidal plexus/displacement of anal cushion
↓
Venous dilation and stasis
↓
Inflammation and oedema
↓
Clinical manifestations (bleeding, prolapse, pain, itching)
External haemorrhoids – below the dentate line; can form thrombus and cause severe pain that usually resolves after 2 weeks.
Internal haemorrhoids – above dentate line; can prolapse out of anal canal.
Although external thrombosed haemorrhoids causes severe pain, the presence of severe pain raises the possibility of other conditions, including anal fissure, perirectal or perivaginal infection, abscess, and other inflammatory processes.
Commonest age of onset is young adulthood.
Approximately 40% of haemorrhoids are asymptomatic.
Anoscopy – most conclusive and specific tests for haemorrhoids
Endoscopic evaluation with colonoscopy or flexible sigmoidoscopy; indicated if:
Labs – FBC (rarely performed): might show iron deficiency anaemia if significant bleeding (indicates endoscopic evaluation)
General treatment (first-line)
Medical treatment
Surgical treatment
Avoid constipation/straining. Exercise, high-fiber diet and drinking plenty of water are good recommendations.
1. Community HealthPathways. Haemorrhoids: Hunter New England; [cited 2025 Sep 20]. Available from: https://hne.communityhealthpathways.org/13803.htm.
2. BMJ Best Practice. Haemorrhoids [updated 27 September 2024; [cited 2025 Sep 20]. Available from: https://bestpractice.bmj.com/topics/en-gb/181.
3. American Society of Colon & Rectal Surgeons. Hemorrhoids [cited 2025 Sep 20]. https://fascrs.org/patients/diseases-and-conditions/a-z/hemorrhoids
4. healthdirect. Haemorrhoids [cited 2025 Sep 20]. Available from: https://www.healthdirect.gov.au/haemorrhoids-piles.
5. GP Exams. Haemorrhoids [cited 2025 Sep 20]. Available from: https://gpexams.com/haemorrhoids/.
6. Bleday R, Breen E. Hemorrhoids: Clinical manifestations and diagnosis [updated 2025 Sep 11; cited 2025 Sep 20]. Available from: https://www-uptodate-com.ezproxy.newcastle.edu.au/contents/hemorrhoids-clinical-manifestations-and-diagnosis.

Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.
Discussion